Sunday Poster Session
Category: Liver
P1602 - Effects of Bariatric Surgery on Non-Invasive Markers of MASLD
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Junaid khan, MD
Tidal Health
Salisbury, MD
Presenting Author(s)
Junaid Khan, MD1, Ismet Lukolic, MD, FACG2, Muhammad Jibran, MD3, Mohammad Hamza, MD2, Safana Ismail, MD3, Michael Mccabe, MD2, Anurag Maheshwari, MD, FACG4
1Tidal Health, Salisbury, MD; 2Tidalhealth, Salisbury, MD; 3TidalHealth, Salisbury, MD; 4Mercy Medical Center, Baltimore, MD
Introduction: MASLD is among the most prevalent liver conditions, leading to cirrhosis and liver cancer. This study evaluated the impact of bariatric surgery on MASLD.
Methods: This was a retrospective study of 181 patients undergoing weight loss surgery (sleeve gastrectomy (SG=54) or Roux-en-Y gastric bypass (RGB=127)) at TidalHealth, Salisbury, MD from 2017-22. Non-invasive markers of fibrosis: FIB-4, NAFLD Fibrosis Score (NFS), and BARD were assessed at baseline and 12–18 months post-op. Change in fibrosis was assessed using the paired t-test. Secondary outcomes included the prevalence of GLP-1 analog and statin use before and after surgery. Baseline demographics including BMI, AST, ALT, platelet count, and comorbidities (diabetes, hypertension) are presented in Table 1. Pre- and post-op changes in non-invasive fibrosis scores are summarized in Table 2.
Results: Mean change in BMI was 46.2 to 37.8 (p < 0.001). A statistically significant reduction in the mean NFS (0.205 to -0.373, p = 0.0001; 95% CI: 0.28 to 0.87) was observed, indicating a shift in fibrosis scores from the indeterminate to the low-risk fibrosis category for the entire cohort. In a subgroup of 25 patients with advanced baseline fibrosis (NFS stage F3–F4), bariatric surgery resulted in a significant reduction in NFS from 1.63 to 0.84 (p = 0.001), indicative of meaningful fibrosis regression. Changes in other markers of fibrosis were not as consistent; FIB-4 score exhibited a modest but significant increase (0.95 to 1.02; p = 0.004; 95% CI: -0.18 to -0.04), while the BARD score decreased (2.90 to 2.01, p = 0.91; 95% CI: -0.20 to 0.19). In the subgroup with advanced fibrosis at baseline, the drop in BARD score was statistically significant (3.48 to 3.28; p = 0.05). However, the FIB-4 score remained essentially unchanged (1.94 to 1.92; p = 0.80), highlighting the limitations of this test. Post-op, the use of GLP-1 receptor agonists and statins increased significantly (10% to 19.3%, and 32.5% to 42.5%, p = 0.005 and p = 0.04, respectively).
Discussion: Bariatric surgery resulted in significant improvement in the fibrosis markers of MASLD, as shown by reduction in the NFS. Changes in the FIB-4 and BARD scores were less consistent, suggesting these tests are less useful in the longitudinal assessments of fibrosis amongst patients with MASLD. As an ancillary benefit, we observed an increase in the use of GLP-1 analogs and statins, suggesting a trend toward improved management of the underlying metabolic syndrome.
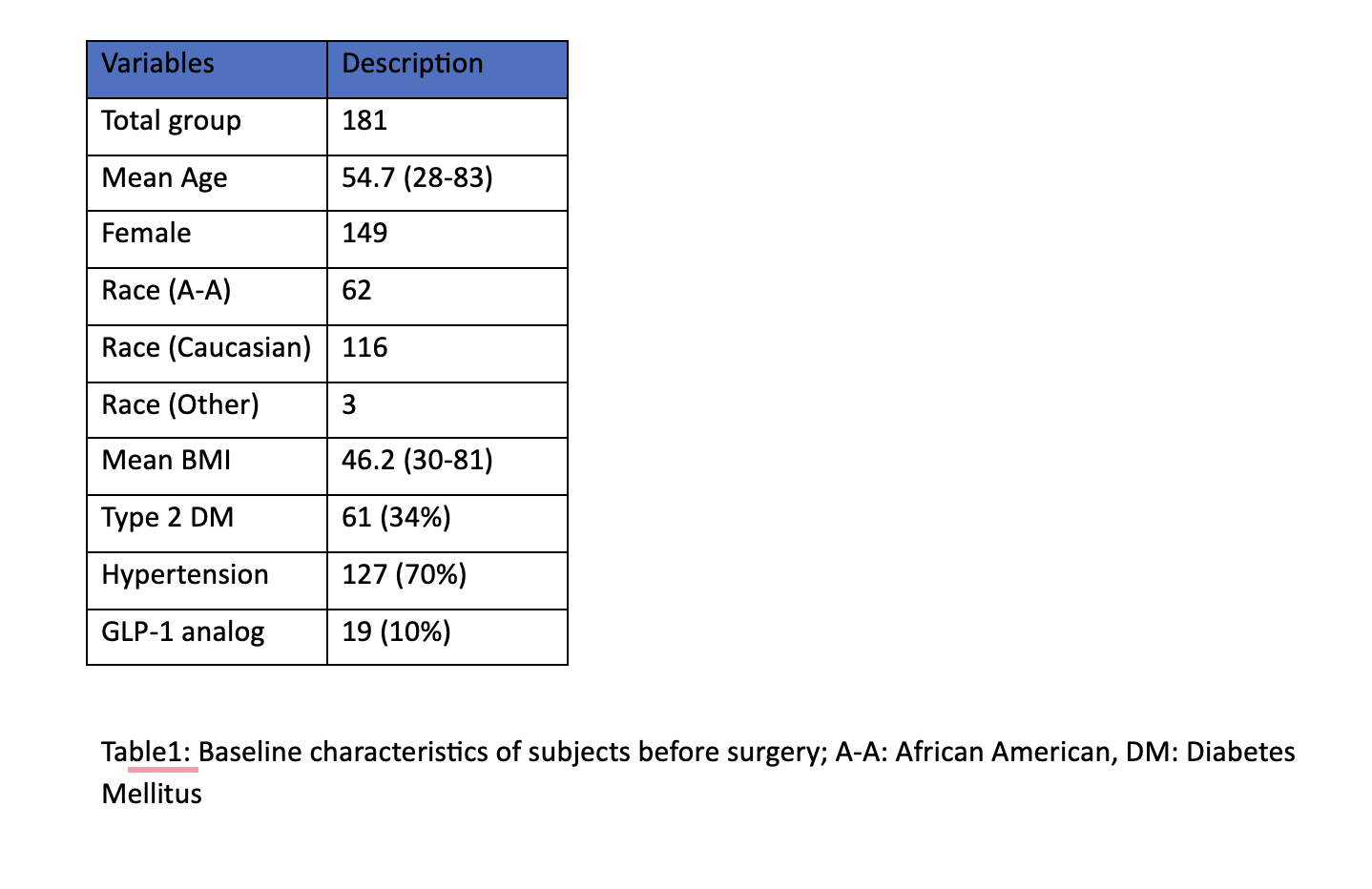
Figure: Table 1: Baseline characteristics
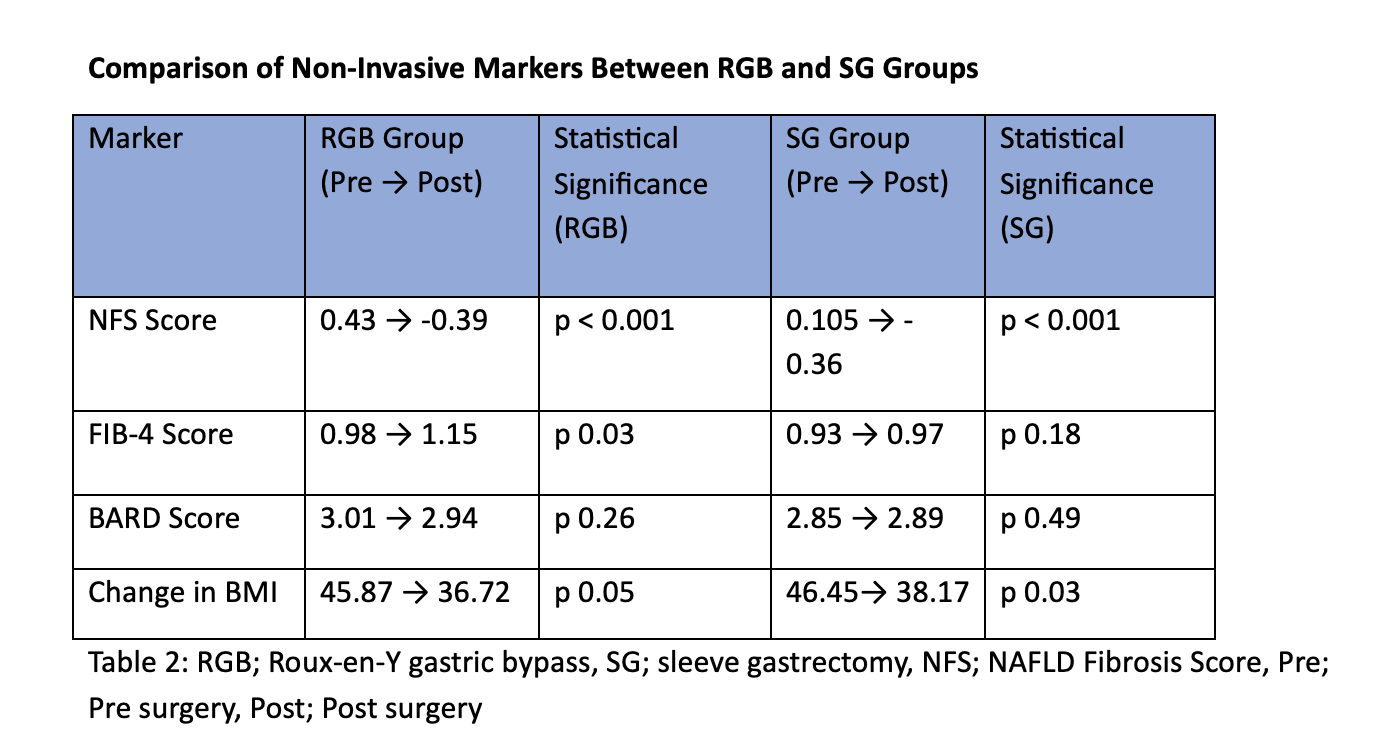
Figure: Comparison of Non-Invasive Markers Between RGB and SG Groups
Disclosures:
Junaid Khan indicated no relevant financial relationships.
Ismet Lukolic indicated no relevant financial relationships.
Muhammad Jibran indicated no relevant financial relationships.
Mohammad Hamza indicated no relevant financial relationships.
Safana Ismail indicated no relevant financial relationships.
Michael Mccabe indicated no relevant financial relationships.
Anurag Maheshwari indicated no relevant financial relationships.
Junaid Khan, MD1, Ismet Lukolic, MD, FACG2, Muhammad Jibran, MD3, Mohammad Hamza, MD2, Safana Ismail, MD3, Michael Mccabe, MD2, Anurag Maheshwari, MD, FACG4. P1602 - Effects of Bariatric Surgery on Non-Invasive Markers of MASLD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tidal Health, Salisbury, MD; 2Tidalhealth, Salisbury, MD; 3TidalHealth, Salisbury, MD; 4Mercy Medical Center, Baltimore, MD
Introduction: MASLD is among the most prevalent liver conditions, leading to cirrhosis and liver cancer. This study evaluated the impact of bariatric surgery on MASLD.
Methods: This was a retrospective study of 181 patients undergoing weight loss surgery (sleeve gastrectomy (SG=54) or Roux-en-Y gastric bypass (RGB=127)) at TidalHealth, Salisbury, MD from 2017-22. Non-invasive markers of fibrosis: FIB-4, NAFLD Fibrosis Score (NFS), and BARD were assessed at baseline and 12–18 months post-op. Change in fibrosis was assessed using the paired t-test. Secondary outcomes included the prevalence of GLP-1 analog and statin use before and after surgery. Baseline demographics including BMI, AST, ALT, platelet count, and comorbidities (diabetes, hypertension) are presented in Table 1. Pre- and post-op changes in non-invasive fibrosis scores are summarized in Table 2.
Results: Mean change in BMI was 46.2 to 37.8 (p < 0.001). A statistically significant reduction in the mean NFS (0.205 to -0.373, p = 0.0001; 95% CI: 0.28 to 0.87) was observed, indicating a shift in fibrosis scores from the indeterminate to the low-risk fibrosis category for the entire cohort. In a subgroup of 25 patients with advanced baseline fibrosis (NFS stage F3–F4), bariatric surgery resulted in a significant reduction in NFS from 1.63 to 0.84 (p = 0.001), indicative of meaningful fibrosis regression. Changes in other markers of fibrosis were not as consistent; FIB-4 score exhibited a modest but significant increase (0.95 to 1.02; p = 0.004; 95% CI: -0.18 to -0.04), while the BARD score decreased (2.90 to 2.01, p = 0.91; 95% CI: -0.20 to 0.19). In the subgroup with advanced fibrosis at baseline, the drop in BARD score was statistically significant (3.48 to 3.28; p = 0.05). However, the FIB-4 score remained essentially unchanged (1.94 to 1.92; p = 0.80), highlighting the limitations of this test. Post-op, the use of GLP-1 receptor agonists and statins increased significantly (10% to 19.3%, and 32.5% to 42.5%, p = 0.005 and p = 0.04, respectively).
Discussion: Bariatric surgery resulted in significant improvement in the fibrosis markers of MASLD, as shown by reduction in the NFS. Changes in the FIB-4 and BARD scores were less consistent, suggesting these tests are less useful in the longitudinal assessments of fibrosis amongst patients with MASLD. As an ancillary benefit, we observed an increase in the use of GLP-1 analogs and statins, suggesting a trend toward improved management of the underlying metabolic syndrome.
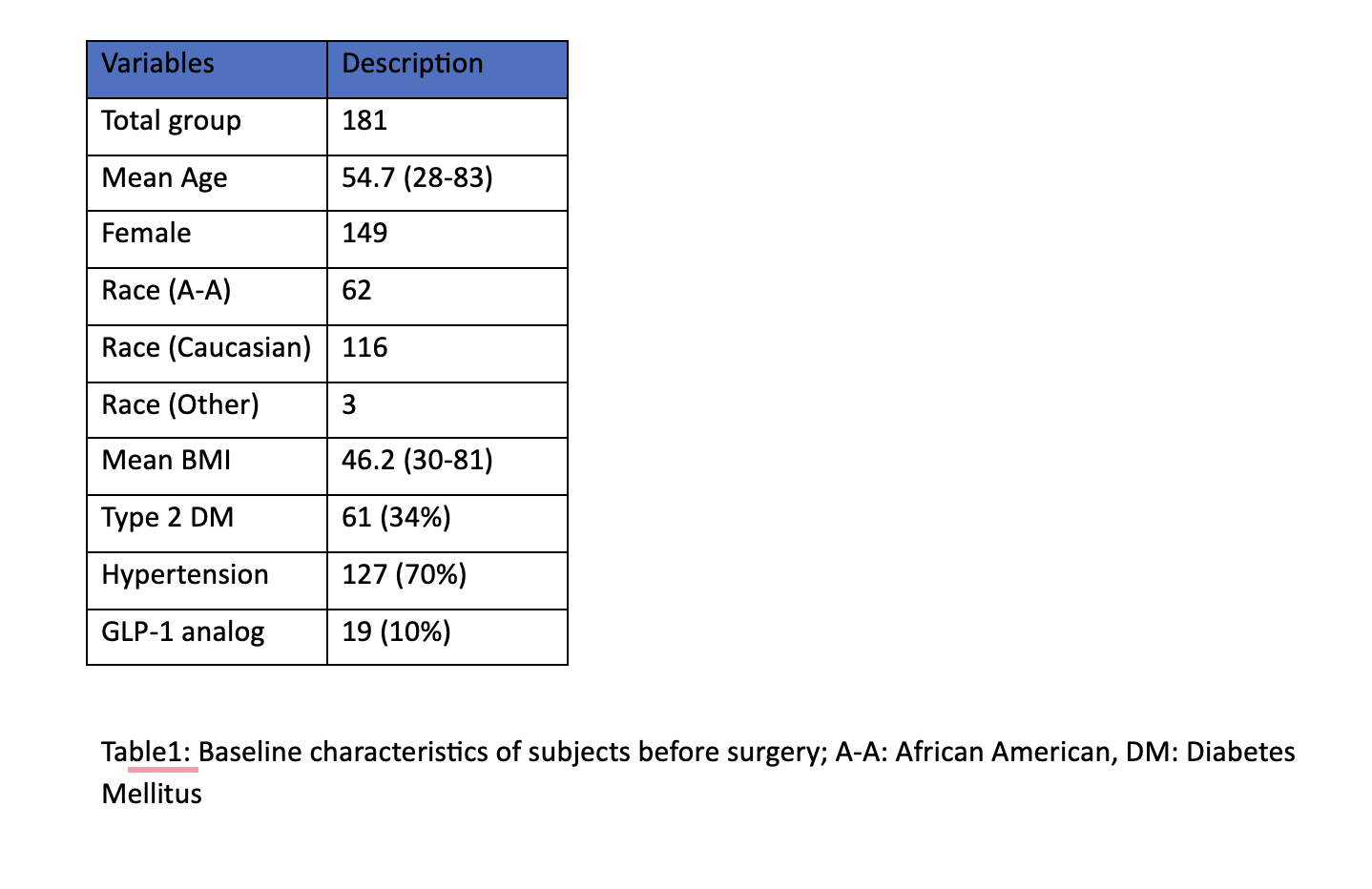
Figure: Table 1: Baseline characteristics
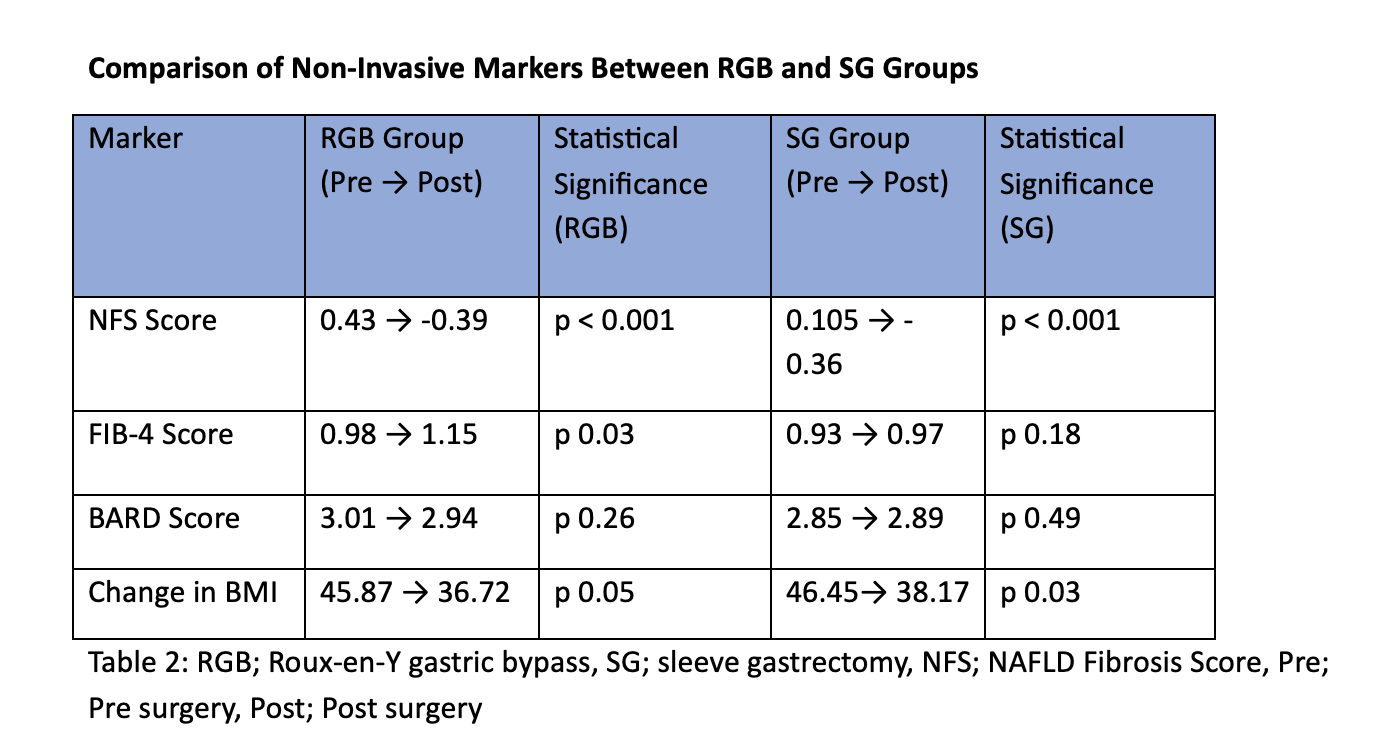
Figure: Comparison of Non-Invasive Markers Between RGB and SG Groups
Disclosures:
Junaid Khan indicated no relevant financial relationships.
Ismet Lukolic indicated no relevant financial relationships.
Muhammad Jibran indicated no relevant financial relationships.
Mohammad Hamza indicated no relevant financial relationships.
Safana Ismail indicated no relevant financial relationships.
Michael Mccabe indicated no relevant financial relationships.
Anurag Maheshwari indicated no relevant financial relationships.
Junaid Khan, MD1, Ismet Lukolic, MD, FACG2, Muhammad Jibran, MD3, Mohammad Hamza, MD2, Safana Ismail, MD3, Michael Mccabe, MD2, Anurag Maheshwari, MD, FACG4. P1602 - Effects of Bariatric Surgery on Non-Invasive Markers of MASLD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
