Sunday Poster Session
Category: Liver
P1595 - Combined Platelet Count and Fib-4 Score for Risk Stratification in MASLD: Perfect Separation of Advanced Disease in a Veteran Population
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jacky Reny, MD (he/him/his)
Stony Brook University Hospital
Port Jefferson Station, NY
Presenting Author(s)
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, David Stein, MD2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4
1Stony Brook University Hospital, Port Jefferson Station, NY; 2Stony Brook Medicine, Stony Brook, NY; 3Philadelphia College of Osteopathic Medicine, Philadelphia, PA; 4Stony Brook University Hospital, Northport, NY
Introduction: Early identification of advanced fibrosis is essential in MASLD to guide referral, monitoring, and therapeutic intervention. Noninvasive scoring systems such as Fib-4 are widely recommended, yet their use may be limited by accessibility. Platelet count is routinely available, and has been associated with liver fibrosis. However, the value and practical impact of combining platelet count with Fib-4 for rapid risk stratification has not been systematically assessed. We aimed to evaluate whether an approach using both platelet count and Fib-4 score can achieve near-perfect separation of patients at risk for advanced fibrosis, and to characterize the clinical features of discordant phenotypes.
Methods: We conducted a retrospective cohort analysis of 80 adults with MASLD from a veteran's affairs hospital. Demographic, clinical, and laboratory data were abstracted from the EMR. Advanced fibrosis was defined by Fib-4 >2.67 or clinical cirrhosis diagnosis. Platelet count < 162 x10⁹/L, identified by ROC analysis, was used as the optimal threshold. Patients were stratified based on combinations of platelet count and Fib-4 score. Sensitivity, specificity, NPV, and PPV were calculated for both single and combined strategies. Discordant cases were analyzed for demographic and clinical differences.
Results: All patients with advanced fibrosis (n = 10,12.3%) had either a high Fib-4 ( >2.67) or a low platelet count (< 162 x10⁹/L), resulting in 100% sensitivity and NPV for the combined approach. No patient with both a normal platelet count and low/intermediate Fib-4 had advanced fibrosis. The specificity of the strategy was 68%, and PPV was 22%. Discordant cases (low platelet, low Fib-4) were older (mean age 73 vs. 58 years), more likely to have diabetes (81% vs. 38%), and had lower BMI (30.4 vs. 30.8). Multivariable regression confirmed that the combination of platelet count and Fib-4 offered superior discrimination for advanced disease compared to either marker alone (p < 0.001).
Discussion: The combination of platelet count and Fib-4 score provided perfect NPV for advanced fibrosis in this cohort. This simple two-step rule—advanced fibrosis ruled out if both platelet count ≥162 x10⁹/L and Fib-4 ≤2.67—can serve as an effective and accessible triage tool, reducing unnecessary specialty referrals and diagnostic testing. Discordant cases represent a unique phenotype characterized by older age and greater metabolic risk, highlighting the need for prospective validation in larger cohort.
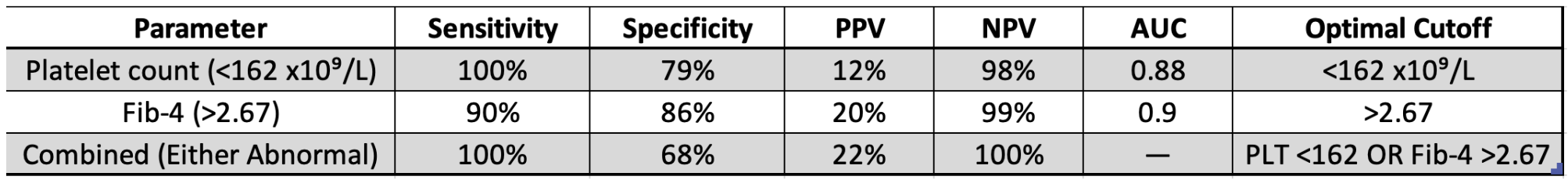
Figure: Diagnostic Performance of Platelet Count and Fib-4 for Advanced Fibrosis in MASLD
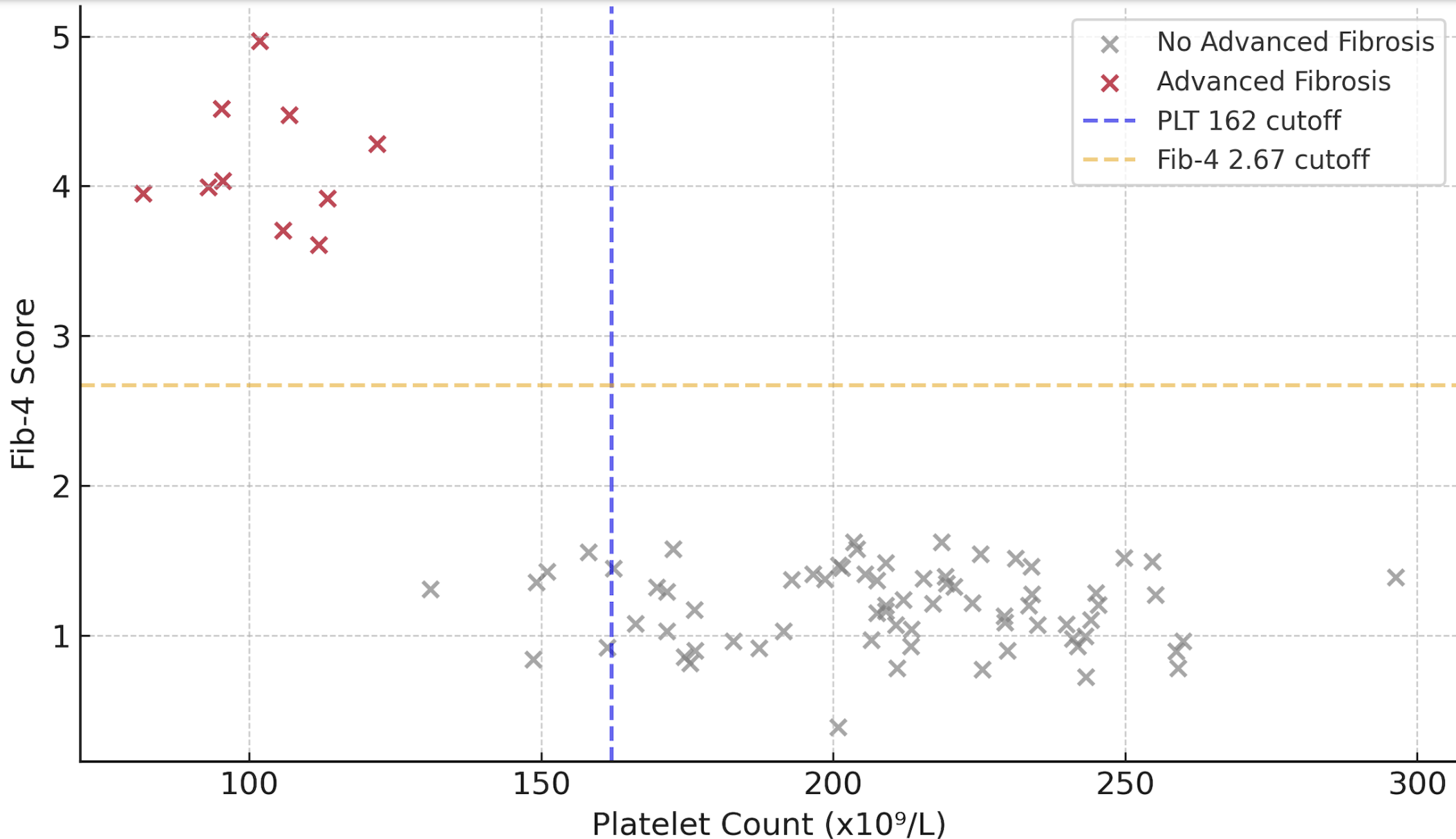
Figure: Distribution of Platelet Counts and Fib-4 by Fibrosis Status
Disclosures:
Jacky Reny indicated no relevant financial relationships.
Jordan Barnett-Kradjian indicated no relevant financial relationships.
David Stein indicated no relevant financial relationships.
Kaustav Patra indicated no relevant financial relationships.
Pallavi Kawatra indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, David Stein, MD2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4. P1595 - Combined Platelet Count and Fib-4 Score for Risk Stratification in MASLD: Perfect Separation of Advanced Disease in a Veteran Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stony Brook University Hospital, Port Jefferson Station, NY; 2Stony Brook Medicine, Stony Brook, NY; 3Philadelphia College of Osteopathic Medicine, Philadelphia, PA; 4Stony Brook University Hospital, Northport, NY
Introduction: Early identification of advanced fibrosis is essential in MASLD to guide referral, monitoring, and therapeutic intervention. Noninvasive scoring systems such as Fib-4 are widely recommended, yet their use may be limited by accessibility. Platelet count is routinely available, and has been associated with liver fibrosis. However, the value and practical impact of combining platelet count with Fib-4 for rapid risk stratification has not been systematically assessed. We aimed to evaluate whether an approach using both platelet count and Fib-4 score can achieve near-perfect separation of patients at risk for advanced fibrosis, and to characterize the clinical features of discordant phenotypes.
Methods: We conducted a retrospective cohort analysis of 80 adults with MASLD from a veteran's affairs hospital. Demographic, clinical, and laboratory data were abstracted from the EMR. Advanced fibrosis was defined by Fib-4 >2.67 or clinical cirrhosis diagnosis. Platelet count < 162 x10⁹/L, identified by ROC analysis, was used as the optimal threshold. Patients were stratified based on combinations of platelet count and Fib-4 score. Sensitivity, specificity, NPV, and PPV were calculated for both single and combined strategies. Discordant cases were analyzed for demographic and clinical differences.
Results: All patients with advanced fibrosis (n = 10,12.3%) had either a high Fib-4 ( >2.67) or a low platelet count (< 162 x10⁹/L), resulting in 100% sensitivity and NPV for the combined approach. No patient with both a normal platelet count and low/intermediate Fib-4 had advanced fibrosis. The specificity of the strategy was 68%, and PPV was 22%. Discordant cases (low platelet, low Fib-4) were older (mean age 73 vs. 58 years), more likely to have diabetes (81% vs. 38%), and had lower BMI (30.4 vs. 30.8). Multivariable regression confirmed that the combination of platelet count and Fib-4 offered superior discrimination for advanced disease compared to either marker alone (p < 0.001).
Discussion: The combination of platelet count and Fib-4 score provided perfect NPV for advanced fibrosis in this cohort. This simple two-step rule—advanced fibrosis ruled out if both platelet count ≥162 x10⁹/L and Fib-4 ≤2.67—can serve as an effective and accessible triage tool, reducing unnecessary specialty referrals and diagnostic testing. Discordant cases represent a unique phenotype characterized by older age and greater metabolic risk, highlighting the need for prospective validation in larger cohort.
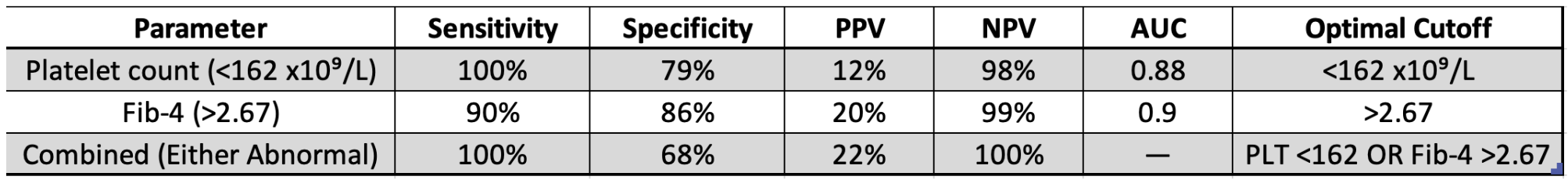
Figure: Diagnostic Performance of Platelet Count and Fib-4 for Advanced Fibrosis in MASLD
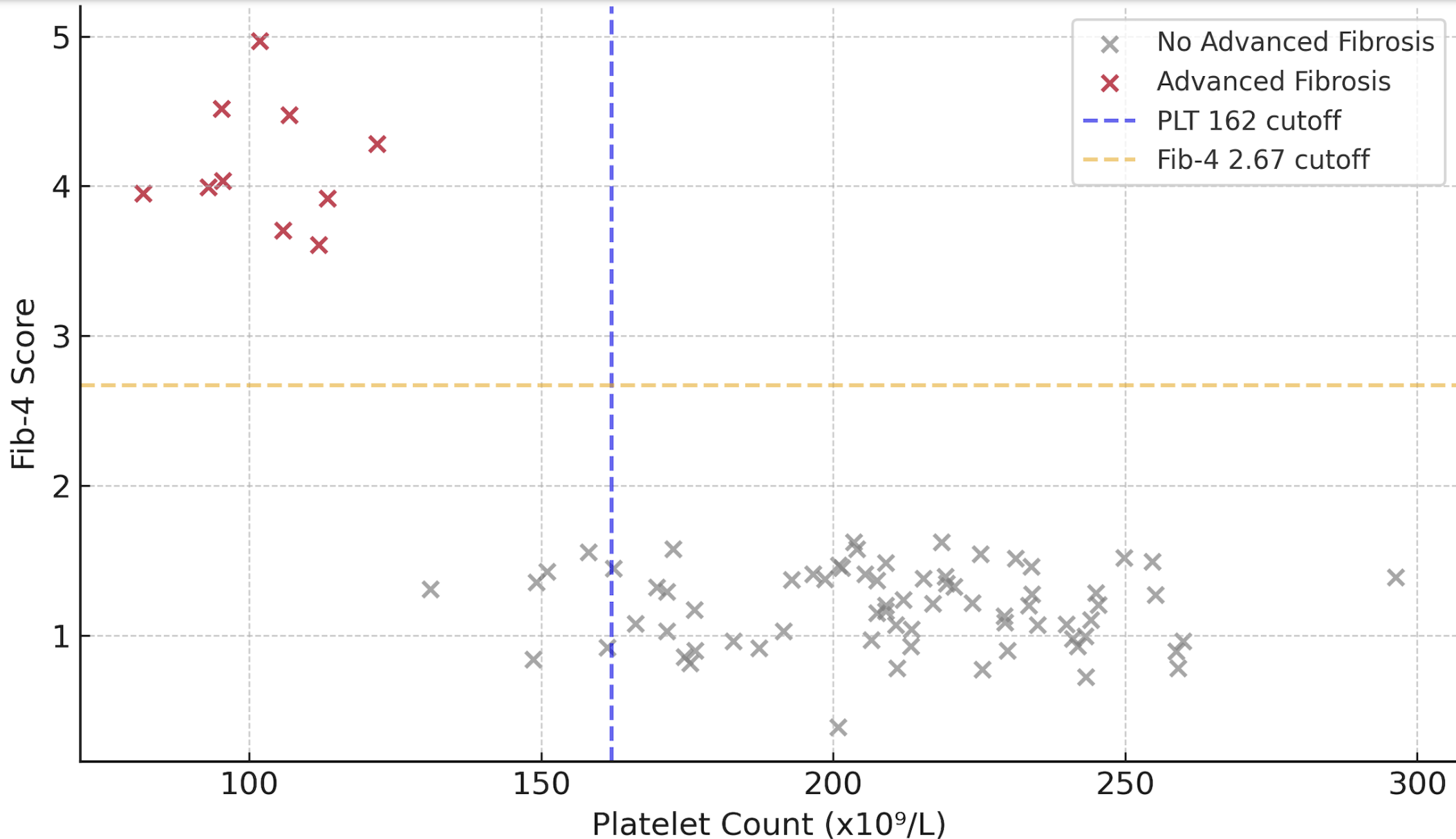
Figure: Distribution of Platelet Counts and Fib-4 by Fibrosis Status
Disclosures:
Jacky Reny indicated no relevant financial relationships.
Jordan Barnett-Kradjian indicated no relevant financial relationships.
David Stein indicated no relevant financial relationships.
Kaustav Patra indicated no relevant financial relationships.
Pallavi Kawatra indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, David Stein, MD2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4. P1595 - Combined Platelet Count and Fib-4 Score for Risk Stratification in MASLD: Perfect Separation of Advanced Disease in a Veteran Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

