Sunday Poster Session
Category: Liver
P1616 - A Quality Improvement Study to Increase Diagnostic Paracentesis for Admitted Veterans With Ascites
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Chung-Heng Liu, MD (he/him/his)
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Chung-Heng Liu, MD, Gabriel Monti, MD, Quinn Nelson, MD, Michael Chang, MD
Oregon Health & Science University, Portland, OR
Introduction: Multiple society guidelines recommend diagnostic paracentesis in all patients admitted to the hospital with cirrhosis and ascites. However, one multi-center study conducted at Veteran Administration (VA) medical centers demonstrated < 15% of patients received early paracentesis (EP) within 24h of initial presentation. The aim of this quality improvement (QI) study is to evaluate whether an educational intervention can improve the frequency of timely diagnostic paracentesis.
Methods: This QI study was based on a 90-minute simulation-based educational session for all internal medicine trainees rotating at our VA inpatient service for each 3-week rotation started on January 13, 2025. The simulation utilized a mannequin and all the supplied necessary to perform a paracentesis at our facility. Furthermore, education regarding the indication for paracentesis was provided to all attendees.
Outcomes were analyzed using statistical process control C chart of these data for both outcomes. Special cause variation was noted by the presence of a data point outside the upper control limit. Veterans were also divided into 2 cohorts, pre-intervention (October 2024 to December 2024) and post-intervention (January 2025 to April 2025).
Results: 132 Veterans (96.8% male and median age 72 years) with liver cirrhosis were admitted from October 1, 2024 – April 14, 2025. 28% of the cohort (N=37) had ascites present on admission. Amongst those with ascites, 20 (54%) and 14 (38%) Veterans had a diagnostic paracentesis at any point during their admission and EP, respectively. Special cause variation is noted in those undergoing diagnostic paracentesis after the educational intervention (Figure 1). A similar relationship was not observed for Veterans who received EP. There is no significant difference in proportion of paracentesis between the pre- and post- intervention cohorts (Figure 2).
Discussion: Early data from this QI study suggest that implementation of a structured educational simulation for internal medicine trainees increased the frequency of diagnostic paracentesis for Veterans with cirrhosis and ascites admitted to the hospital by means of special cause variation on a C chart. Aggregate comparisons of the pre and post intervention cohorts failed to show a statistically significant improvement, likely due to small sample size. Ongoing efforts aimed at both trainees and attending hospitalists are underway.
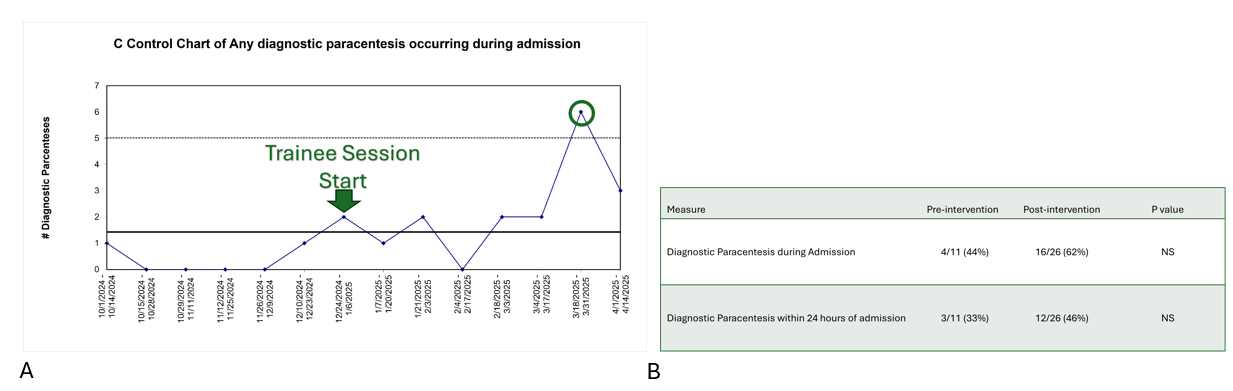
Figure: (A) Statistical process control C chart of any diagnostic paracentesis during admissions; (B) Table comparing aggregated rates of diagnostic paracentesis.
Disclosures:
Chung-Heng Liu indicated no relevant financial relationships.
Gabriel Monti indicated no relevant financial relationships.
Quinn Nelson indicated no relevant financial relationships.
Michael Chang indicated no relevant financial relationships.
Chung-Heng Liu, MD, Gabriel Monti, MD, Quinn Nelson, MD, Michael Chang, MD. P1616 - A Quality Improvement Study to Increase Diagnostic Paracentesis for Admitted Veterans With Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Oregon Health & Science University, Portland, OR
Introduction: Multiple society guidelines recommend diagnostic paracentesis in all patients admitted to the hospital with cirrhosis and ascites. However, one multi-center study conducted at Veteran Administration (VA) medical centers demonstrated < 15% of patients received early paracentesis (EP) within 24h of initial presentation. The aim of this quality improvement (QI) study is to evaluate whether an educational intervention can improve the frequency of timely diagnostic paracentesis.
Methods: This QI study was based on a 90-minute simulation-based educational session for all internal medicine trainees rotating at our VA inpatient service for each 3-week rotation started on January 13, 2025. The simulation utilized a mannequin and all the supplied necessary to perform a paracentesis at our facility. Furthermore, education regarding the indication for paracentesis was provided to all attendees.
Outcomes were analyzed using statistical process control C chart of these data for both outcomes. Special cause variation was noted by the presence of a data point outside the upper control limit. Veterans were also divided into 2 cohorts, pre-intervention (October 2024 to December 2024) and post-intervention (January 2025 to April 2025).
Results: 132 Veterans (96.8% male and median age 72 years) with liver cirrhosis were admitted from October 1, 2024 – April 14, 2025. 28% of the cohort (N=37) had ascites present on admission. Amongst those with ascites, 20 (54%) and 14 (38%) Veterans had a diagnostic paracentesis at any point during their admission and EP, respectively. Special cause variation is noted in those undergoing diagnostic paracentesis after the educational intervention (Figure 1). A similar relationship was not observed for Veterans who received EP. There is no significant difference in proportion of paracentesis between the pre- and post- intervention cohorts (Figure 2).
Discussion: Early data from this QI study suggest that implementation of a structured educational simulation for internal medicine trainees increased the frequency of diagnostic paracentesis for Veterans with cirrhosis and ascites admitted to the hospital by means of special cause variation on a C chart. Aggregate comparisons of the pre and post intervention cohorts failed to show a statistically significant improvement, likely due to small sample size. Ongoing efforts aimed at both trainees and attending hospitalists are underway.
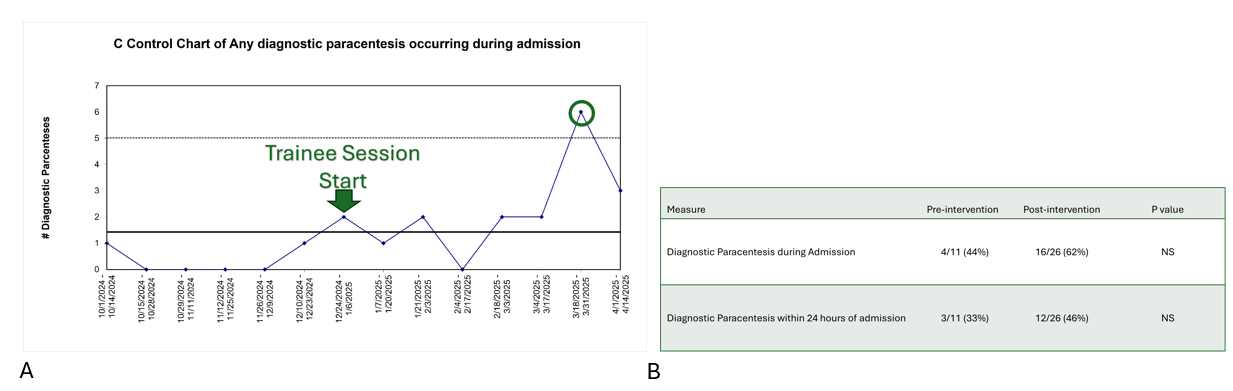
Figure: (A) Statistical process control C chart of any diagnostic paracentesis during admissions; (B) Table comparing aggregated rates of diagnostic paracentesis.
Disclosures:
Chung-Heng Liu indicated no relevant financial relationships.
Gabriel Monti indicated no relevant financial relationships.
Quinn Nelson indicated no relevant financial relationships.
Michael Chang indicated no relevant financial relationships.
Chung-Heng Liu, MD, Gabriel Monti, MD, Quinn Nelson, MD, Michael Chang, MD. P1616 - A Quality Improvement Study to Increase Diagnostic Paracentesis for Admitted Veterans With Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
