Sunday Poster Session
Category: Liver
P1506 - Beyond Varices: The Cardiovascular Impact of Non-Selective Beta-Blockers in Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Eunice Omeludike, MD (she/her/hers)
Piedmont Athens Regional Medical Centre
Athens, GA
Presenting Author(s)
Eunice Omeludike, MD1, Babajide Obidigbo, MBBS2, Abdul-Rahaman A. Ottun, MD3, Eunice Aregbesola, MD4, Cherechi Nwabueze, MBBS, MPH5, Ooreoluwa Fasola, MD6, Sarpong Boateng, MD, MPH7, Samuel Acheampong, MD, MSc3, Elizabeth Soladoye, MD, MPH3, Chisom Nwaneki, MD, MPH8, Papa K. Beeko, MBChB3, Brice Njobe, MD, MPH9
1Piedmont Athens Regional Medical Centre, Athens, GA; 2York and Scaborough NHS Foundation Trust, Scaborough, England, United Kingdom; 3Piedmont Athens Regional, Athens, GA; 4University of Missouri Health Care, Columbia, MO; 5John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 6Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX; 7Yale New Haven Health, Bridgeport, CT; 8Saint Peter's University Hospital, New Brunswick, NJ, New Brunswick, NJ; 9Piedmont Athens Regional Medical center, Athens, GA
Introduction: Patients with cirrhosis and portal hypertension are at elevated cardiovascular risk due to systemic inflammation, autonomic imbalance, and hemodynamic alterations. Non-selective beta-blockers (NSBBs), routinely used to prevent variceal bleeding, may also influence cardiovascular outcomes.
Methods: We conducted a systematic review and meta-analysis using the PRISMA guidelines. Literature
searches were performed across PubMed, Embase, and Cochrane Library through February 2025
for studies assessing cardiovascular outcomes in adults with cirrhosis and clinically significant
portal hypertension on long-term NSBB therapy (propranolol, nadolol, or carvedilol) versus no
NSBBs. The primary outcome was major adverse cardiovascular events (MACE: myocardial
infarction, stroke, cardiovascular death). Secondary outcomes included all-cause mortality and
heart failure hospitalization. Ten eligible studies (N = 18,612 patients), including two
randomized controlled trials and eight observational cohorts, were included. Data were pooled
using a random-effects model, and heterogeneity was quantified using the I² statistic. The risk of bias was assessed
using the Newcastle–Ottawa Scale for cohorts and the Cochrane Risk of Bias 2 tool for RCTs.
Results: Pooled analysis showed that NSBB use was associated with a statistically significant reduction in MACE (RR = 0.79, 95% CI: 0.68–0.91; p = 0.001; I² = 41%) and all-cause mortality (RR = 0.83,95% CI: 0.74–0.94; p = 0.004; I² = 52%). No significant difference was observed in heart failure hospitalizations (RR = 1.06, 95% CI: 0.89–1.26; p = 0.51; I² = 35%). Subgroup analyses by age, MELD score, and diabetes status confirmed the cardioprotective trend. Sensitivity analyses and leave-one-out tests confirmed robustness. Funnel plot and Egger's test showed minimal publication bias. Figure 1 presents the forest plot summarizing the relative risks of major adverse cardiovascular events (MACE) across the included studies.
Discussion: Our meta-analysis provides pooled evidence supporting the cardiovascular benefit of NSBBs in patients with cirrhosis and portal hypertension. NSBBs are associated with a lower risk of MACE and mortality without increasing heart failure admissions. These findings suggest that NSBBs may serve a dual protective role—reducing both portal pressures and cardiovascular burden. While RCTs strengthen the conclusions, larger prospective trials remain necessary to confirm causality and guide practice.
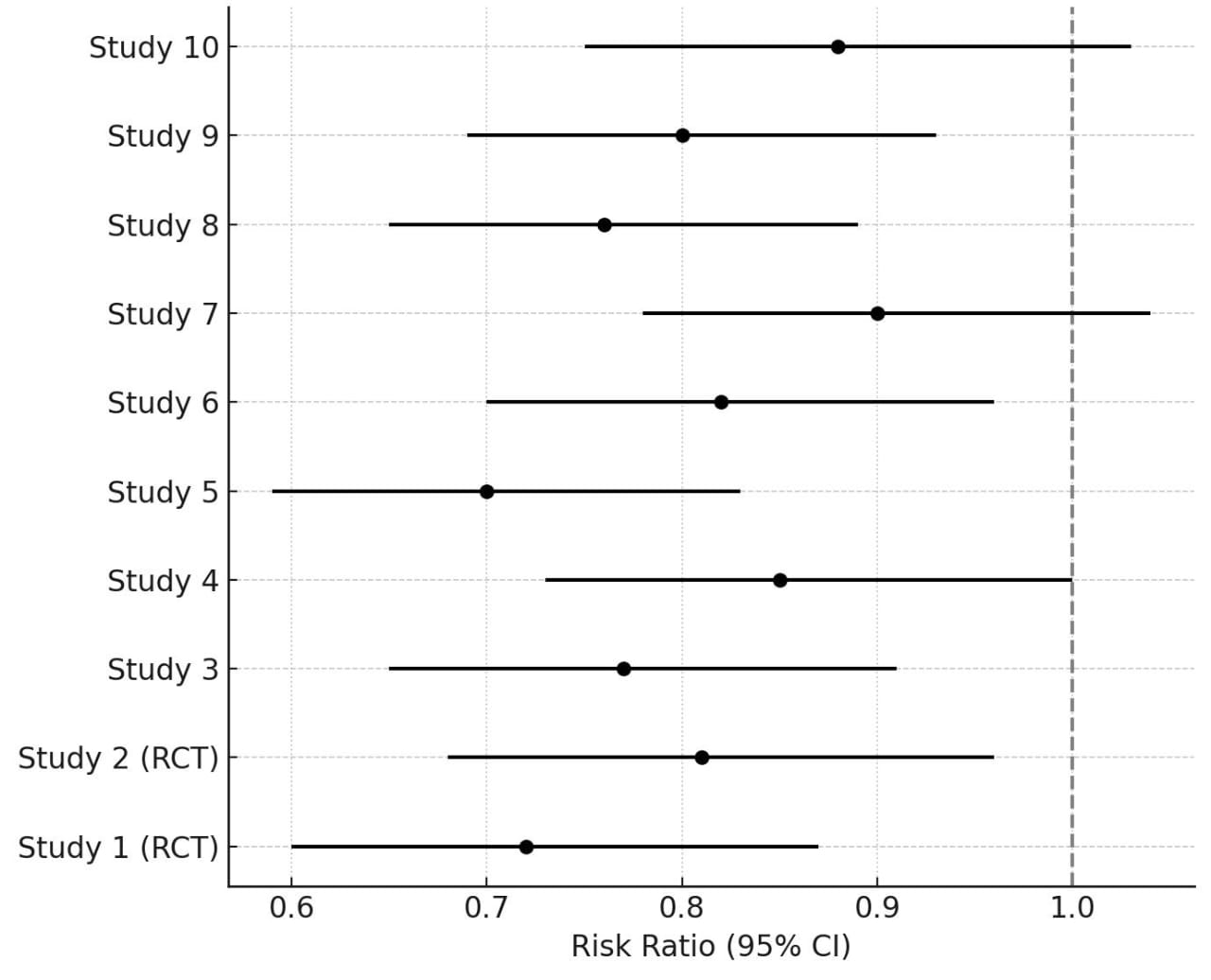
Figure: Figure 1: Forest Plot of Risk of MACE with NSBB use.
Disclosures:
Eunice Omeludike indicated no relevant financial relationships.
Babajide Obidigbo indicated no relevant financial relationships.
Abdul-Rahaman Ottun indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Cherechi Nwabueze indicated no relevant financial relationships.
Ooreoluwa Fasola indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Samuel Acheampong indicated no relevant financial relationships.
Elizabeth Soladoye indicated no relevant financial relationships.
Chisom Nwaneki indicated no relevant financial relationships.
Papa Beeko indicated no relevant financial relationships.
Brice Njobe indicated no relevant financial relationships.
Eunice Omeludike, MD1, Babajide Obidigbo, MBBS2, Abdul-Rahaman A. Ottun, MD3, Eunice Aregbesola, MD4, Cherechi Nwabueze, MBBS, MPH5, Ooreoluwa Fasola, MD6, Sarpong Boateng, MD, MPH7, Samuel Acheampong, MD, MSc3, Elizabeth Soladoye, MD, MPH3, Chisom Nwaneki, MD, MPH8, Papa K. Beeko, MBChB3, Brice Njobe, MD, MPH9. P1506 - Beyond Varices: The Cardiovascular Impact of Non-Selective Beta-Blockers in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Piedmont Athens Regional Medical Centre, Athens, GA; 2York and Scaborough NHS Foundation Trust, Scaborough, England, United Kingdom; 3Piedmont Athens Regional, Athens, GA; 4University of Missouri Health Care, Columbia, MO; 5John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 6Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX; 7Yale New Haven Health, Bridgeport, CT; 8Saint Peter's University Hospital, New Brunswick, NJ, New Brunswick, NJ; 9Piedmont Athens Regional Medical center, Athens, GA
Introduction: Patients with cirrhosis and portal hypertension are at elevated cardiovascular risk due to systemic inflammation, autonomic imbalance, and hemodynamic alterations. Non-selective beta-blockers (NSBBs), routinely used to prevent variceal bleeding, may also influence cardiovascular outcomes.
Methods: We conducted a systematic review and meta-analysis using the PRISMA guidelines. Literature
searches were performed across PubMed, Embase, and Cochrane Library through February 2025
for studies assessing cardiovascular outcomes in adults with cirrhosis and clinically significant
portal hypertension on long-term NSBB therapy (propranolol, nadolol, or carvedilol) versus no
NSBBs. The primary outcome was major adverse cardiovascular events (MACE: myocardial
infarction, stroke, cardiovascular death). Secondary outcomes included all-cause mortality and
heart failure hospitalization. Ten eligible studies (N = 18,612 patients), including two
randomized controlled trials and eight observational cohorts, were included. Data were pooled
using a random-effects model, and heterogeneity was quantified using the I² statistic. The risk of bias was assessed
using the Newcastle–Ottawa Scale for cohorts and the Cochrane Risk of Bias 2 tool for RCTs.
Results: Pooled analysis showed that NSBB use was associated with a statistically significant reduction in MACE (RR = 0.79, 95% CI: 0.68–0.91; p = 0.001; I² = 41%) and all-cause mortality (RR = 0.83,95% CI: 0.74–0.94; p = 0.004; I² = 52%). No significant difference was observed in heart failure hospitalizations (RR = 1.06, 95% CI: 0.89–1.26; p = 0.51; I² = 35%). Subgroup analyses by age, MELD score, and diabetes status confirmed the cardioprotective trend. Sensitivity analyses and leave-one-out tests confirmed robustness. Funnel plot and Egger's test showed minimal publication bias. Figure 1 presents the forest plot summarizing the relative risks of major adverse cardiovascular events (MACE) across the included studies.
Discussion: Our meta-analysis provides pooled evidence supporting the cardiovascular benefit of NSBBs in patients with cirrhosis and portal hypertension. NSBBs are associated with a lower risk of MACE and mortality without increasing heart failure admissions. These findings suggest that NSBBs may serve a dual protective role—reducing both portal pressures and cardiovascular burden. While RCTs strengthen the conclusions, larger prospective trials remain necessary to confirm causality and guide practice.
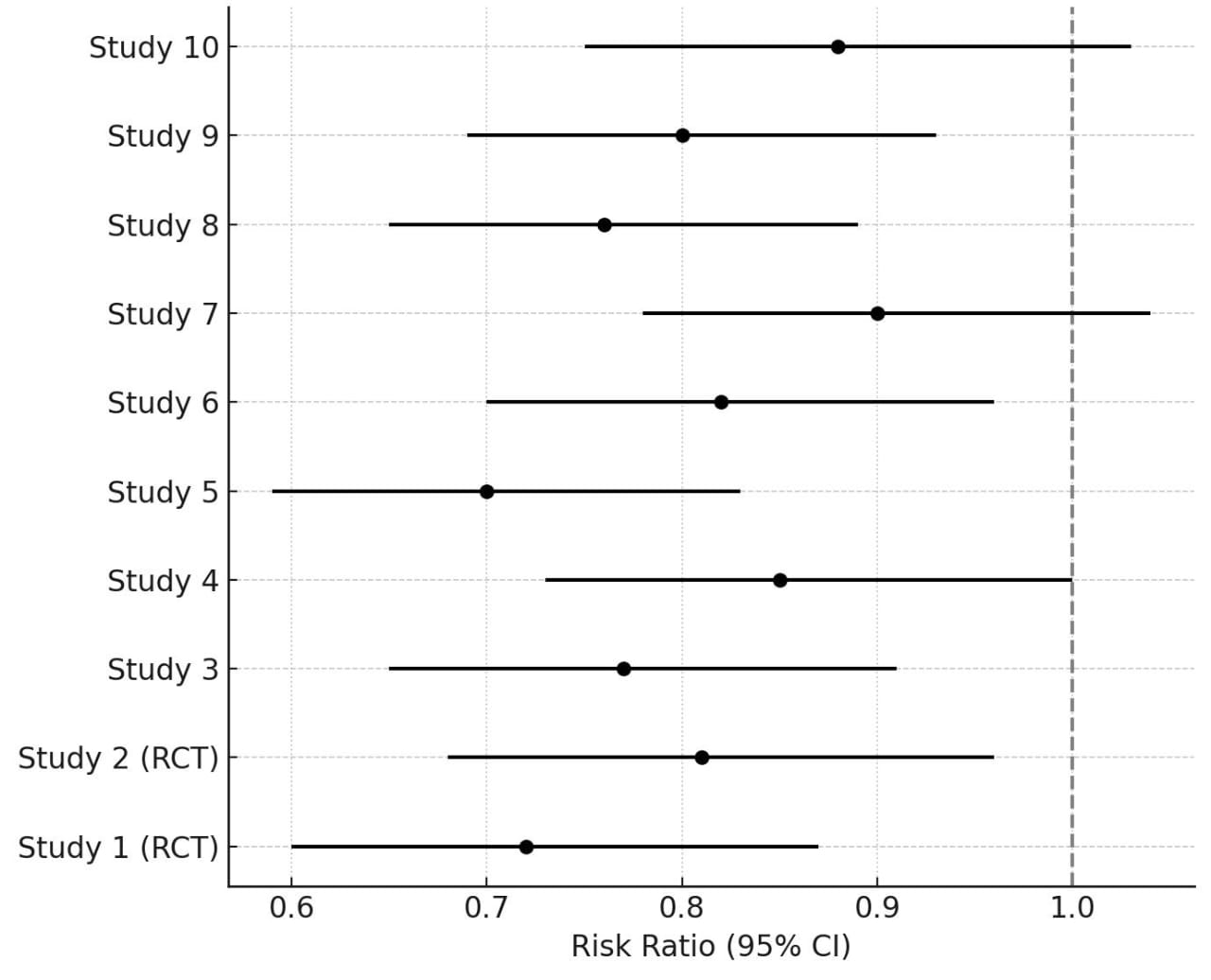
Figure: Figure 1: Forest Plot of Risk of MACE with NSBB use.
Disclosures:
Eunice Omeludike indicated no relevant financial relationships.
Babajide Obidigbo indicated no relevant financial relationships.
Abdul-Rahaman Ottun indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Cherechi Nwabueze indicated no relevant financial relationships.
Ooreoluwa Fasola indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Samuel Acheampong indicated no relevant financial relationships.
Elizabeth Soladoye indicated no relevant financial relationships.
Chisom Nwaneki indicated no relevant financial relationships.
Papa Beeko indicated no relevant financial relationships.
Brice Njobe indicated no relevant financial relationships.
Eunice Omeludike, MD1, Babajide Obidigbo, MBBS2, Abdul-Rahaman A. Ottun, MD3, Eunice Aregbesola, MD4, Cherechi Nwabueze, MBBS, MPH5, Ooreoluwa Fasola, MD6, Sarpong Boateng, MD, MPH7, Samuel Acheampong, MD, MSc3, Elizabeth Soladoye, MD, MPH3, Chisom Nwaneki, MD, MPH8, Papa K. Beeko, MBChB3, Brice Njobe, MD, MPH9. P1506 - Beyond Varices: The Cardiovascular Impact of Non-Selective Beta-Blockers in Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
