Sunday Poster Session
Category: Liver
P1590 - Survival in Early Liver Transplantation in Severe Alcoholic Hepatitis: A Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Meagan H. Phox, DO (she/her/hers)
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Meagan H. Phox, DO1, Mohamed A. Omar, MD1, John Thesing, DO1, David Maundu, MBChB, MSc-HCM, MSc-ID2, Daly Al-Hadeethi, MD3, Clark Kulig, MD4, Nathan Tofteland, MD1
1University of Kansas School of Medicine, Wichita, KS; 2KU School of Medicine-Wichita, Wichita, KS; 3Wichita-KUMC, Wichita, KS; 4Advent Health Porter, Denver, CO
Introduction: Alcoholic liver disease includes conditions from steatosis to cirrhosis and hepatocellular carcinoma. Severe alcohol-related hepatitis (SAH) is associated with high short-term mortality, particularly in patients unresponsive to medical therapy. While a 6-month abstinence period has traditionally been required before liver transplantation (LT), recent evidence suggests early LT may offer significant survival benefits. This review examines the outcomes of early LT in SAH.
Methods: We performed a comprehensive search of PubMed, the Cochrane Library and Embase through February 2025 for all published English language studies that investigated survival rates of early LT in SAH. Data from 9 studies were analyzed using R. The meta prop function estimated pooled survival proportions at 6 months, 1 year, 2 years, and 3 years. A random-effects model was used to account for variability. Heterogeneity was assessed using the I² statistic.
Results: Analysis included 376 patients with SAH who underwent early LT. The pooled survival proportion across all studies and time points for early LT was 0.916 (95% CI 0.8853; 0.9390) (I2 = 25.5%), indicating a high overall survival rate. The pooled survival proportion at 6-months was 0.9136 (95 CI 83.02%, 95.81%) (I2 = 34%), 1 year was 0.9321 (95% CI 0.8975, 0.9556) (I2 = 0%), 2 years was 0.9210 (95% CI 0.8436; 0.9618) (I2 = 4.6%) and 3 years was 0.9071 (95% CI 0.7519, 0.9692) (I2=50.8%).
Discussion: This systematic review analyzed 9 studies from 4 countries, evaluating early LT in 376 patients with SAH. Historically excluded from LT due to a required 6-month sobriety period, these high-risk patients (mean Maddrey Discriminate Function 79.4) had limited options beyond medical therapy. The review found significantly improved survival rates with early LT, regardless of varied inclusion criteria or demographics (mean age 46, 66% male). Ethical debates continue around relapse risk (28.2%) and fairness, though relapse was often minimal. Despite differences in study design and patient selection, survival outcomes remained consistent. Limitations include a lack of biopsy-confirmed diagnoses and limited long-term outcome data. However, findings support reevaluating current LT guidelines, advocating for earlier access to LT in select SAH patients, while highlighting the need for more long-term studies and integrated addiction care.
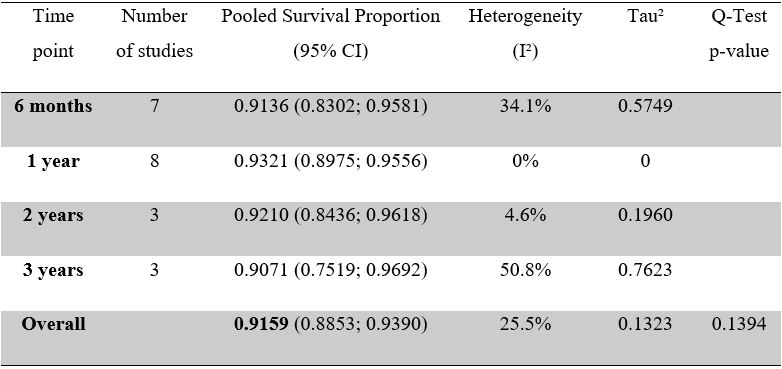
Figure: Table 1. Summary table of pooled survival proportion at all time points analyzed
Disclosures:
Meagan Phox indicated no relevant financial relationships.
Mohamed Omar indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
David Maundu indicated no relevant financial relationships.
Daly Al-Hadeethi indicated no relevant financial relationships.
Clark Kulig indicated no relevant financial relationships.
Nathan Tofteland indicated no relevant financial relationships.
Meagan H. Phox, DO1, Mohamed A. Omar, MD1, John Thesing, DO1, David Maundu, MBChB, MSc-HCM, MSc-ID2, Daly Al-Hadeethi, MD3, Clark Kulig, MD4, Nathan Tofteland, MD1. P1590 - Survival in Early Liver Transplantation in Severe Alcoholic Hepatitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2KU School of Medicine-Wichita, Wichita, KS; 3Wichita-KUMC, Wichita, KS; 4Advent Health Porter, Denver, CO
Introduction: Alcoholic liver disease includes conditions from steatosis to cirrhosis and hepatocellular carcinoma. Severe alcohol-related hepatitis (SAH) is associated with high short-term mortality, particularly in patients unresponsive to medical therapy. While a 6-month abstinence period has traditionally been required before liver transplantation (LT), recent evidence suggests early LT may offer significant survival benefits. This review examines the outcomes of early LT in SAH.
Methods: We performed a comprehensive search of PubMed, the Cochrane Library and Embase through February 2025 for all published English language studies that investigated survival rates of early LT in SAH. Data from 9 studies were analyzed using R. The meta prop function estimated pooled survival proportions at 6 months, 1 year, 2 years, and 3 years. A random-effects model was used to account for variability. Heterogeneity was assessed using the I² statistic.
Results: Analysis included 376 patients with SAH who underwent early LT. The pooled survival proportion across all studies and time points for early LT was 0.916 (95% CI 0.8853; 0.9390) (I2 = 25.5%), indicating a high overall survival rate. The pooled survival proportion at 6-months was 0.9136 (95 CI 83.02%, 95.81%) (I2 = 34%), 1 year was 0.9321 (95% CI 0.8975, 0.9556) (I2 = 0%), 2 years was 0.9210 (95% CI 0.8436; 0.9618) (I2 = 4.6%) and 3 years was 0.9071 (95% CI 0.7519, 0.9692) (I2=50.8%).
Discussion: This systematic review analyzed 9 studies from 4 countries, evaluating early LT in 376 patients with SAH. Historically excluded from LT due to a required 6-month sobriety period, these high-risk patients (mean Maddrey Discriminate Function 79.4) had limited options beyond medical therapy. The review found significantly improved survival rates with early LT, regardless of varied inclusion criteria or demographics (mean age 46, 66% male). Ethical debates continue around relapse risk (28.2%) and fairness, though relapse was often minimal. Despite differences in study design and patient selection, survival outcomes remained consistent. Limitations include a lack of biopsy-confirmed diagnoses and limited long-term outcome data. However, findings support reevaluating current LT guidelines, advocating for earlier access to LT in select SAH patients, while highlighting the need for more long-term studies and integrated addiction care.
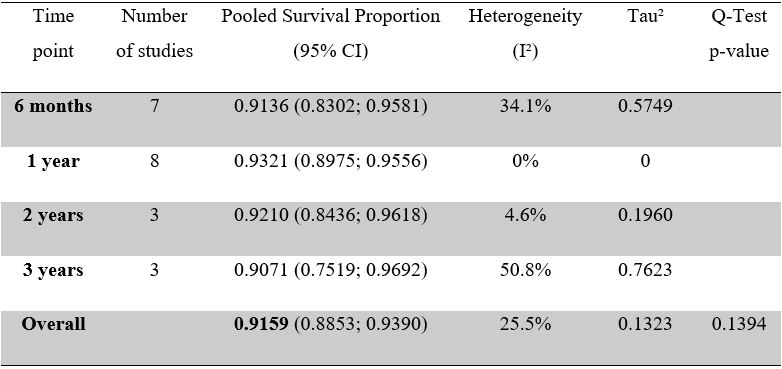
Figure: Table 1. Summary table of pooled survival proportion at all time points analyzed
Disclosures:
Meagan Phox indicated no relevant financial relationships.
Mohamed Omar indicated no relevant financial relationships.
John Thesing indicated no relevant financial relationships.
David Maundu indicated no relevant financial relationships.
Daly Al-Hadeethi indicated no relevant financial relationships.
Clark Kulig indicated no relevant financial relationships.
Nathan Tofteland indicated no relevant financial relationships.
Meagan H. Phox, DO1, Mohamed A. Omar, MD1, John Thesing, DO1, David Maundu, MBChB, MSc-HCM, MSc-ID2, Daly Al-Hadeethi, MD3, Clark Kulig, MD4, Nathan Tofteland, MD1. P1590 - Survival in Early Liver Transplantation in Severe Alcoholic Hepatitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
