Sunday Poster Session
Category: Liver
P1655 - Differential Impact of the COVID-19 Pandemic on Post-Liver Transplant Survival by Etiology: A Retrospective Analysis of UNOS STAR Data (2016–2025)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abhijith K. Atkuru, MD
Tulane University School of Medicine
New Orleans, LA
Presenting Author(s)
Abhijith K. Atkuru, MD1, Chandler Gilliard, MD, BS1, Luis A.. Morales, MD, MS2, Jacob Lampenfeld, MD3, Peng-Sheng Ting, MD3
1Tulane University School of Medicine, New Orleans, LA; 2Tulane University, New Orleans, LA; 3Tulane School of Medicine, New Orleans, LA
Introduction: COVID-19 disrupted liver transplant (LT) trends, with alcohol-associated liver disease (ALD) becoming the leading indication. The long-term survival impact of these shifts remains poorly defined. This study examined patient and graft survival after LT across etiologies (ALD, Hepatitis C Virus [HCV], Metabolic-Associated Steatotic Liver Disease [MASLD], Other) during the pre-pandemic (2016–Feb 2020), COVID era (Apr 2020–Dec 2022), and post-COVID (2023–Apr 2025) periods.
Methods: We analyzed adult (≥18 years old), first-time, deceased donor LT recipients from the UNOS STAR database. Patient survival (n=70,523; 10,691 deaths) and graft survival (n=70,523; 11,940 failures) were modeled using Cox regression stratified by diagnosis × era. Time-dependent interactions were modeled using tt() in R. Covariates included recipient and donor age, sex, MELD at transplant, recipient citizenship, hepatocellular carcinoma (HCC), donor HCV/HBV/HIV serologies, circulatory/brain death donation (DCD/DBD), and cold ischemia time (CIT). Ethnicity was evaluated in a secondary proportional hazards (PH) model. PH assumptions were evaluated using cox.zph in R. Kaplan-Meier (KM) curves compared 90-day graft survival across eras.
Results: Patient survival improved for ALD in the COVID-era (aHR 0.92; 95% CI 0.87–0.98; p=0.008) but worsened for MASLD (1.23; 1.15–1.32; p< 0.001), Other (1.14; 1.06–1.23; p< 0.001), and HCV (1.10; 1.00–1.21; p=0.046). Key time-dependent effects were observed for survival: MELD score increased early mortality risk, diminishing over time (tt p=0.005); male sex and HCC were protective early but were associated with increased mortality later (tt p< 0.001). For graft survival, DCD donor status (aHR 1.18, p< 0.001) and CIT (aHR 1.05; p< 0.001) were consistently associated with graft failure. In a secondary model, Black recipients had higher graft failure risk (aHR 1.27; 95% CI 1.19-1.36) and Asian recipients had lower risk (aHR 0.76; 0.64-0.90). One-year graft survival was similar across the eras (Kaplan-Meier log-rank p=0.19) when restricted to patients with adequate follow-up.
Discussion: COVID-era post-LT survival showed dynamic, time-varying changes, notably for ALD, HCC, and MELD. Racial disparities were most pronounced in worse outcomes for Black transplant recipients. Our findings highlight disparities in transplant outcomes by etiology and race that may benefit from focused attention on those at risk of graft failure.
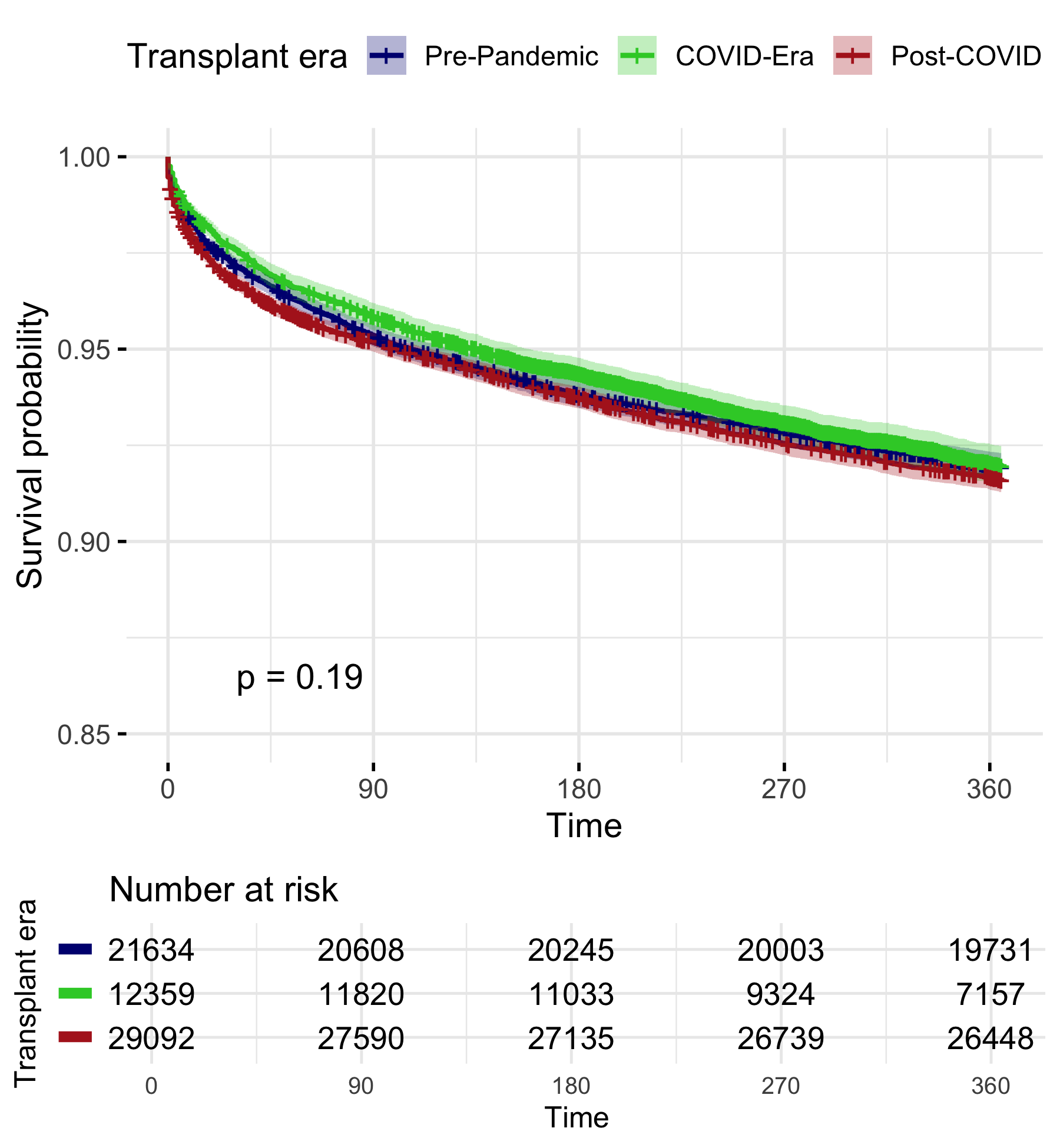
Figure: Time-varying hazard ratios for graft failure in liver transplant recipients. A: MELD score (per point increase). B: Male versus female sex. C: Cold ischemia time (per hour). Hazard ratios estimated using Cox regression with time-dependent covariates over 3 years post-transplant.
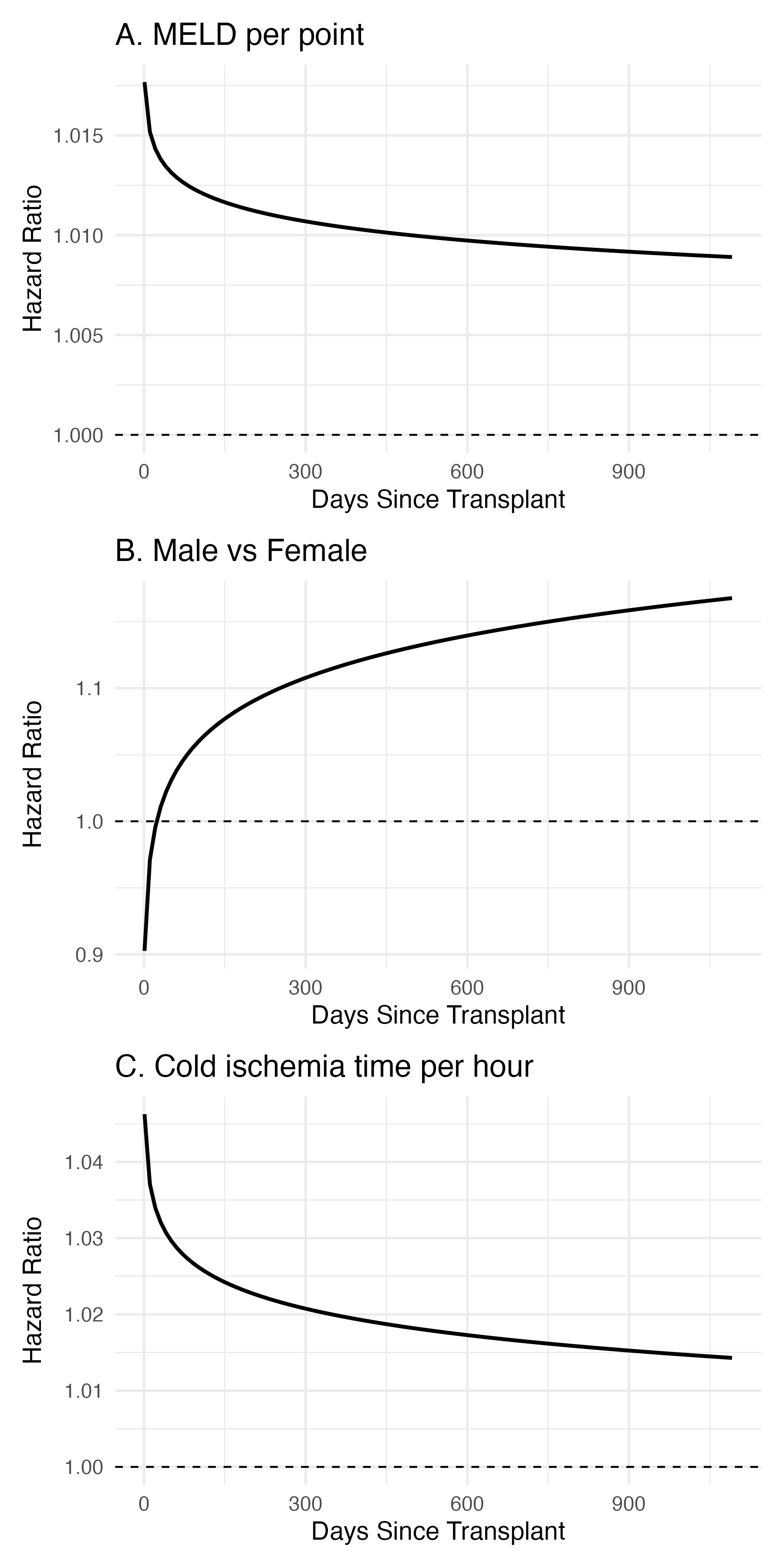
Figure: Unadjusted Kaplan-Meier curves for 1-year graft survival in adult, first-time, deceased donor liver transplant (LT) recipients, stratified by pandemic era: Pre-Pandemic (initial N=29,092), COVID-Era (initial N=21,634), and Post-COVID (initial N=12,359). No statistically significant difference was observed among eras (log-rank p=0.19). Shaded areas indicate 95% confidence intervals.
Disclosures:
Abhijith Atkuru indicated no relevant financial relationships.
Chandler Gilliard indicated no relevant financial relationships.
Luis Morales indicated no relevant financial relationships.
Jacob Lampenfeld indicated no relevant financial relationships.
Peng-Sheng Ting indicated no relevant financial relationships.
Abhijith K. Atkuru, MD1, Chandler Gilliard, MD, BS1, Luis A.. Morales, MD, MS2, Jacob Lampenfeld, MD3, Peng-Sheng Ting, MD3. P1655 - Differential Impact of the COVID-19 Pandemic on Post-Liver Transplant Survival by Etiology: A Retrospective Analysis of UNOS STAR Data (2016–2025), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tulane University School of Medicine, New Orleans, LA; 2Tulane University, New Orleans, LA; 3Tulane School of Medicine, New Orleans, LA
Introduction: COVID-19 disrupted liver transplant (LT) trends, with alcohol-associated liver disease (ALD) becoming the leading indication. The long-term survival impact of these shifts remains poorly defined. This study examined patient and graft survival after LT across etiologies (ALD, Hepatitis C Virus [HCV], Metabolic-Associated Steatotic Liver Disease [MASLD], Other) during the pre-pandemic (2016–Feb 2020), COVID era (Apr 2020–Dec 2022), and post-COVID (2023–Apr 2025) periods.
Methods: We analyzed adult (≥18 years old), first-time, deceased donor LT recipients from the UNOS STAR database. Patient survival (n=70,523; 10,691 deaths) and graft survival (n=70,523; 11,940 failures) were modeled using Cox regression stratified by diagnosis × era. Time-dependent interactions were modeled using tt() in R. Covariates included recipient and donor age, sex, MELD at transplant, recipient citizenship, hepatocellular carcinoma (HCC), donor HCV/HBV/HIV serologies, circulatory/brain death donation (DCD/DBD), and cold ischemia time (CIT). Ethnicity was evaluated in a secondary proportional hazards (PH) model. PH assumptions were evaluated using cox.zph in R. Kaplan-Meier (KM) curves compared 90-day graft survival across eras.
Results: Patient survival improved for ALD in the COVID-era (aHR 0.92; 95% CI 0.87–0.98; p=0.008) but worsened for MASLD (1.23; 1.15–1.32; p< 0.001), Other (1.14; 1.06–1.23; p< 0.001), and HCV (1.10; 1.00–1.21; p=0.046). Key time-dependent effects were observed for survival: MELD score increased early mortality risk, diminishing over time (tt p=0.005); male sex and HCC were protective early but were associated with increased mortality later (tt p< 0.001). For graft survival, DCD donor status (aHR 1.18, p< 0.001) and CIT (aHR 1.05; p< 0.001) were consistently associated with graft failure. In a secondary model, Black recipients had higher graft failure risk (aHR 1.27; 95% CI 1.19-1.36) and Asian recipients had lower risk (aHR 0.76; 0.64-0.90). One-year graft survival was similar across the eras (Kaplan-Meier log-rank p=0.19) when restricted to patients with adequate follow-up.
Discussion: COVID-era post-LT survival showed dynamic, time-varying changes, notably for ALD, HCC, and MELD. Racial disparities were most pronounced in worse outcomes for Black transplant recipients. Our findings highlight disparities in transplant outcomes by etiology and race that may benefit from focused attention on those at risk of graft failure.
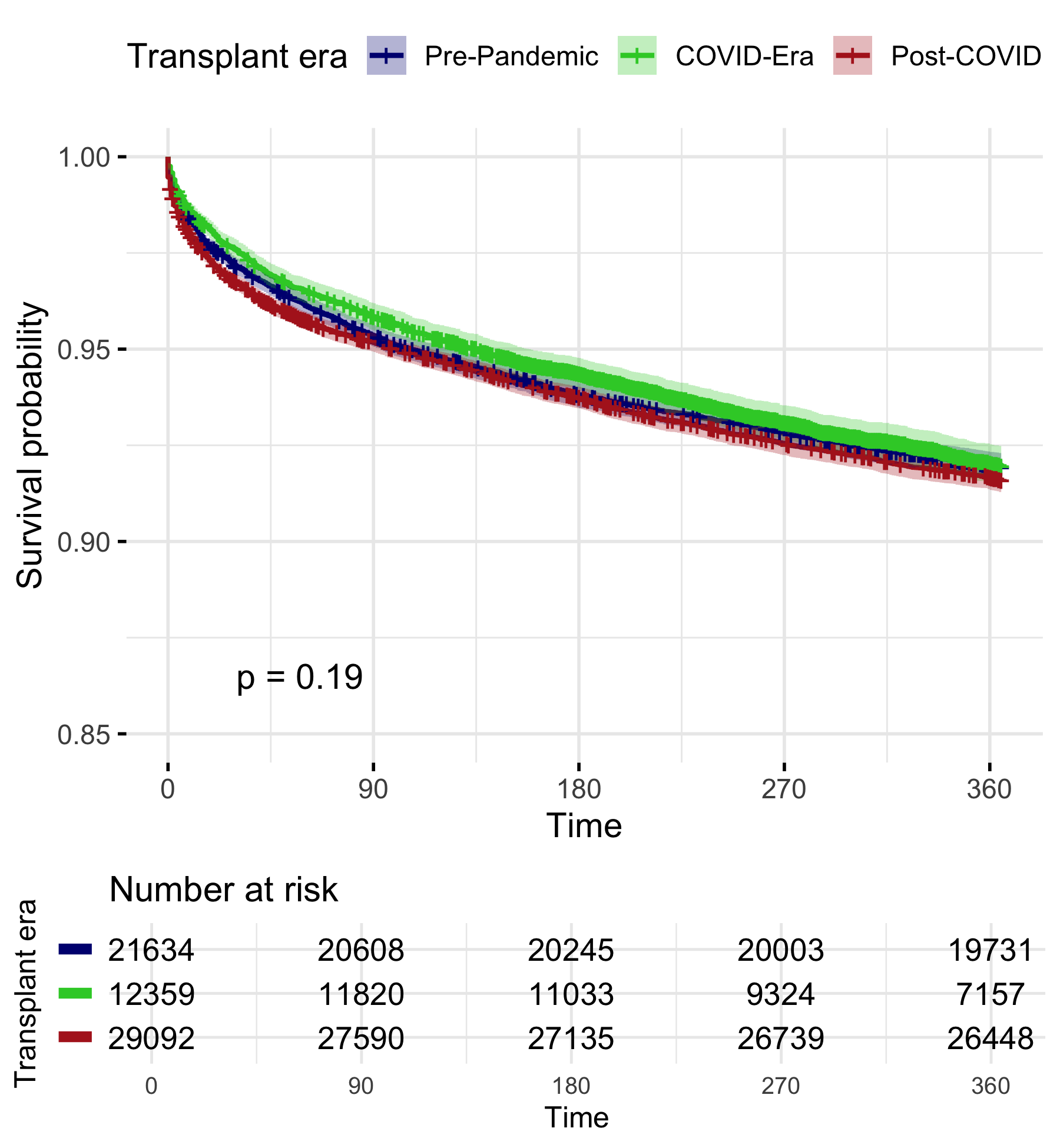
Figure: Time-varying hazard ratios for graft failure in liver transplant recipients. A: MELD score (per point increase). B: Male versus female sex. C: Cold ischemia time (per hour). Hazard ratios estimated using Cox regression with time-dependent covariates over 3 years post-transplant.
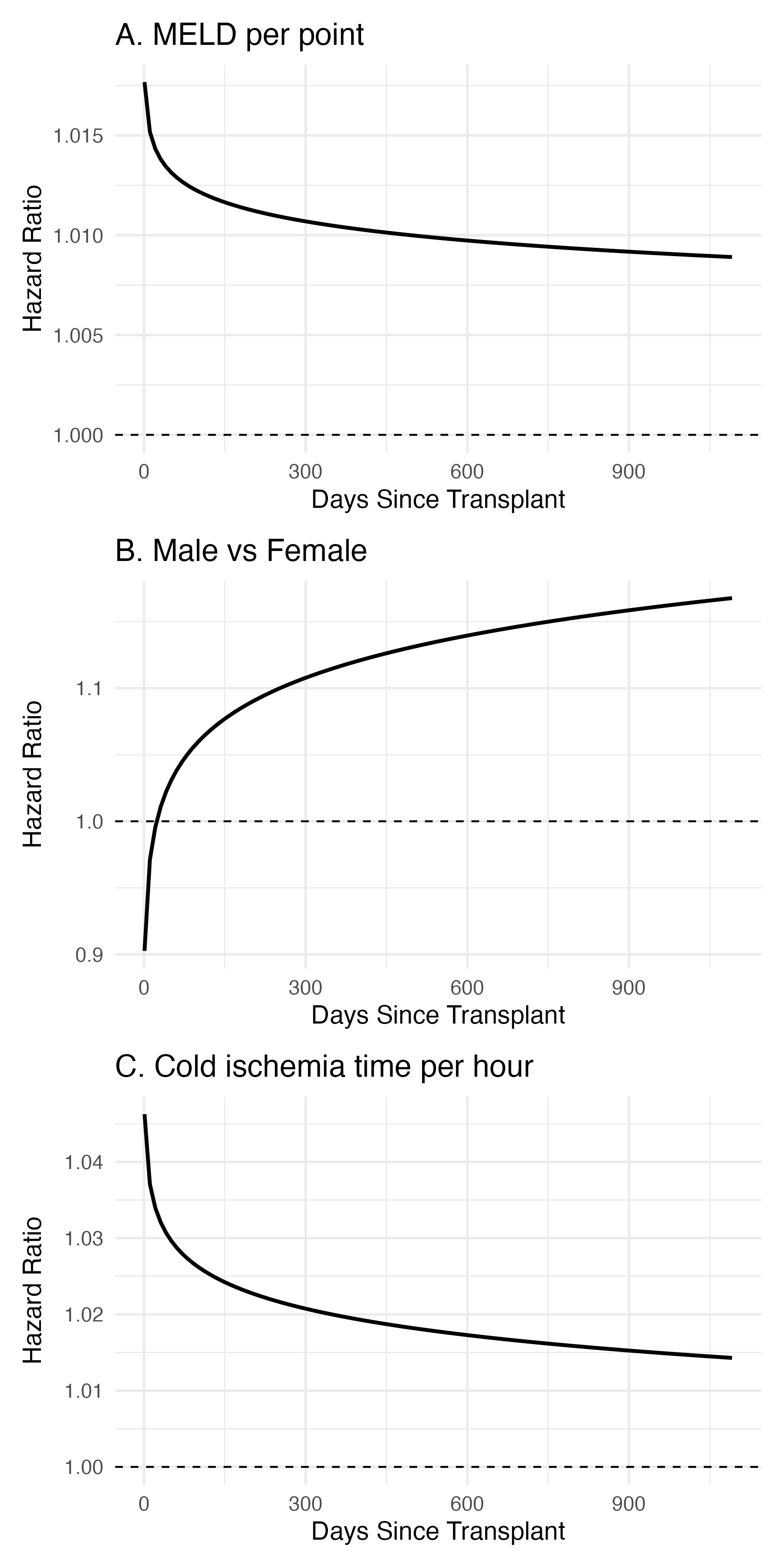
Figure: Unadjusted Kaplan-Meier curves for 1-year graft survival in adult, first-time, deceased donor liver transplant (LT) recipients, stratified by pandemic era: Pre-Pandemic (initial N=29,092), COVID-Era (initial N=21,634), and Post-COVID (initial N=12,359). No statistically significant difference was observed among eras (log-rank p=0.19). Shaded areas indicate 95% confidence intervals.
Disclosures:
Abhijith Atkuru indicated no relevant financial relationships.
Chandler Gilliard indicated no relevant financial relationships.
Luis Morales indicated no relevant financial relationships.
Jacob Lampenfeld indicated no relevant financial relationships.
Peng-Sheng Ting indicated no relevant financial relationships.
Abhijith K. Atkuru, MD1, Chandler Gilliard, MD, BS1, Luis A.. Morales, MD, MS2, Jacob Lampenfeld, MD3, Peng-Sheng Ting, MD3. P1655 - Differential Impact of the COVID-19 Pandemic on Post-Liver Transplant Survival by Etiology: A Retrospective Analysis of UNOS STAR Data (2016–2025), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

