Sunday Poster Session
Category: Liver
P1593 - Association of Fib-4 Score and Body Mass Index With Cirrhosis in a Contemporary MASLD Cohort
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jacky Reny, MD (he/him/his)
Stony Brook University Hospital
Port Jefferson Station, NY
Presenting Author(s)
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4
1Stony Brook University Hospital, Port Jefferson Station, NY; 2Stony Brook Medicine, Stony Brook, NY; 3Philadelphia College of Osteopathic Medicine, Philadelphia, PA; 4Stony Brook University Hospital, Northport, NY
Introduction: MASLD is now the leading cause of chronic liver disease globally, with rates of advanced fibrosis and cirrhosis rising rapidly. While noninvasive scores such as Fib-4 are widely used to estimate fibrosis risk, and obesity is a recognized risk factor for MASLD progression, the quantitative relationship between BMI and cirrhosis remains incompletely defined. We aimed to evaluate the independent and combined associations of Fib-4 and BMI with cirrhosis in a MASLD cohort, and to determine whether the risk of cirrhosis rises progressively with increasing BMI once obesity is established.
Methods: We conducted a retrospective cross-sectional study of 80 adults with MASLD followed at a veteran's affair hospital. Multiple clinical and laboratory data were abstracted from the EMR. Cirrhosis was defined by provider diagnosis or evidence of decompensated liver disease. Patients were categorized into BMI quartiles and standard obesity classes. Group comparisons were made using Mann-Whitney U test and Fisher’s exact test as appropriate. Multivariable logistic regression evaluated Fib-4 and BMI as independent predictors of cirrhosis, and a quadratic term for BMI was used to assess for dose-response versus plateau effects.
Results: Of 80 patients, 6 (7.4%) had cirrhosis. Median Fib-4 was significantly higher in cirrhosis patients (4.00 [IQR: 3.16–4.97] vs.1.20 [IQR: 0.87–1.82], p = 0.021), and median BMI was also higher (36.7 [IQR: 33.6–42.1] vs. 31.2 [IQR: 27.5–33.2], p = 0.009). The prevalence of cirrhosis increased stepwise across BMI quartiles: 0% in Q1 (BMI ≤ 28.3), 5% in Q2 (28.3–30.7), 8% in Q3 (30.8–34.8), and 18% in Q4 (BMI ≥ 34.9). Cirrhosis rates by BMI category were 0% (normal/underweight), 5% (overweight), 8% (obese I), 11% (obese II), and 20% (obese III). Logistic regression confirmed both Fib-4 (OR per unit: 2.17, 95% CI 1.14–4.13, p = 0.018) and BMI (OR per unit: 1.19, 95% CI 1.05–1.37, p = 0.007) as independent predictors of cirrhosis.
Discussion: In this contemporary MASLD cohort, both Fib-4 score and body mass index were independently and additively associated with cirrhosis. The risk of cirrhosis increased progressively with rising BMI rather than plateauing once obesity was established. These findings underscore the importance of aggressive risk factor modification and routine risk stratification in patients with elevated BMI. Further prospective studies are warranted to confirm these observations and inform optimal surveillance strategies for high-risk populations.
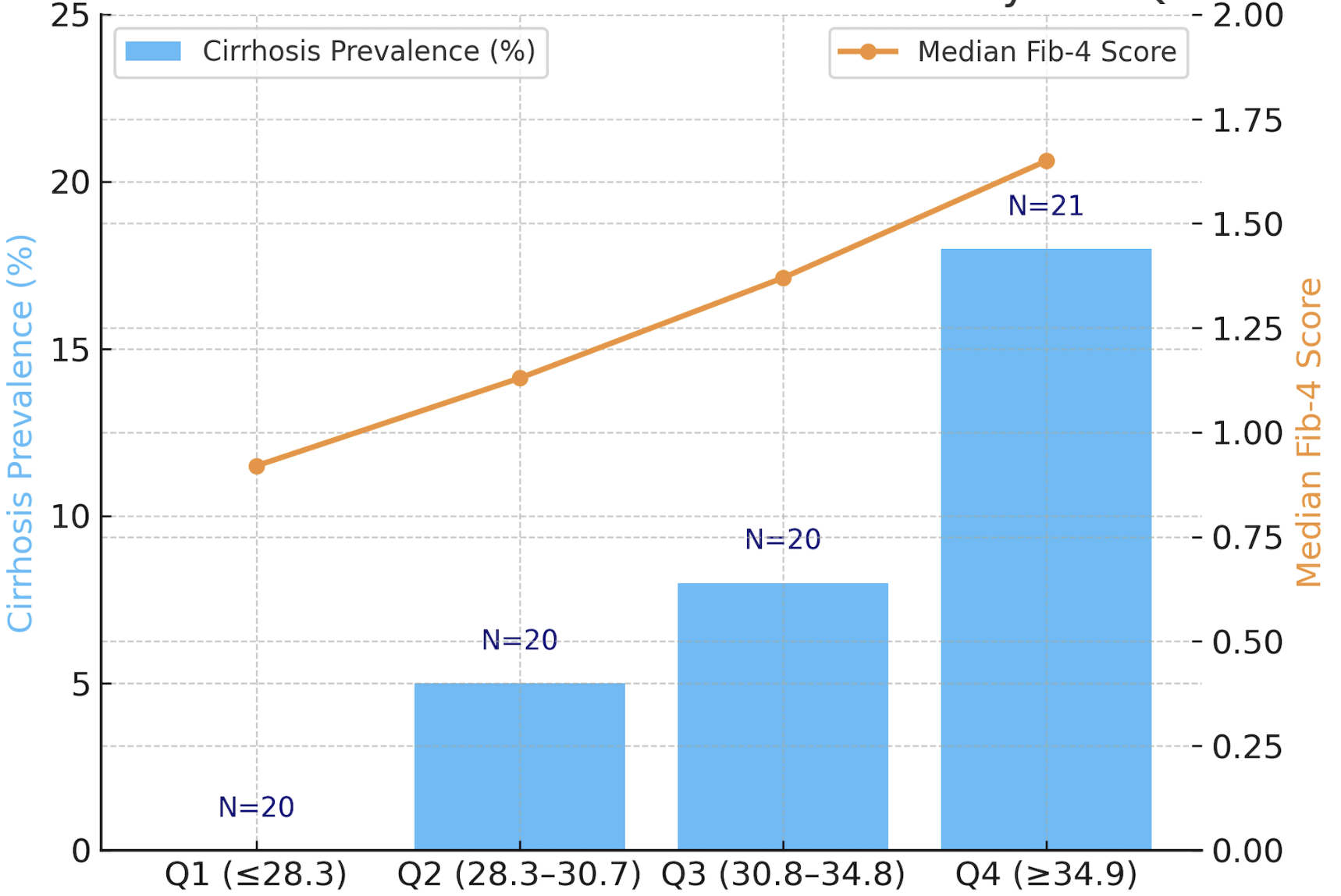
Figure: Table 1: Cirrhosis and Median Fib-4 Score by BMI Quartile
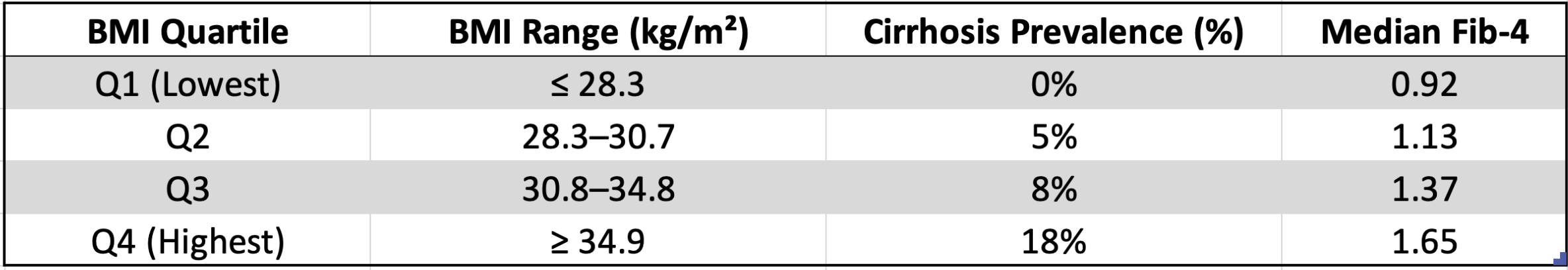
Figure: Chart 1: Cirrhosis and Median Fib-4 Score by BMI Quartile
Disclosures:
Jacky Reny indicated no relevant financial relationships.
Jordan Barnett-Kradjian indicated no relevant financial relationships.
Kaustav Patra indicated no relevant financial relationships.
Pallavi Kawatra indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4. P1593 - Association of Fib-4 Score and Body Mass Index With Cirrhosis in a Contemporary MASLD Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stony Brook University Hospital, Port Jefferson Station, NY; 2Stony Brook Medicine, Stony Brook, NY; 3Philadelphia College of Osteopathic Medicine, Philadelphia, PA; 4Stony Brook University Hospital, Northport, NY
Introduction: MASLD is now the leading cause of chronic liver disease globally, with rates of advanced fibrosis and cirrhosis rising rapidly. While noninvasive scores such as Fib-4 are widely used to estimate fibrosis risk, and obesity is a recognized risk factor for MASLD progression, the quantitative relationship between BMI and cirrhosis remains incompletely defined. We aimed to evaluate the independent and combined associations of Fib-4 and BMI with cirrhosis in a MASLD cohort, and to determine whether the risk of cirrhosis rises progressively with increasing BMI once obesity is established.
Methods: We conducted a retrospective cross-sectional study of 80 adults with MASLD followed at a veteran's affair hospital. Multiple clinical and laboratory data were abstracted from the EMR. Cirrhosis was defined by provider diagnosis or evidence of decompensated liver disease. Patients were categorized into BMI quartiles and standard obesity classes. Group comparisons were made using Mann-Whitney U test and Fisher’s exact test as appropriate. Multivariable logistic regression evaluated Fib-4 and BMI as independent predictors of cirrhosis, and a quadratic term for BMI was used to assess for dose-response versus plateau effects.
Results: Of 80 patients, 6 (7.4%) had cirrhosis. Median Fib-4 was significantly higher in cirrhosis patients (4.00 [IQR: 3.16–4.97] vs.1.20 [IQR: 0.87–1.82], p = 0.021), and median BMI was also higher (36.7 [IQR: 33.6–42.1] vs. 31.2 [IQR: 27.5–33.2], p = 0.009). The prevalence of cirrhosis increased stepwise across BMI quartiles: 0% in Q1 (BMI ≤ 28.3), 5% in Q2 (28.3–30.7), 8% in Q3 (30.8–34.8), and 18% in Q4 (BMI ≥ 34.9). Cirrhosis rates by BMI category were 0% (normal/underweight), 5% (overweight), 8% (obese I), 11% (obese II), and 20% (obese III). Logistic regression confirmed both Fib-4 (OR per unit: 2.17, 95% CI 1.14–4.13, p = 0.018) and BMI (OR per unit: 1.19, 95% CI 1.05–1.37, p = 0.007) as independent predictors of cirrhosis.
Discussion: In this contemporary MASLD cohort, both Fib-4 score and body mass index were independently and additively associated with cirrhosis. The risk of cirrhosis increased progressively with rising BMI rather than plateauing once obesity was established. These findings underscore the importance of aggressive risk factor modification and routine risk stratification in patients with elevated BMI. Further prospective studies are warranted to confirm these observations and inform optimal surveillance strategies for high-risk populations.
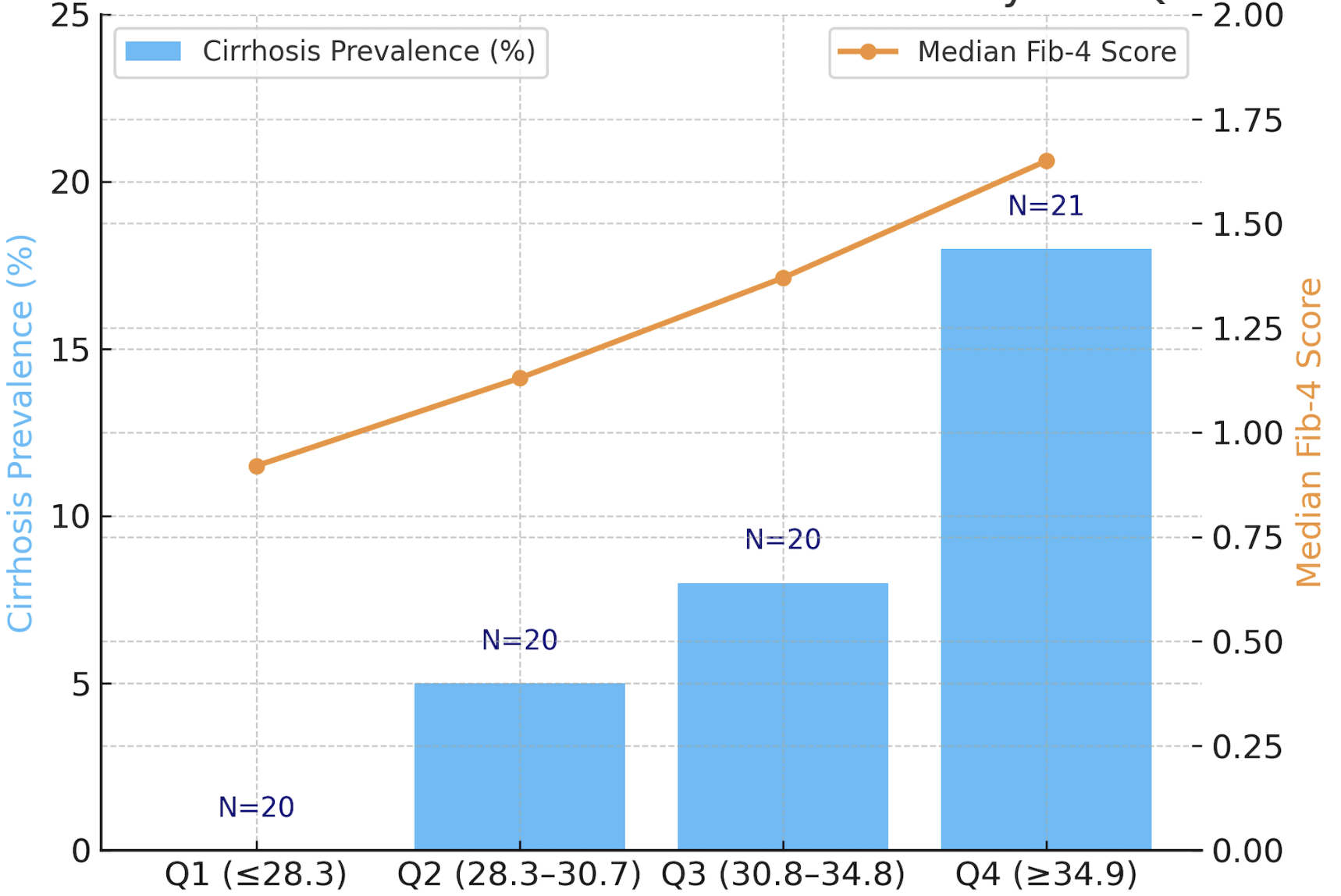
Figure: Table 1: Cirrhosis and Median Fib-4 Score by BMI Quartile
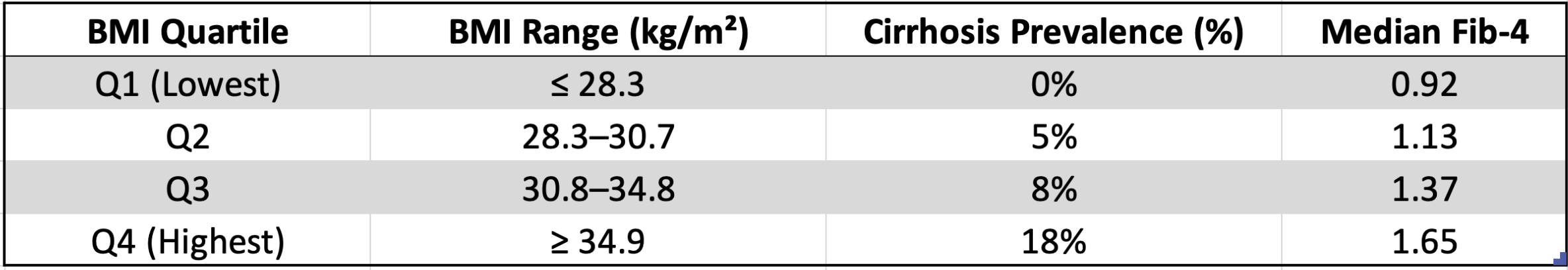
Figure: Chart 1: Cirrhosis and Median Fib-4 Score by BMI Quartile
Disclosures:
Jacky Reny indicated no relevant financial relationships.
Jordan Barnett-Kradjian indicated no relevant financial relationships.
Kaustav Patra indicated no relevant financial relationships.
Pallavi Kawatra indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4. P1593 - Association of Fib-4 Score and Body Mass Index With Cirrhosis in a Contemporary MASLD Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
