Sunday Poster Session
Category: Liver
P1585 - Characteristics of Individuals Aged 70 Years or Greater Evaluated for Liver Transplantation: A Single Center Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- BM
Bridgette B. McNally, DO
Mayo Clinic
Phoenix, AZ
Presenting Author(s)
Bridgette B. McNally, DO, Elizabeth Carey, MD
Mayo Clinic, Phoenix, AZ
Introduction: The rate of liver transplantation in patients over sixty-five is rising and about 20 percent of the US population is projected to be over age sixty-five in 2030. The rise in transplantation is due to an increased incidence in metabolic dysfunction-associated steototic liver disease (MASLD) and hepatocellular carcinoma (HCC). Previous studies on liver transplantation in patients over 65 years have shown an increased morbidity and mortality compared to younger groups. Our study investigated the demographic and clinical characteristics of patients aged seventy or older who were evaluated for liver transplantation.
Methods: A retrospective chart review of all patients aged seventy or older who were evaluated for liver transplantation at a single center was conducted. Descriptive statistical analysis was performed.
Results: A total of 138 patients aged 70 or older were evaluated for liver transplantation. 78 patients were listed for transplantation and 60 were denied. The most common reasons for denial were the presence of comorbidities, HCC outside the parameters for transplantation and frailty. Age and BMI were similar in those listed vs denied. Autoimmune liver disease was significantly higher in patients denied transplant. There was no significant difference between MELD 3.0 or Six Minute Walk Duration in those listed vs denied. However, the Standford Integrated Psychosocial Assessment for Transplantation (SPIAT), which predicts negative post transplant psychosocial and medical outcomes, was significantly higher in those denied. There was no significant difference in rates of HCC in those listed vs denied. Concomitant coronary artery disease was significantly higher in those denied transplant.
Discussion: We have demonstrated that a comprehensive evaluation that not only considers the indication for transplantation, presence of malignancy and other comorbidities is paramount to identify those appropriate for transplantation. Similarly, objective measures of frailty are valuable given the high incidence of denial related to underlying frailty. SIPAT scores were higher in those denied transplantation, indicating that this score is important when considering the psychosocial implications of transplantation in the elderly population. Further studies are needed to directly compare all ages of patients who are evaluated for liver transplantation as a rise in the need for transplantation in those over age 65 is expected.
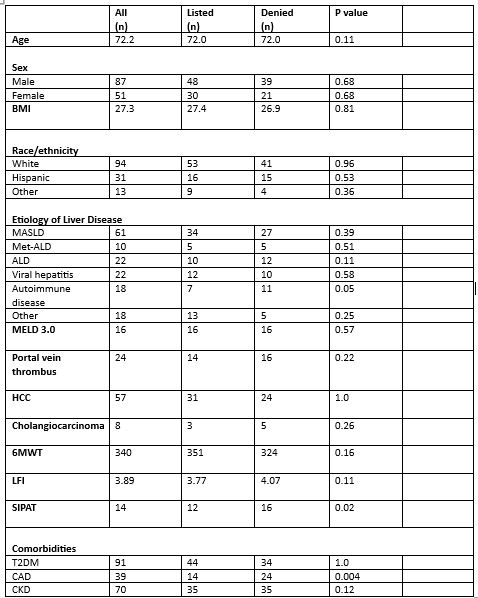
Figure: Table 1. Demographics
Caption: Metabolic Alcohol-Related Liver Disease (Met-ALD), Alcohol Related Liver Disease (ALD), Six Minute Walk Test (6MWT), Liver Frailty Index (LFI), Type 2 Diabetes Mellitus (T2DM), Coronary Artery Disease (CAD), Chronic Kidney Disease (CKD)
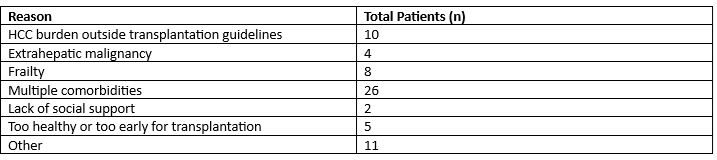
Figure: Table 2. Reasons for Denial of Liver Transplantation
Disclosures:
Bridgette McNally indicated no relevant financial relationships.
Elizabeth Carey: GlaxoSmithKline – Advisory Committee/Board Member.
Bridgette B. McNally, DO, Elizabeth Carey, MD. P1585 - Characteristics of Individuals Aged 70 Years or Greater Evaluated for Liver Transplantation: A Single Center Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mayo Clinic, Phoenix, AZ
Introduction: The rate of liver transplantation in patients over sixty-five is rising and about 20 percent of the US population is projected to be over age sixty-five in 2030. The rise in transplantation is due to an increased incidence in metabolic dysfunction-associated steototic liver disease (MASLD) and hepatocellular carcinoma (HCC). Previous studies on liver transplantation in patients over 65 years have shown an increased morbidity and mortality compared to younger groups. Our study investigated the demographic and clinical characteristics of patients aged seventy or older who were evaluated for liver transplantation.
Methods: A retrospective chart review of all patients aged seventy or older who were evaluated for liver transplantation at a single center was conducted. Descriptive statistical analysis was performed.
Results: A total of 138 patients aged 70 or older were evaluated for liver transplantation. 78 patients were listed for transplantation and 60 were denied. The most common reasons for denial were the presence of comorbidities, HCC outside the parameters for transplantation and frailty. Age and BMI were similar in those listed vs denied. Autoimmune liver disease was significantly higher in patients denied transplant. There was no significant difference between MELD 3.0 or Six Minute Walk Duration in those listed vs denied. However, the Standford Integrated Psychosocial Assessment for Transplantation (SPIAT), which predicts negative post transplant psychosocial and medical outcomes, was significantly higher in those denied. There was no significant difference in rates of HCC in those listed vs denied. Concomitant coronary artery disease was significantly higher in those denied transplant.
Discussion: We have demonstrated that a comprehensive evaluation that not only considers the indication for transplantation, presence of malignancy and other comorbidities is paramount to identify those appropriate for transplantation. Similarly, objective measures of frailty are valuable given the high incidence of denial related to underlying frailty. SIPAT scores were higher in those denied transplantation, indicating that this score is important when considering the psychosocial implications of transplantation in the elderly population. Further studies are needed to directly compare all ages of patients who are evaluated for liver transplantation as a rise in the need for transplantation in those over age 65 is expected.
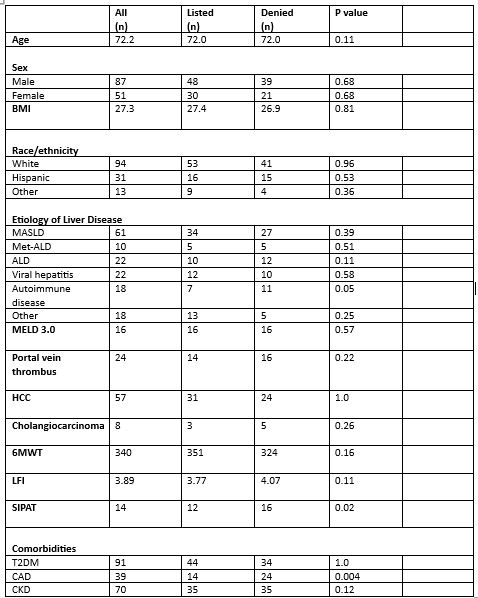
Figure: Table 1. Demographics
Caption: Metabolic Alcohol-Related Liver Disease (Met-ALD), Alcohol Related Liver Disease (ALD), Six Minute Walk Test (6MWT), Liver Frailty Index (LFI), Type 2 Diabetes Mellitus (T2DM), Coronary Artery Disease (CAD), Chronic Kidney Disease (CKD)
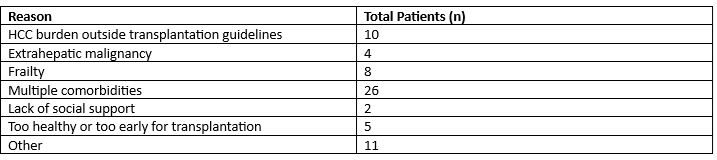
Figure: Table 2. Reasons for Denial of Liver Transplantation
Disclosures:
Bridgette McNally indicated no relevant financial relationships.
Elizabeth Carey: GlaxoSmithKline – Advisory Committee/Board Member.
Bridgette B. McNally, DO, Elizabeth Carey, MD. P1585 - Characteristics of Individuals Aged 70 Years or Greater Evaluated for Liver Transplantation: A Single Center Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
