Sunday Poster Session
Category: Liver
P1612 - Herbal Supplement-Induced Liver Injury: A Systematic Review of Clinical Characteristics and Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed B. Elnaggar, MD
Hartford Healthcare
Hartford, CT
Presenting Author(s)
Mohamed A. B. Elnaggar, MD1, Mohamed Saad Sayed, MBBCh2, Husam Abu Suilik, MD3, Abanoub Mokhles, MBBCh4, Mo'tasem Abdelaziz, MBBCH5, Amr A. Salem, MD6, Ismail Elkhattib, MBBCh7, Mahmoud Elsayed, MD8, Mohamed Abuelazm, 9
1Hartford Healthcare, Hartford, CT; 2Faculty of Medicine, Ihnasya, Bani Suwayf, Egypt; 3The Hashemite University, Zarqa, Az Zarqa', Jordan; 4University of Sohag, Cairo, Suhaj, Egypt; 5Faculty of Medicine, Bani Sueif University, Bani Suwayf, Bani Suwayf, Egypt; 6Boston University, Boston, MA; 7University of Nebraska, Hartford, CT; 8Massachusetts General Hospital-Harvard University, Boston, MA; 9Faculty of Medicine, Tanta University, Tanta, Egypt, Tanta, Al Gharbiyah, Egypt
Introduction: The use of herbal supplements has increased globally, leading to rising reports of adverse health effects, including hepatotoxicity. However, comprehensive data summarizing the clinical characteristics and outcomes of supplement-induced liver injury are limited.
Methods: Five different databases, including PubMed, Embase, and Web of Science, were searched up to December 17, 2024. We included all studies that reported liver injury associated with herbal supplement use. The data was extracted using a uniform Excel extraction sheet. All statistical tests were conducted with a 95% confidence interval and a 5% margin of error. A p-value of less than 0.05 was considered statistically significant
Results: A total of 293 cases of herbal supplement-induced liver injury were identified from published reports. The most common study design was case-control (57.7%), followed by case reports (14.7%), case series (13.3%), observational studies (9.9%), and letters (2.7%). Khat was the most frequently implicated supplement (202 cases, 69.0%), followed by turmeric/curcuma (61 cases, 20.8%) and ashwagandha (23 cases, 7.8%). Other supplements, including rooibos tea and Yogi herbal tea, accounted for a small minority of cases. Of the patients described, 152 (51.9%) were female, 136 (46.4%) were male, and the gender was unspecified in 5 cases (1.7%). The most commonly reported symptoms were jaundice (36 cases, 12.3%), abdominal discomfort or pain (17 cases, 5.8%), and pruritus (16 cases, 5.5%). Discontinuation of the offending supplement was reported as a management strategy in 23 cases (7.8%). Corticosteroid therapy was used in 11 cases (3.8%), and supportive therapy (such as N-acetylcysteine or ursodeoxycholic acid) in 12 cases (4.1%). Most patients (261 cases, 89.1%) recovered fully, while mortality was reported in 9 cases (3.1%). The outcome was unknown in 23 cases (7.9%).
Discussion: Herbal supplements such as khat, turmeric/curcuma, and ashwagandha can cause liver injury, typically presenting with jaundice and abdominal discomfort. Most patients recover, but severe cases do occur. Greater awareness and better reporting are needed to ensure safe use.
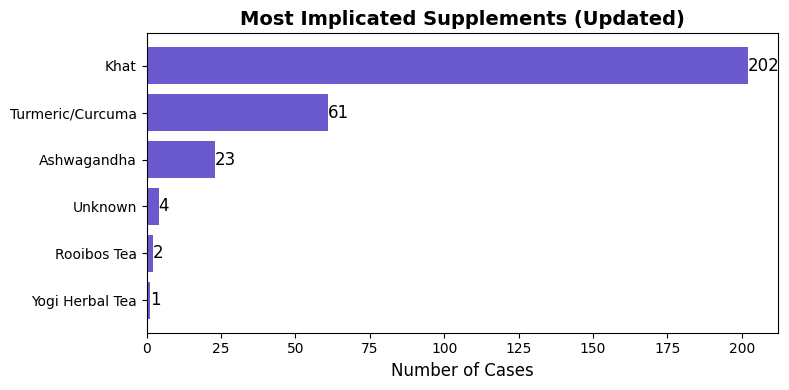
Figure: Most implicated supplements
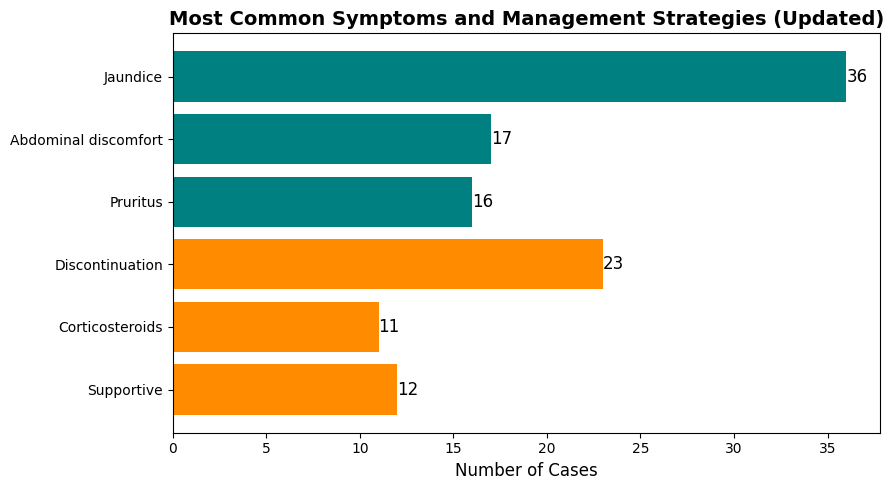
Figure: Most common symptoms and management strategies
Disclosures:
Mohamed A. Elnaggar indicated no relevant financial relationships.
Mohamed Saad Sayed indicated no relevant financial relationships.
Husam Abu Suilik indicated no relevant financial relationships.
Abanoub Mokhles indicated no relevant financial relationships.
Mo'tasem Abdelaziz indicated no relevant financial relationships.
Amr A. Salem indicated no relevant financial relationships.
Ismail Elkhattib indicated no relevant financial relationships.
Mahmoud Elsayed indicated no relevant financial relationships.
Mohamed Abuelazm indicated no relevant financial relationships.
Mohamed A. B. Elnaggar, MD1, Mohamed Saad Sayed, MBBCh2, Husam Abu Suilik, MD3, Abanoub Mokhles, MBBCh4, Mo'tasem Abdelaziz, MBBCH5, Amr A. Salem, MD6, Ismail Elkhattib, MBBCh7, Mahmoud Elsayed, MD8, Mohamed Abuelazm, 9. P1612 - Herbal Supplement-Induced Liver Injury: A Systematic Review of Clinical Characteristics and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hartford Healthcare, Hartford, CT; 2Faculty of Medicine, Ihnasya, Bani Suwayf, Egypt; 3The Hashemite University, Zarqa, Az Zarqa', Jordan; 4University of Sohag, Cairo, Suhaj, Egypt; 5Faculty of Medicine, Bani Sueif University, Bani Suwayf, Bani Suwayf, Egypt; 6Boston University, Boston, MA; 7University of Nebraska, Hartford, CT; 8Massachusetts General Hospital-Harvard University, Boston, MA; 9Faculty of Medicine, Tanta University, Tanta, Egypt, Tanta, Al Gharbiyah, Egypt
Introduction: The use of herbal supplements has increased globally, leading to rising reports of adverse health effects, including hepatotoxicity. However, comprehensive data summarizing the clinical characteristics and outcomes of supplement-induced liver injury are limited.
Methods: Five different databases, including PubMed, Embase, and Web of Science, were searched up to December 17, 2024. We included all studies that reported liver injury associated with herbal supplement use. The data was extracted using a uniform Excel extraction sheet. All statistical tests were conducted with a 95% confidence interval and a 5% margin of error. A p-value of less than 0.05 was considered statistically significant
Results: A total of 293 cases of herbal supplement-induced liver injury were identified from published reports. The most common study design was case-control (57.7%), followed by case reports (14.7%), case series (13.3%), observational studies (9.9%), and letters (2.7%). Khat was the most frequently implicated supplement (202 cases, 69.0%), followed by turmeric/curcuma (61 cases, 20.8%) and ashwagandha (23 cases, 7.8%). Other supplements, including rooibos tea and Yogi herbal tea, accounted for a small minority of cases. Of the patients described, 152 (51.9%) were female, 136 (46.4%) were male, and the gender was unspecified in 5 cases (1.7%). The most commonly reported symptoms were jaundice (36 cases, 12.3%), abdominal discomfort or pain (17 cases, 5.8%), and pruritus (16 cases, 5.5%). Discontinuation of the offending supplement was reported as a management strategy in 23 cases (7.8%). Corticosteroid therapy was used in 11 cases (3.8%), and supportive therapy (such as N-acetylcysteine or ursodeoxycholic acid) in 12 cases (4.1%). Most patients (261 cases, 89.1%) recovered fully, while mortality was reported in 9 cases (3.1%). The outcome was unknown in 23 cases (7.9%).
Discussion: Herbal supplements such as khat, turmeric/curcuma, and ashwagandha can cause liver injury, typically presenting with jaundice and abdominal discomfort. Most patients recover, but severe cases do occur. Greater awareness and better reporting are needed to ensure safe use.
Figure: Most implicated supplements
Figure: Most common symptoms and management strategies
Disclosures:
Mohamed A. Elnaggar indicated no relevant financial relationships.
Mohamed Saad Sayed indicated no relevant financial relationships.
Husam Abu Suilik indicated no relevant financial relationships.
Abanoub Mokhles indicated no relevant financial relationships.
Mo'tasem Abdelaziz indicated no relevant financial relationships.
Amr A. Salem indicated no relevant financial relationships.
Ismail Elkhattib indicated no relevant financial relationships.
Mahmoud Elsayed indicated no relevant financial relationships.
Mohamed Abuelazm indicated no relevant financial relationships.
Mohamed A. B. Elnaggar, MD1, Mohamed Saad Sayed, MBBCh2, Husam Abu Suilik, MD3, Abanoub Mokhles, MBBCh4, Mo'tasem Abdelaziz, MBBCH5, Amr A. Salem, MD6, Ismail Elkhattib, MBBCh7, Mahmoud Elsayed, MD8, Mohamed Abuelazm, 9. P1612 - Herbal Supplement-Induced Liver Injury: A Systematic Review of Clinical Characteristics and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
