Sunday Poster Session
Category: Liver
P1586 - Association of Liver Enzymes With 18FDG PET/CT Uptake in Sarcoidosis Patients
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- ZM
Zeel Modi, MD (she/her/hers)
University of Illinois
Chicago, IL
Presenting Author(s)
Zeel Modi, MD, Nadera Sweiss, MD, Adam E. Mikolajczyk, MD, Christen Vagts, MD, Christian Ascoli, MD
University of Illinois, Chicago, IL
Introduction: Hepatic involvement is a common sarcoidosis manifestation with clinically significant abnormalities, including portal hypertension and cirrhosis, seen in up to 25% of patients. However, despite this high prevalence, there are unclear guidelines on interpreting liver function tests (LFTs) and 18FDG PET/CT studies in hepatic sarcoidosis. In this pilot study, we assessed the predictive value of LFTs as biomarkers of hepatic sarcoidosis based on 18FDG liver uptake. We hypothesized that LFT abnormalities would correlate with hepatic 18FDG uptake when using a standardized blood pool (aorta) rather than liver as a reference background and could serve as a screening tool for hepatic sarcoidosis.
Methods: We retrospectively abstracted clinical and radiologic data on biopsy-confirmed sarcoidosis patients between 1/1/2015 and 12/31/2020. In total, 48 out of 288 patients with available 18FDG PET/CT studies were included and randomized into exploratory (n=24) and validation (n=24) cohorts. Patients with incomplete data or liver diseases other than sarcoidosis were excluded. LIFEx radiomic software (v7.8.0) was used to analyze 18FDG PET/CT studies, interpreting standardized uptake values (SUV) from the liver and aorta. Statistical analyses were performed using R and GraphPad.
Results: In the exploratory cohort, a significant relationship was noted within groups between Alkaline Phosphatase (ALP), but not ALT or AST, with SUV ratios. Specifically, those with elevated ALP levels had increased SUV ratios, while those with normal ALP had significantly lower SUV ratios (Mann-Whitney U test p < 0.005). Receiver operating characteristic analysis determined an optimal threshold ALP value (Y-Index) at 86.5 U/L (Figure A), which effectively stratified patients with elevated hepatic 18FDG uptake. Application of the Y-Index threshold value for ALP to the validation cohort demonstrated a statistically significant difference in the SUV ratios between the normal and elevated ALP cohorts (Figure B).
Discussion: Although further investigation is warranted, our study demonstrates an association between ALP levels and hepatic 18FDG uptake using a standardized blood pool reference with the LIFEx radiomic software. Our findings suggest that ALP, when assessed using a modified threshold, may serve as a clinically relevant biomarker for identifying hepatic involvement in sarcoidosis. Recognition of elevated ALP on routine laboratory testing could prompt earlier imaging and/or biopsy for confirmation of hepatic sarcoidosis.
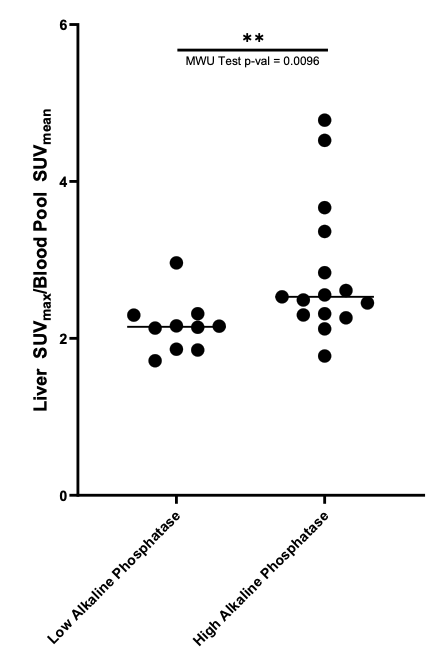
Figure: Figure A: Receiver Operating Characteristic (ROC) analysis applied to the exploratory cohort demonstrates that ALP level provides diagnostic insight for hepatic sarcoidosis. A Y-index threshold of 86.5 U/L was determined as the optimal cutoff value to discriminate low vs. high hepatic 18FDG uptake.
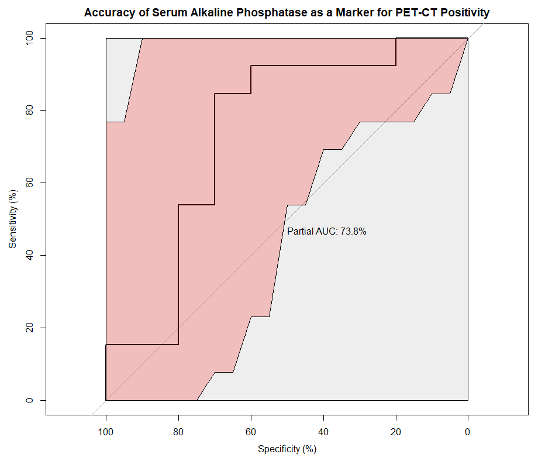
Figure: Figure B: Association between low vs. high ALP levels based on Y-Index threshold and SUV ratios in the validation cohort. High ALP levels are noted to be related to a significantly higher SUV ratio.
Disclosures:
Zeel Modi indicated no relevant financial relationships.
Nadera Sweiss indicated no relevant financial relationships.
Adam Mikolajczyk indicated no relevant financial relationships.
Christen Vagts indicated no relevant financial relationships.
Christian Ascoli indicated no relevant financial relationships.
Zeel Modi, MD, Nadera Sweiss, MD, Adam E. Mikolajczyk, MD, Christen Vagts, MD, Christian Ascoli, MD. P1586 - Association of Liver Enzymes With 18FDG PET/CT Uptake in Sarcoidosis Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Illinois, Chicago, IL
Introduction: Hepatic involvement is a common sarcoidosis manifestation with clinically significant abnormalities, including portal hypertension and cirrhosis, seen in up to 25% of patients. However, despite this high prevalence, there are unclear guidelines on interpreting liver function tests (LFTs) and 18FDG PET/CT studies in hepatic sarcoidosis. In this pilot study, we assessed the predictive value of LFTs as biomarkers of hepatic sarcoidosis based on 18FDG liver uptake. We hypothesized that LFT abnormalities would correlate with hepatic 18FDG uptake when using a standardized blood pool (aorta) rather than liver as a reference background and could serve as a screening tool for hepatic sarcoidosis.
Methods: We retrospectively abstracted clinical and radiologic data on biopsy-confirmed sarcoidosis patients between 1/1/2015 and 12/31/2020. In total, 48 out of 288 patients with available 18FDG PET/CT studies were included and randomized into exploratory (n=24) and validation (n=24) cohorts. Patients with incomplete data or liver diseases other than sarcoidosis were excluded. LIFEx radiomic software (v7.8.0) was used to analyze 18FDG PET/CT studies, interpreting standardized uptake values (SUV) from the liver and aorta. Statistical analyses were performed using R and GraphPad.
Results: In the exploratory cohort, a significant relationship was noted within groups between Alkaline Phosphatase (ALP), but not ALT or AST, with SUV ratios. Specifically, those with elevated ALP levels had increased SUV ratios, while those with normal ALP had significantly lower SUV ratios (Mann-Whitney U test p < 0.005). Receiver operating characteristic analysis determined an optimal threshold ALP value (Y-Index) at 86.5 U/L (Figure A), which effectively stratified patients with elevated hepatic 18FDG uptake. Application of the Y-Index threshold value for ALP to the validation cohort demonstrated a statistically significant difference in the SUV ratios between the normal and elevated ALP cohorts (Figure B).
Discussion: Although further investigation is warranted, our study demonstrates an association between ALP levels and hepatic 18FDG uptake using a standardized blood pool reference with the LIFEx radiomic software. Our findings suggest that ALP, when assessed using a modified threshold, may serve as a clinically relevant biomarker for identifying hepatic involvement in sarcoidosis. Recognition of elevated ALP on routine laboratory testing could prompt earlier imaging and/or biopsy for confirmation of hepatic sarcoidosis.
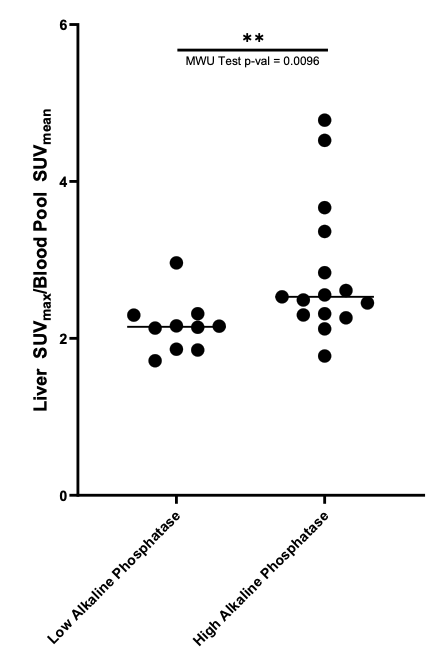
Figure: Figure A: Receiver Operating Characteristic (ROC) analysis applied to the exploratory cohort demonstrates that ALP level provides diagnostic insight for hepatic sarcoidosis. A Y-index threshold of 86.5 U/L was determined as the optimal cutoff value to discriminate low vs. high hepatic 18FDG uptake.
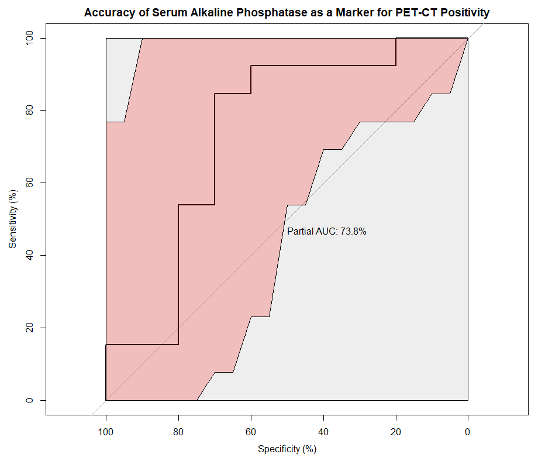
Figure: Figure B: Association between low vs. high ALP levels based on Y-Index threshold and SUV ratios in the validation cohort. High ALP levels are noted to be related to a significantly higher SUV ratio.
Disclosures:
Zeel Modi indicated no relevant financial relationships.
Nadera Sweiss indicated no relevant financial relationships.
Adam Mikolajczyk indicated no relevant financial relationships.
Christen Vagts indicated no relevant financial relationships.
Christian Ascoli indicated no relevant financial relationships.
Zeel Modi, MD, Nadera Sweiss, MD, Adam E. Mikolajczyk, MD, Christen Vagts, MD, Christian Ascoli, MD. P1586 - Association of Liver Enzymes With 18FDG PET/CT Uptake in Sarcoidosis Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

