Sunday Poster Session
Category: Liver
P1507 - Racial, Ethnic, and Sex-Based Disparities in Met-ALD: A 10-Year Propensity Score Matched Analysis Utilizing a National Database
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Himsikhar Khataniar, MD (he/him/his)
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Himsikhar Khataniar, MD1, Kaitlyn Gernhard, DO2, Hany Habib, MD3, Nikki Duong, MD4
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3Allegheny Health Network Medicine Institute, Pittsburgh, PA; 4Stanford University, Stanford, CA
Introduction: Metabolic dysfunction–associated alcohol-related liver disease (Met-ALD) describes MASLD in individuals whose alcohol intake exceeds guideline thresholds. Black and Hispanic populations already carry a disproportionate MASLD burden, yet cardiovascular and hepatic risks across race, sex and ethnicity in Met-ALD remain poorly defined.
Methods: Adults with Met-ALD recorded in the U.S. TriNetX electronic-health-record network (2010-2020) were identified by AASLD criteria. Patients with pre-existing major adverse cardiovascular events (MACE), major adverse liver outcomes (MALO), liver transplant, or viral/cholestatic liver disease were excluded. Propensity-score matching (1:1) balanced age, sex, race, BMI, comorbidities, tobacco and alcohol use, cardiovascular medications, bariatric surgery, GLP-1 agonist and insulin exposure. Five-year MACE and MALO were primary endpoints; myocardial infarction, stroke, acute heart failure, decompensated cirrhosis, hepatocellular carcinoma (HCC), liver transplant, all-cause death and hospitalization were secondary.
Results: Fifty-eight thousand one hundred thirteen patients met inclusion (mean age 54 ± 14 yr; 64.8% male; 68.4% White; 10.3 % Hispanic). Compared with Whites, Blacks had higher odds of MACE (adjusted odds ratio [aOR] 1.13, 95 % CI 1.01–1.25) and stroke (aOR 1.45, 1.20–1.76), whereas Asians had lower five-year mortality (aOR 0.60, 0.38–0.97). Male sex predicted greater risks of MACE (aOR 1.17, 1.07–1.27), heart failure (aOR 1.20, 1.04–1.39) and death (aOR 1.13, 1.03–1.25) but lower MALO (aOR 0.89, 0.74–0.97) than female sex. Hispanics experienced reduced MACE (aOR 0.85, 0.72–1.00), decompensated cirrhosis (aOR 0.67, 0.51–0.88) and mortality (aOR 0.66, 0.54–0.79) versus non-Hispanics, with no ethnicity-based differences in MALO, HCC or transplant.
Discussion: Black race and male sex independently confer excess cardiovascular morbidity and mortality in Met-ALD, whereas Hispanic ethnicity shows a paradoxical survival and hepatic advantage; Asian race associates with lower mortality. Clarifying biological, behavioural and care-access mechanisms underlying these trajectories is essential to develop equitable, culturally responsive prevention and treatment strategies.
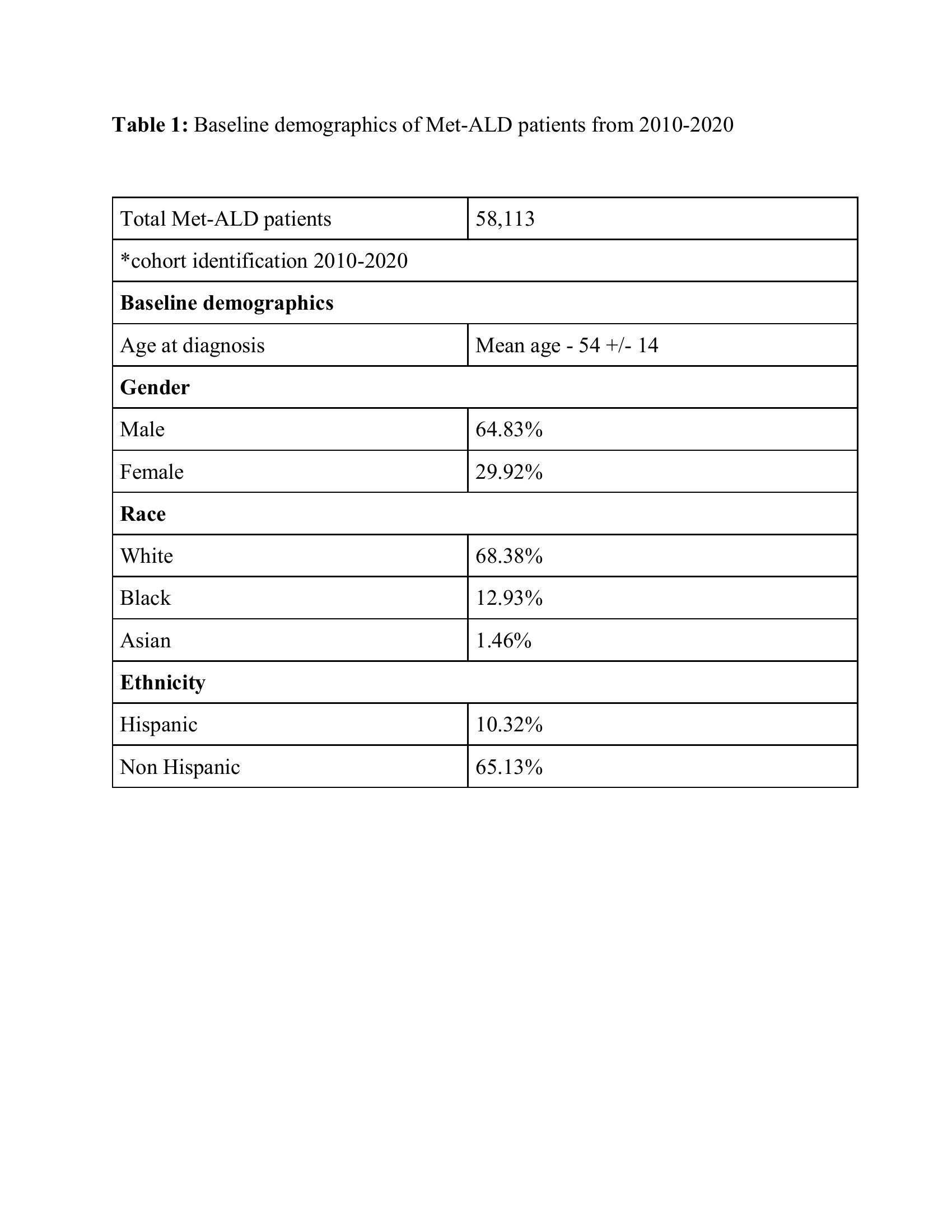
Figure: Table 1: Baseline demographics of Met-ALD patients from 2010-2020
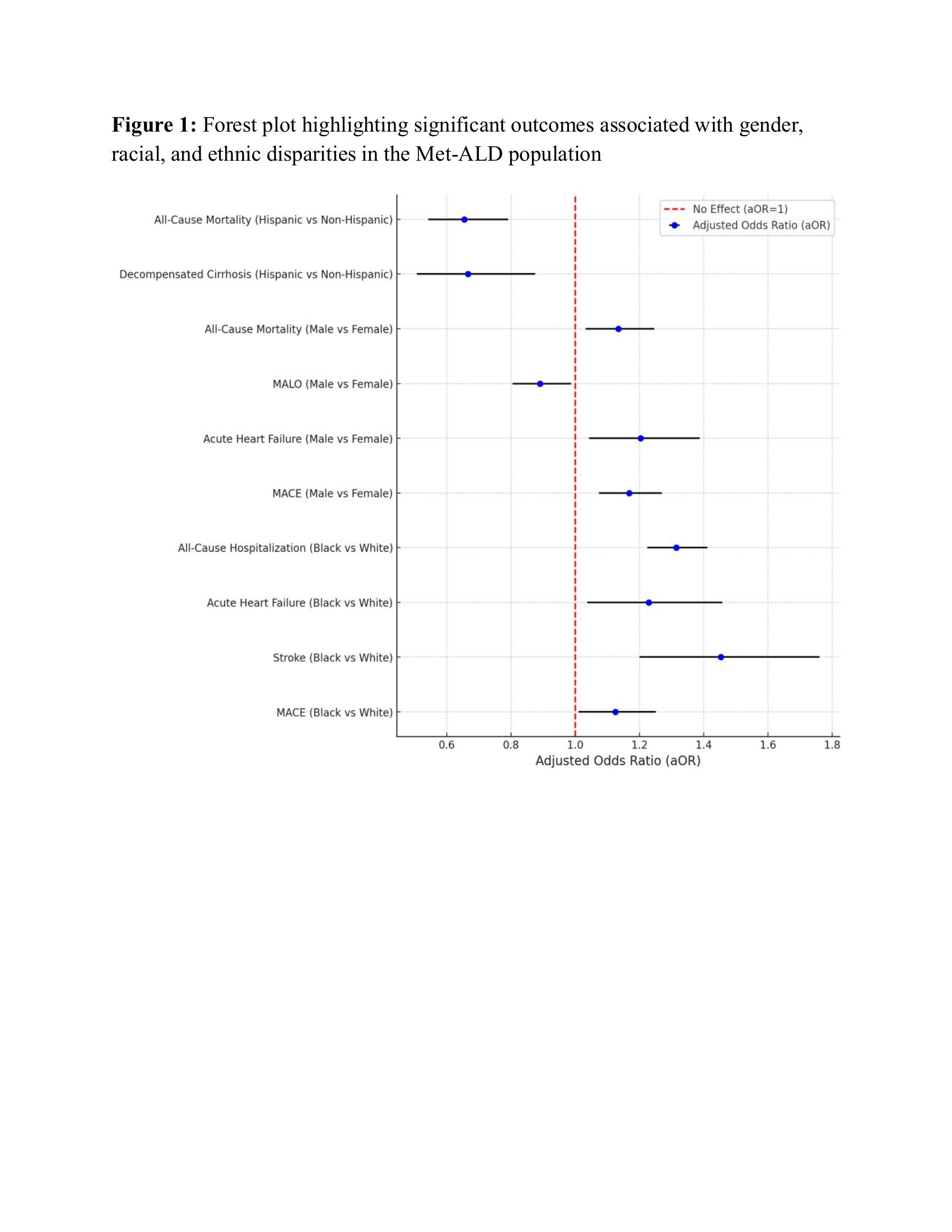
Figure: Figure 1: Forest plot highlighting significant outcomes associated with gender, racial, and ethnic disparities in the Met-ALD population
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Hany Habib indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Himsikhar Khataniar, MD1, Kaitlyn Gernhard, DO2, Hany Habib, MD3, Nikki Duong, MD4. P1507 - Racial, Ethnic, and Sex-Based Disparities in Met-ALD: A 10-Year Propensity Score Matched Analysis Utilizing a National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3Allegheny Health Network Medicine Institute, Pittsburgh, PA; 4Stanford University, Stanford, CA
Introduction: Metabolic dysfunction–associated alcohol-related liver disease (Met-ALD) describes MASLD in individuals whose alcohol intake exceeds guideline thresholds. Black and Hispanic populations already carry a disproportionate MASLD burden, yet cardiovascular and hepatic risks across race, sex and ethnicity in Met-ALD remain poorly defined.
Methods: Adults with Met-ALD recorded in the U.S. TriNetX electronic-health-record network (2010-2020) were identified by AASLD criteria. Patients with pre-existing major adverse cardiovascular events (MACE), major adverse liver outcomes (MALO), liver transplant, or viral/cholestatic liver disease were excluded. Propensity-score matching (1:1) balanced age, sex, race, BMI, comorbidities, tobacco and alcohol use, cardiovascular medications, bariatric surgery, GLP-1 agonist and insulin exposure. Five-year MACE and MALO were primary endpoints; myocardial infarction, stroke, acute heart failure, decompensated cirrhosis, hepatocellular carcinoma (HCC), liver transplant, all-cause death and hospitalization were secondary.
Results: Fifty-eight thousand one hundred thirteen patients met inclusion (mean age 54 ± 14 yr; 64.8% male; 68.4% White; 10.3 % Hispanic). Compared with Whites, Blacks had higher odds of MACE (adjusted odds ratio [aOR] 1.13, 95 % CI 1.01–1.25) and stroke (aOR 1.45, 1.20–1.76), whereas Asians had lower five-year mortality (aOR 0.60, 0.38–0.97). Male sex predicted greater risks of MACE (aOR 1.17, 1.07–1.27), heart failure (aOR 1.20, 1.04–1.39) and death (aOR 1.13, 1.03–1.25) but lower MALO (aOR 0.89, 0.74–0.97) than female sex. Hispanics experienced reduced MACE (aOR 0.85, 0.72–1.00), decompensated cirrhosis (aOR 0.67, 0.51–0.88) and mortality (aOR 0.66, 0.54–0.79) versus non-Hispanics, with no ethnicity-based differences in MALO, HCC or transplant.
Discussion: Black race and male sex independently confer excess cardiovascular morbidity and mortality in Met-ALD, whereas Hispanic ethnicity shows a paradoxical survival and hepatic advantage; Asian race associates with lower mortality. Clarifying biological, behavioural and care-access mechanisms underlying these trajectories is essential to develop equitable, culturally responsive prevention and treatment strategies.
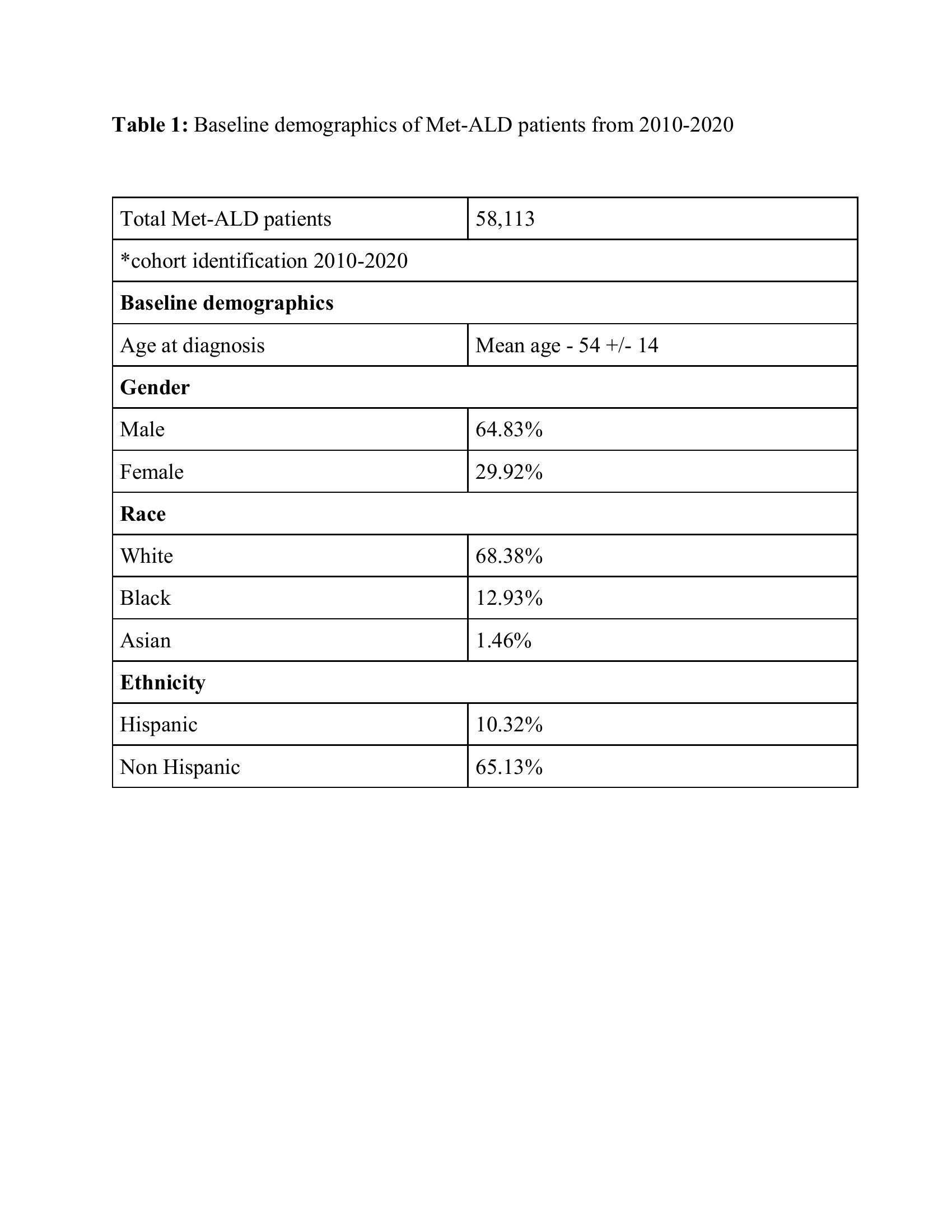
Figure: Table 1: Baseline demographics of Met-ALD patients from 2010-2020
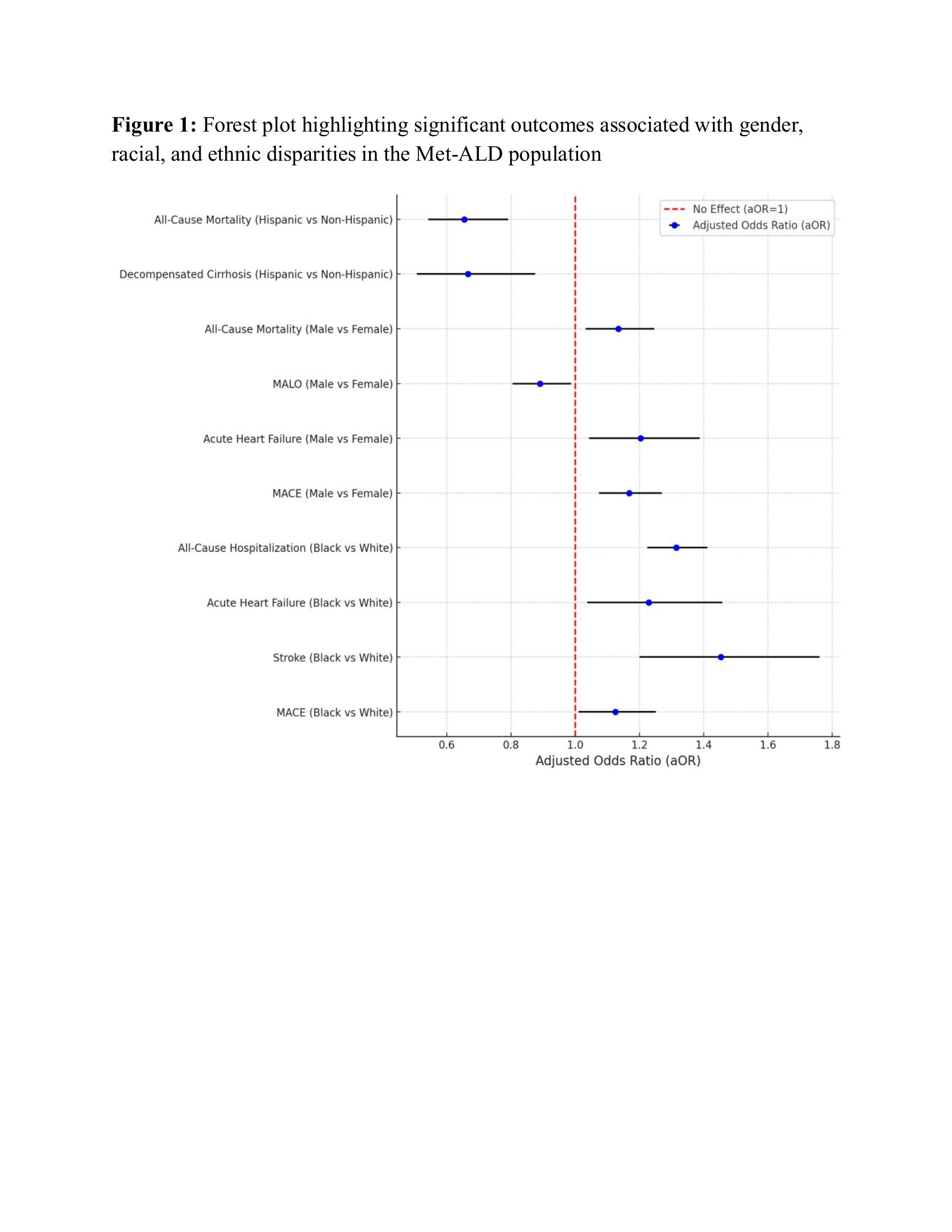
Figure: Figure 1: Forest plot highlighting significant outcomes associated with gender, racial, and ethnic disparities in the Met-ALD population
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Hany Habib indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Himsikhar Khataniar, MD1, Kaitlyn Gernhard, DO2, Hany Habib, MD3, Nikki Duong, MD4. P1507 - Racial, Ethnic, and Sex-Based Disparities in Met-ALD: A 10-Year Propensity Score Matched Analysis Utilizing a National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
