Sunday Poster Session
Category: Liver
P1620 - Bridging the Procedural Gap: A Quality Improvement Initiative Targeting Resident Involvement and Time-to-Paracentesis at a Tertiary Academic Center
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SP
Samuel C. Purkey, DO
Allegheny Health Network
Knoxville, TN
Presenting Author(s)
Samuel C.. Purkey, DO1, Helene Bloom, DO2, Jonathan Ghobrial, MD3, Dash Chandan, MD4, Marissa Gorvet, DO2, Michael Babich, MD4
1Allegheny Health Network, Knoxville, TN; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA; 3Allegheny Health Network, Cleveland, OH; 4Allegheny Health Network, Pittsburgh, PA
Introduction: Timely paracentesis (≤ 24 h from admission) improves diagnostic yield and outcomes in decompensated cirrhosis, yet bedside opportunities for internal-medicine (IM) residents have declined. We performed a baseline assessment to launch a QI project whose SMART aim is to raise the proportion of in-patients receiving paracentesis within 24 h from 55 % to 90 % and double resident involvement by June 2027.
Methods: At an ACGME-accredited tertiary center we:
Results: Survey (21 responses): Only 2 (9.5 %) residents that completed the survey had ever performed paracentesis; 19 (90.5 %) felt uncomfortable, 18 (85.7 %) wanted more training, and 16 (76.2 %) perceived delays.
Chart review (72 evaluable admissions): Mean time-to-paracentesis = 55.6 ± 94.7 h (median 20.9; 39 % > 24 h; no complications). Proceduralists: APPs 50 %, critical-care fellows 22 %, residents 19 %, radiologists 7 %, and internists 1 %. Location: radiology 68 %, ICU/ED 32 %, medicine ward 0%. Procedure location independently predicted longer delay (β = +0.28 log-hours ≈ 1.9-fold, p = 0.010) after adjustment for provider type and medication with radiology-based procedures showing greater delays; provider type trended toward significance (p = 0.086).
Discussion: IM residents should feel comfortable with bedside procedure but rarely perform paracentesis. Over one-third of patients miss the 24-hour benchmark, largely because cases are routed to radiology. Our findings support the need for structured procedural education, including supervised bedside paracentesis during residency. Interventions include dedicated didactic time, protected procedural rotations, bedside teaching, and simulation-based training. Empowering residents to perform procedures will help achieve our SMART aim and could cut mean delay by ≥ 35 h, enhance resident competence, and potentially shorten length of stay without added risk.
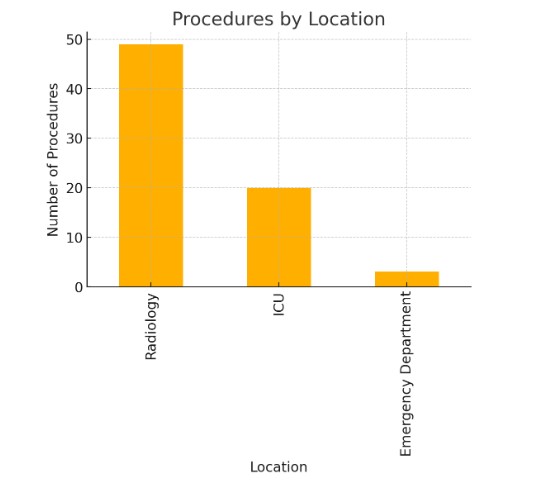
Figure: Location of paracenteses being completed at a tertiary academic medical center
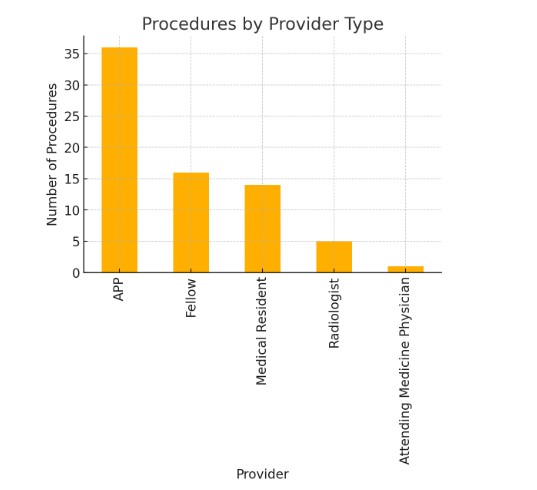
Figure: Comparison of the proceduralist completing paracenteses at a tertiary academic medical center
Disclosures:
Samuel Purkey indicated no relevant financial relationships.
Helene Bloom indicated no relevant financial relationships.
Jonathan Ghobrial indicated no relevant financial relationships.
Dash Chandan indicated no relevant financial relationships.
Marissa Gorvet indicated no relevant financial relationships.
Michael Babich indicated no relevant financial relationships.
Samuel C.. Purkey, DO1, Helene Bloom, DO2, Jonathan Ghobrial, MD3, Dash Chandan, MD4, Marissa Gorvet, DO2, Michael Babich, MD4. P1620 - Bridging the Procedural Gap: A Quality Improvement Initiative Targeting Resident Involvement and Time-to-Paracentesis at a Tertiary Academic Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network, Knoxville, TN; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA; 3Allegheny Health Network, Cleveland, OH; 4Allegheny Health Network, Pittsburgh, PA
Introduction: Timely paracentesis (≤ 24 h from admission) improves diagnostic yield and outcomes in decompensated cirrhosis, yet bedside opportunities for internal-medicine (IM) residents have declined. We performed a baseline assessment to launch a QI project whose SMART aim is to raise the proportion of in-patients receiving paracentesis within 24 h from 55 % to 90 % and double resident involvement by June 2027.
Methods: At an ACGME-accredited tertiary center we:
- Administered an anonymous 7-item electronic survey to PGY-1–3 IM residents (experience, comfort, perceived delays, training needs).
- Conducted a retrospective review of adult admissions undergoing paracentesis (July 2022 – December 2024).
Primary outcome = hours from admission to procedure; covariates = provider type, location, medication use, and laboratory values. Descriptive statistics were used to summarize the timing and characteristics of the procedures and predictors were analyzed with ANOVA and multivariable linear regression of log-transformed time.
Results: Survey (21 responses): Only 2 (9.5 %) residents that completed the survey had ever performed paracentesis; 19 (90.5 %) felt uncomfortable, 18 (85.7 %) wanted more training, and 16 (76.2 %) perceived delays.
Chart review (72 evaluable admissions): Mean time-to-paracentesis = 55.6 ± 94.7 h (median 20.9; 39 % > 24 h; no complications). Proceduralists: APPs 50 %, critical-care fellows 22 %, residents 19 %, radiologists 7 %, and internists 1 %. Location: radiology 68 %, ICU/ED 32 %, medicine ward 0%. Procedure location independently predicted longer delay (β = +0.28 log-hours ≈ 1.9-fold, p = 0.010) after adjustment for provider type and medication with radiology-based procedures showing greater delays; provider type trended toward significance (p = 0.086).
Discussion: IM residents should feel comfortable with bedside procedure but rarely perform paracentesis. Over one-third of patients miss the 24-hour benchmark, largely because cases are routed to radiology. Our findings support the need for structured procedural education, including supervised bedside paracentesis during residency. Interventions include dedicated didactic time, protected procedural rotations, bedside teaching, and simulation-based training. Empowering residents to perform procedures will help achieve our SMART aim and could cut mean delay by ≥ 35 h, enhance resident competence, and potentially shorten length of stay without added risk.
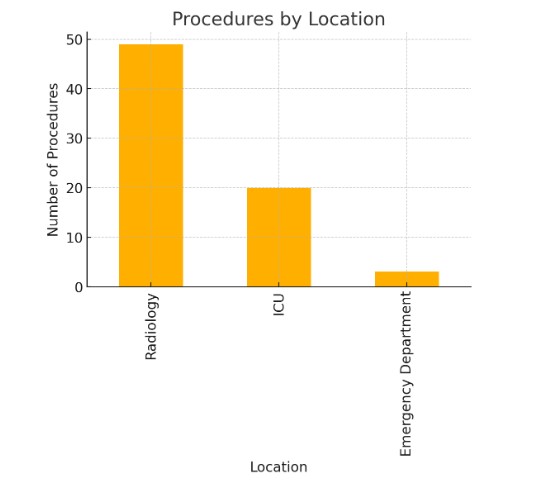
Figure: Location of paracenteses being completed at a tertiary academic medical center
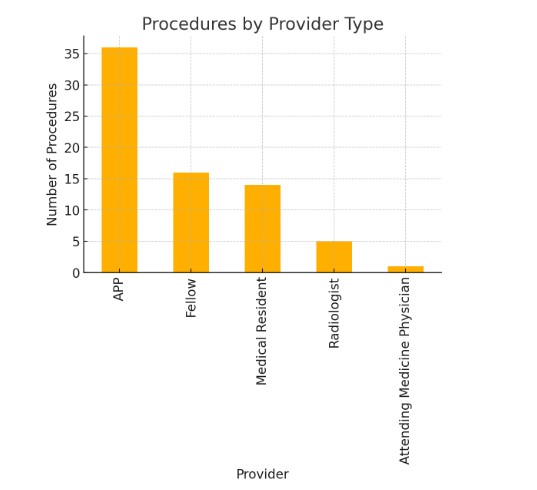
Figure: Comparison of the proceduralist completing paracenteses at a tertiary academic medical center
Disclosures:
Samuel Purkey indicated no relevant financial relationships.
Helene Bloom indicated no relevant financial relationships.
Jonathan Ghobrial indicated no relevant financial relationships.
Dash Chandan indicated no relevant financial relationships.
Marissa Gorvet indicated no relevant financial relationships.
Michael Babich indicated no relevant financial relationships.
Samuel C.. Purkey, DO1, Helene Bloom, DO2, Jonathan Ghobrial, MD3, Dash Chandan, MD4, Marissa Gorvet, DO2, Michael Babich, MD4. P1620 - Bridging the Procedural Gap: A Quality Improvement Initiative Targeting Resident Involvement and Time-to-Paracentesis at a Tertiary Academic Center, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
