Sunday Poster Session
Category: Liver
P1514 - Evaluating FIB-4 Performance and Equity Gaps in Liver Risk Stratification: A Retrospective Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Lan Nguyen, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Lan Nguyen, DO1, Nariman Hossein-Javaheri, DO1, Blake Podger, MD1, Courtney Dennis, DO1, Xavier Zonna, DO1, Mohammed Ayyad, MD2, Renata Anand, MD1
1University at Buffalo, Buffalo, NY; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is common among individuals with obesity and metabolic comorbidities. The FIB-4 index is increasingly used in primary care setting as a non-invasive method for liver fibrosis risk stratification. However, its accuracy and consistency across demographic groups remain unclear. Our study therefore evaluated the associations of FIB-4 risk classification with different genders, primary languages, and races/ethnicities.
Methods: We conducted a retrospective analysis of 510 adults with obesity (BMI > 30) and at least one metabolic comorbidity seen at a primary care clinic. FIB-4 indexes were calculated and categorized using age-adjusted thresholds: for those < 65 years, low risk was < 1.3 and intermediate risk was 1.3-2.67; for those ≥65 years, low risk was < 2.0 and intermediate risk was 2.0-2.67. High risk was defined as >2.67 for all ages. Multivariable logistic regression models were used to evaluate associations between demographic factors (gender, primary language, and race/ethnicity) and fibrosis risk categories.
Results: Male patients had significantly greater odds of high-risk classification (OR=2.72, p=0.016). Spanish-speaking individuals were less likely to be low risk (OR=0.25, p=0.011) and more likely to be classified as intermediate risk (OR=4.39, p=0.009). Findings for Bengali and Arabic speakers were not obtainable due to small sample sizes. Despite well-established higher MASLD burden in Hispanic patients, they had significantly greater odds of low-risk classification compared to White patients (OR=4.02, p=0.037), with a similar but nonsignificant trend versus Black patients (OR=3.62, p=0.062). No significant trends were observed for Black or Asian patients.
Discussion: Higher FIB-4 indexes among men likely reflect true biological differences in fibrosis risk. Since the MASLD burden in Spanish-speaking population remains poorly characterized, their lower likelihood of low-risk classification and greater odds of intermediate risk may stem from baseline risk, language barriers that hinder care, or socioeconomic disparities. Interestingly, the low-risk classification among Hispanic patients may reflect the underutilization of fibrosis testing or the “healthy immigrant effect”. This finding also highlights potential variability in the performance of FIB-4 index across racial/ethnic groups, emphasizing the need for further validation in diverse populations to ensure equitable and accurate liver disease assessment.
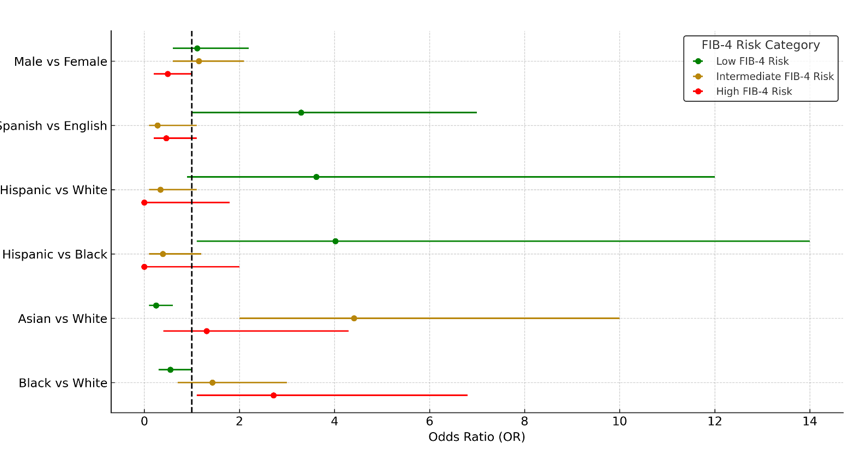
Figure: Table 1. Summary of associations between FIB-4 index classifications (low, intermediate, high) and demographic factors (with indicated reference groups). “N/A” indicates insufficient sample size for reliable estimation.
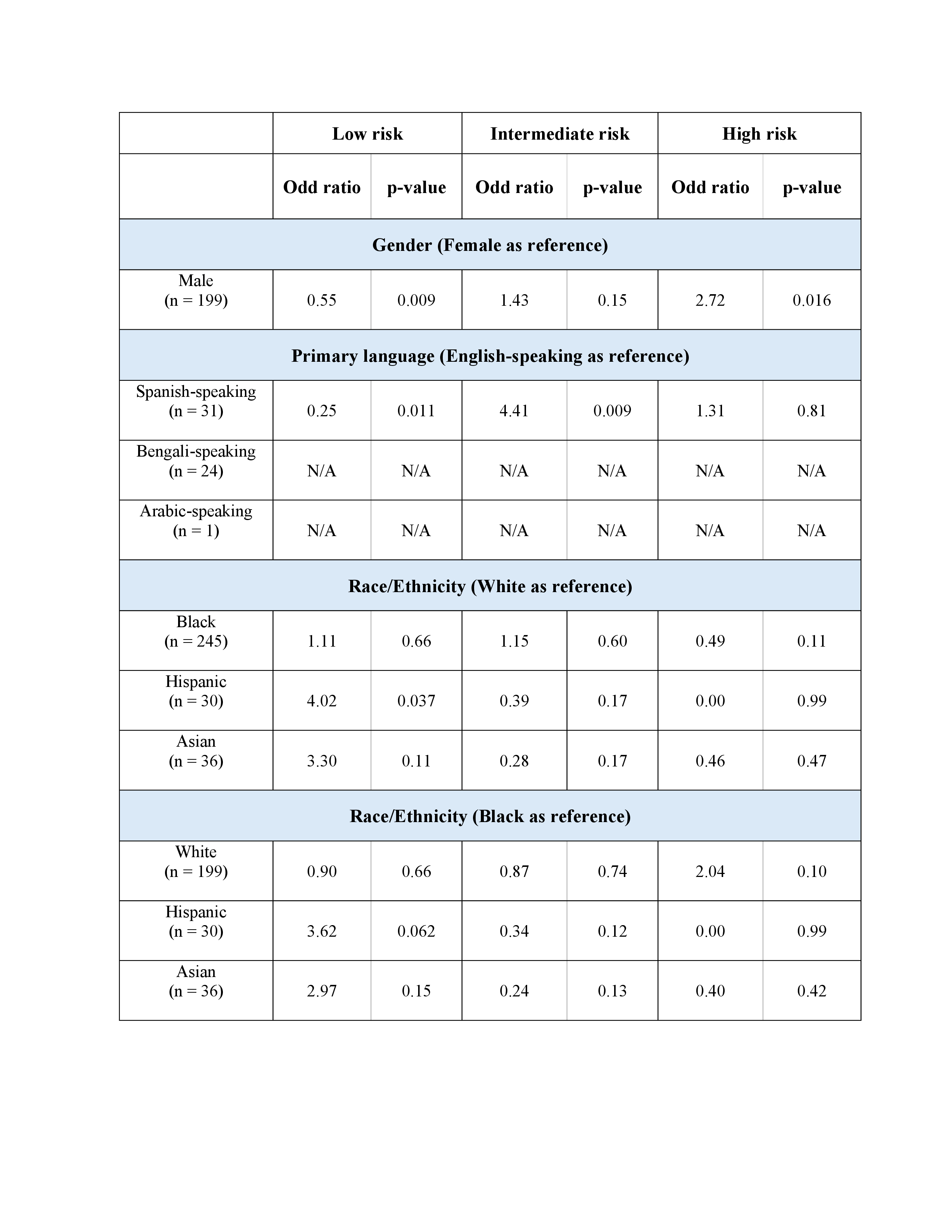
Figure: Figure 1. Forrest plot of adjusted odds ratios for FIB-4 risk categories by gender, primary language, and race/ethnicity
Disclosures:
Lan Nguyen indicated no relevant financial relationships.
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Blake Podger indicated no relevant financial relationships.
Courtney Dennis indicated no relevant financial relationships.
Xavier Zonna indicated no relevant financial relationships.
Mohammed Ayyad indicated no relevant financial relationships.
Renata Anand indicated no relevant financial relationships.
Lan Nguyen, DO1, Nariman Hossein-Javaheri, DO1, Blake Podger, MD1, Courtney Dennis, DO1, Xavier Zonna, DO1, Mohammed Ayyad, MD2, Renata Anand, MD1. P1514 - Evaluating FIB-4 Performance and Equity Gaps in Liver Risk Stratification: A Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is common among individuals with obesity and metabolic comorbidities. The FIB-4 index is increasingly used in primary care setting as a non-invasive method for liver fibrosis risk stratification. However, its accuracy and consistency across demographic groups remain unclear. Our study therefore evaluated the associations of FIB-4 risk classification with different genders, primary languages, and races/ethnicities.
Methods: We conducted a retrospective analysis of 510 adults with obesity (BMI > 30) and at least one metabolic comorbidity seen at a primary care clinic. FIB-4 indexes were calculated and categorized using age-adjusted thresholds: for those < 65 years, low risk was < 1.3 and intermediate risk was 1.3-2.67; for those ≥65 years, low risk was < 2.0 and intermediate risk was 2.0-2.67. High risk was defined as >2.67 for all ages. Multivariable logistic regression models were used to evaluate associations between demographic factors (gender, primary language, and race/ethnicity) and fibrosis risk categories.
Results: Male patients had significantly greater odds of high-risk classification (OR=2.72, p=0.016). Spanish-speaking individuals were less likely to be low risk (OR=0.25, p=0.011) and more likely to be classified as intermediate risk (OR=4.39, p=0.009). Findings for Bengali and Arabic speakers were not obtainable due to small sample sizes. Despite well-established higher MASLD burden in Hispanic patients, they had significantly greater odds of low-risk classification compared to White patients (OR=4.02, p=0.037), with a similar but nonsignificant trend versus Black patients (OR=3.62, p=0.062). No significant trends were observed for Black or Asian patients.
Discussion: Higher FIB-4 indexes among men likely reflect true biological differences in fibrosis risk. Since the MASLD burden in Spanish-speaking population remains poorly characterized, their lower likelihood of low-risk classification and greater odds of intermediate risk may stem from baseline risk, language barriers that hinder care, or socioeconomic disparities. Interestingly, the low-risk classification among Hispanic patients may reflect the underutilization of fibrosis testing or the “healthy immigrant effect”. This finding also highlights potential variability in the performance of FIB-4 index across racial/ethnic groups, emphasizing the need for further validation in diverse populations to ensure equitable and accurate liver disease assessment.
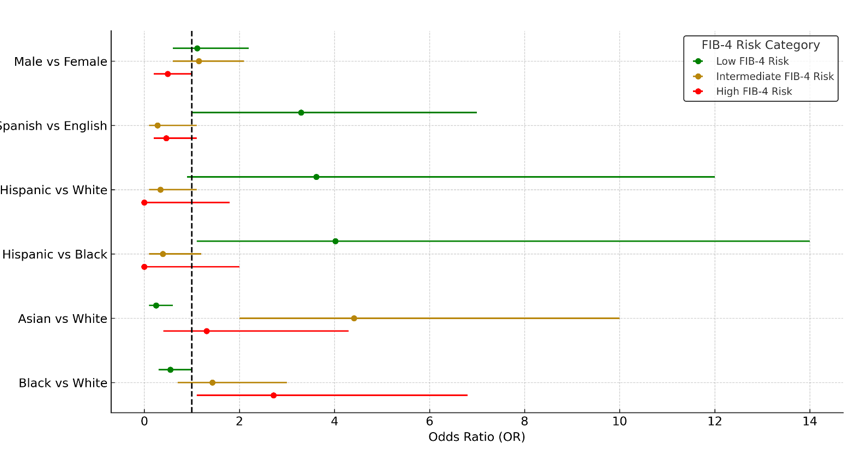
Figure: Table 1. Summary of associations between FIB-4 index classifications (low, intermediate, high) and demographic factors (with indicated reference groups). “N/A” indicates insufficient sample size for reliable estimation.
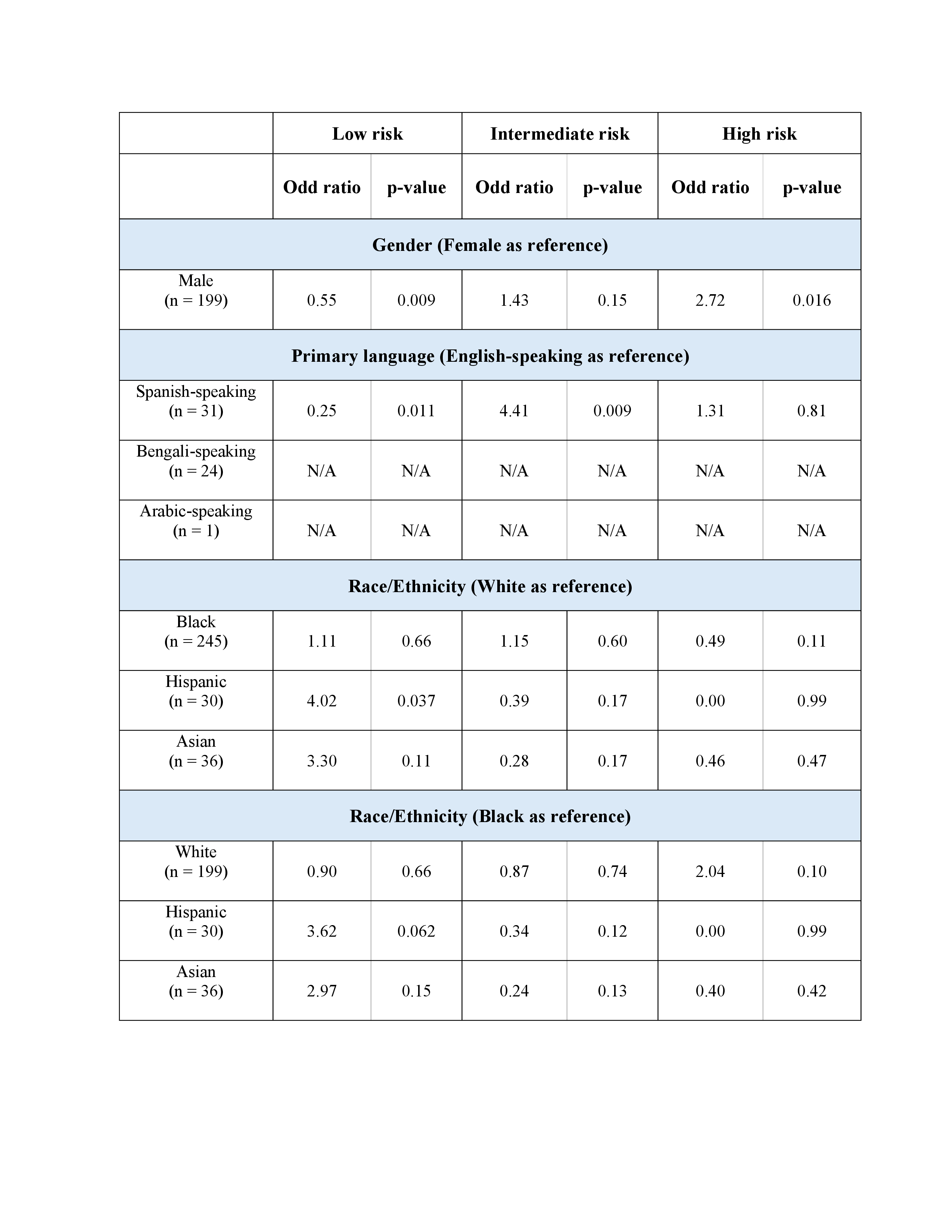
Figure: Figure 1. Forrest plot of adjusted odds ratios for FIB-4 risk categories by gender, primary language, and race/ethnicity
Disclosures:
Lan Nguyen indicated no relevant financial relationships.
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Blake Podger indicated no relevant financial relationships.
Courtney Dennis indicated no relevant financial relationships.
Xavier Zonna indicated no relevant financial relationships.
Mohammed Ayyad indicated no relevant financial relationships.
Renata Anand indicated no relevant financial relationships.
Lan Nguyen, DO1, Nariman Hossein-Javaheri, DO1, Blake Podger, MD1, Courtney Dennis, DO1, Xavier Zonna, DO1, Mohammed Ayyad, MD2, Renata Anand, MD1. P1514 - Evaluating FIB-4 Performance and Equity Gaps in Liver Risk Stratification: A Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
