Sunday Poster Session
Category: Liver
P1497 - Clinical Parameters Associated With Steatosis and Inflammation on Explant in Patients Undergoing Liver Transplantation for Alcohol-Associated Hepatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Qusai Al Zureikat, MD (he/him/his)
MedStar Health-Georgetown/Washington Hospital Center
Washington, DC
Presenting Author(s)
Qusai Al Zureikat, MD1, Sarah Wang Bu, BS2, Ahmad Abdulraheem, MD3, Brototo Deb, MD4, Amol Rangnekar, MD5, Hanna Blaney, MD, MPH5
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2Georgetown University School of Medicine, Washington, DC; 3MedStar Washington Hospital Center-Georgetown University, Washington, DC; 4MedStar Health, Washington, DC; 5MedStar Georgetown University Hospital, Washington, DC
Introduction: Alcohol-associated hepatitis (AH) represents a severe form of alcohol-associated liver disease. Histological findings such as steatosis and inflammation are histologic hallmarks of AH. Understanding the clinical correlates of these features may enhance risk stratification and management of AH
Methods: We conducted a retrospective analysis of patients who underwent liver transplantation (LT) for AH at a single center. Explant liver histology was reviewed, and patients were categorized into four groups based on the presence or absence of steatosis and inflammation: (1) neither steatosis nor inflammation, (2) inflammation only, (3) steatosis only, and (4) both steatosis and inflammation. Pre-transplant demographic, clinical, laboratory, and imaging data were compared across groups using Kruskal-Wallis and Fisher’s exact tests, with a significance threshold of p < 0.05
Results: Among 71 patients who underwent LT for AH, 6 (8.5%) had neither steatosis nor inflammation, 9 (12.7%) had inflammation only, 8 (11.3%) had steatosis only, and 48 (67.6%) had both steatosis and inflammation on explant histology. Notably, neutrophil percentage differed significantly among groups (p = 0.009), with the lowest mean observed in patients lacking both histological features. AST levels were significantly higher in patients with steatosis only and those with both steatosis and inflammation compared to patients with inflammation only (p=0.049 for both), highlighting an association between steatosis and hepatocellular injury in AH. Additionally, time from last drink to transplant differed significantly between patients with both steatosis and inflammation and those with inflammation only (p = 0.029), indicating that the duration of abstinence prior to transplantation may be linked to the degree of hepatic steatosis present at the time of transplant. MELD 3.0 was not statistically significant between the groups (p=0.891)
Discussion: Histological evidence of steatosis and/or inflammation are hallmarks of AH and, in explanted livers of patients undergoing LT for AH, is associated with distinct clinical and laboratory profiles. Certain clinical parameters, including neutrophil count, AST levels may reflect underlying histopathological changes which may offer insights into patients undergoing evaluation for early LT for AH. Further research is warranted to better understand the prognostic implications of these associations and to guide management of AH
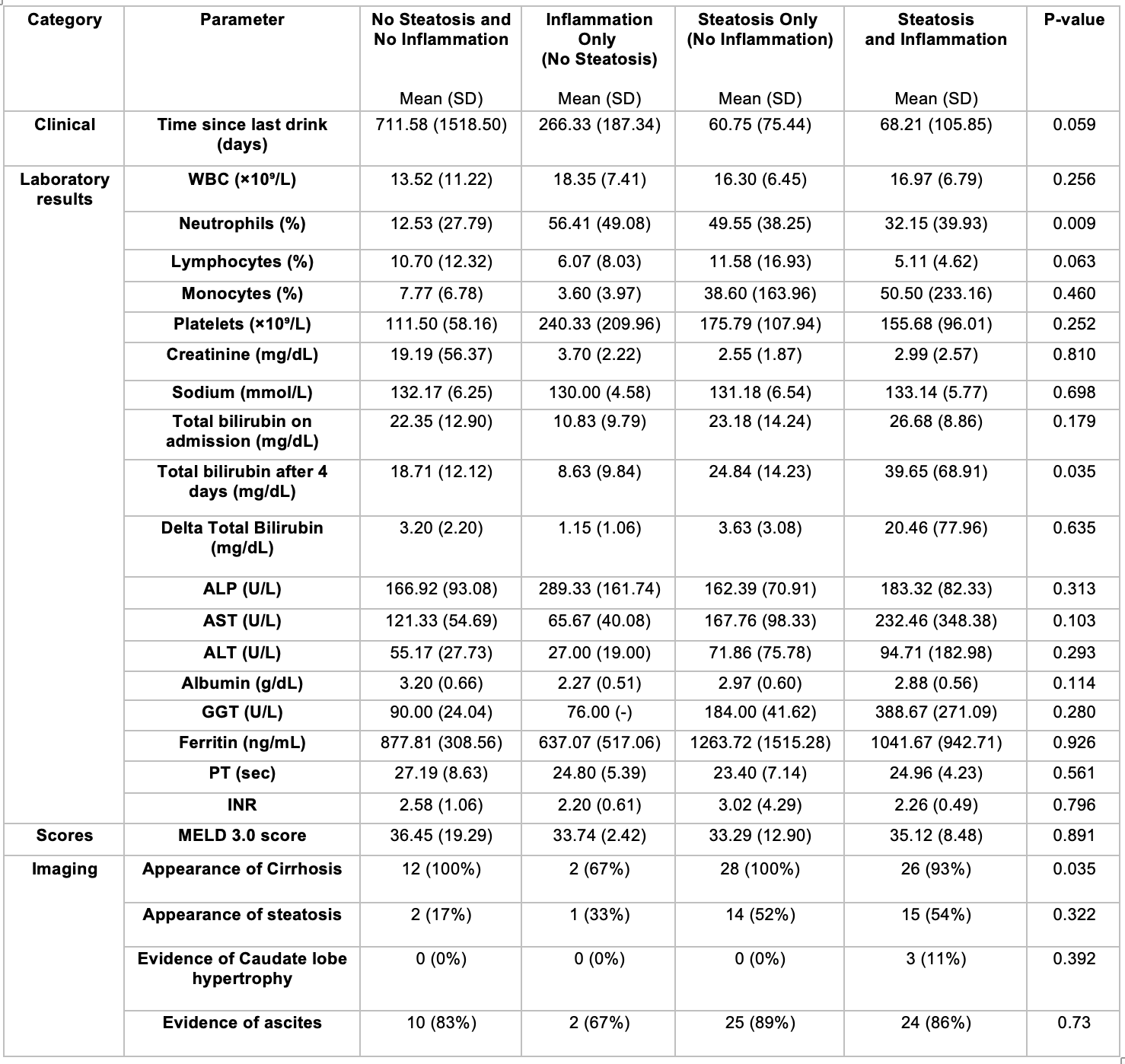
Figure: Table 1. Clinical, Laboratory and Radiographic Characteristics by Steatosis and Inflammation Status
Disclosures:
Qusai Al Zureikat indicated no relevant financial relationships.
Sarah Wang Bu indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Brototo Deb indicated no relevant financial relationships.
Amol Rangnekar indicated no relevant financial relationships.
Hanna Blaney indicated no relevant financial relationships.
Qusai Al Zureikat, MD1, Sarah Wang Bu, BS2, Ahmad Abdulraheem, MD3, Brototo Deb, MD4, Amol Rangnekar, MD5, Hanna Blaney, MD, MPH5. P1497 - Clinical Parameters Associated With Steatosis and Inflammation on Explant in Patients Undergoing Liver Transplantation for Alcohol-Associated Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2Georgetown University School of Medicine, Washington, DC; 3MedStar Washington Hospital Center-Georgetown University, Washington, DC; 4MedStar Health, Washington, DC; 5MedStar Georgetown University Hospital, Washington, DC
Introduction: Alcohol-associated hepatitis (AH) represents a severe form of alcohol-associated liver disease. Histological findings such as steatosis and inflammation are histologic hallmarks of AH. Understanding the clinical correlates of these features may enhance risk stratification and management of AH
Methods: We conducted a retrospective analysis of patients who underwent liver transplantation (LT) for AH at a single center. Explant liver histology was reviewed, and patients were categorized into four groups based on the presence or absence of steatosis and inflammation: (1) neither steatosis nor inflammation, (2) inflammation only, (3) steatosis only, and (4) both steatosis and inflammation. Pre-transplant demographic, clinical, laboratory, and imaging data were compared across groups using Kruskal-Wallis and Fisher’s exact tests, with a significance threshold of p < 0.05
Results: Among 71 patients who underwent LT for AH, 6 (8.5%) had neither steatosis nor inflammation, 9 (12.7%) had inflammation only, 8 (11.3%) had steatosis only, and 48 (67.6%) had both steatosis and inflammation on explant histology. Notably, neutrophil percentage differed significantly among groups (p = 0.009), with the lowest mean observed in patients lacking both histological features. AST levels were significantly higher in patients with steatosis only and those with both steatosis and inflammation compared to patients with inflammation only (p=0.049 for both), highlighting an association between steatosis and hepatocellular injury in AH. Additionally, time from last drink to transplant differed significantly between patients with both steatosis and inflammation and those with inflammation only (p = 0.029), indicating that the duration of abstinence prior to transplantation may be linked to the degree of hepatic steatosis present at the time of transplant. MELD 3.0 was not statistically significant between the groups (p=0.891)
Discussion: Histological evidence of steatosis and/or inflammation are hallmarks of AH and, in explanted livers of patients undergoing LT for AH, is associated with distinct clinical and laboratory profiles. Certain clinical parameters, including neutrophil count, AST levels may reflect underlying histopathological changes which may offer insights into patients undergoing evaluation for early LT for AH. Further research is warranted to better understand the prognostic implications of these associations and to guide management of AH
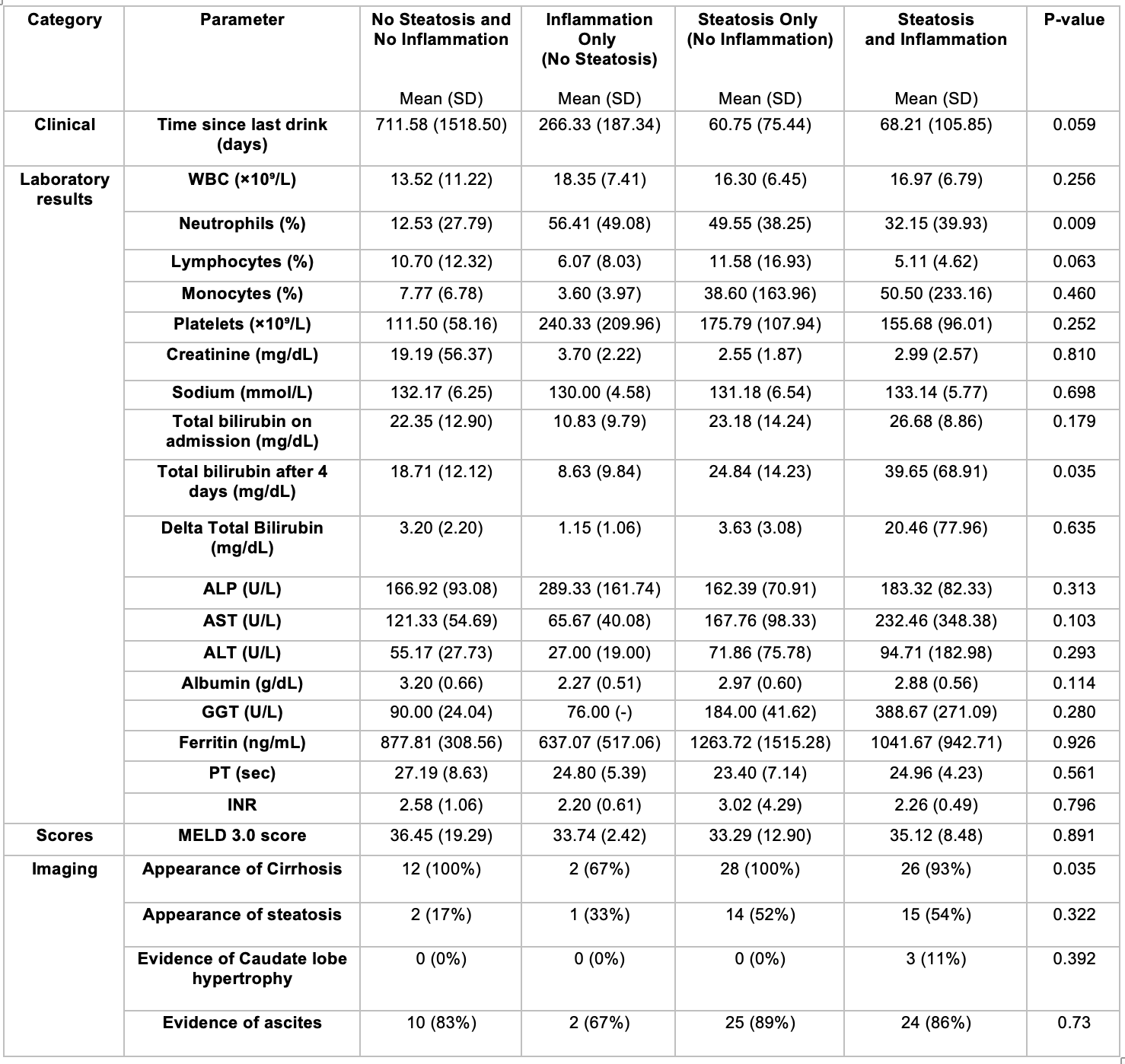
Figure: Table 1. Clinical, Laboratory and Radiographic Characteristics by Steatosis and Inflammation Status
Disclosures:
Qusai Al Zureikat indicated no relevant financial relationships.
Sarah Wang Bu indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Brototo Deb indicated no relevant financial relationships.
Amol Rangnekar indicated no relevant financial relationships.
Hanna Blaney indicated no relevant financial relationships.
Qusai Al Zureikat, MD1, Sarah Wang Bu, BS2, Ahmad Abdulraheem, MD3, Brototo Deb, MD4, Amol Rangnekar, MD5, Hanna Blaney, MD, MPH5. P1497 - Clinical Parameters Associated With Steatosis and Inflammation on Explant in Patients Undergoing Liver Transplantation for Alcohol-Associated Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
