Sunday Poster Session
Category: Liver
Impact of <i>Helicobacter pylori</i> on Liver Outcomes in Cirrhotic Patients
P1491 - Impact of Helicobacter pylori on Liver Outcomes in Cirrhotic Patients
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohammed Al-Aquily, MD
Norwalk Hospital/Yale University
Norwalk, CT
Presenting Author(s)
Mohammed Al-Aquily, MD1, Abdellatif Ismail, MD2, Ahmad Abdulraheem, MD3, Mohammad Kloub, MD4, Omar Abureesh, MD5
1Norwalk Hospital/Yale University, Norwalk, CT; 2University of Maryland, Baltimore, MD; 3MedStar Washington Hospital Center-Georgetown University, Washington, DC; 4New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 5Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Liver cirrhosis is a chronic liver disease that carries a guarded prognosis for affected patients. Helicobacter pylori (H. pylori) infection, while primarily known for causing gastrointestinal disease, has been increasingly reported to affect outcomes in patients with chronic liver disease. This study aims to evaluate whether H. pylori infection worsens clinical outcomes in patients with cirrhosis.
Methods: We conducted a retrospective cohort study using the TriNetX US Collaborative Network, utilizing data from 69 healthcare organizations. Two cohorts were identified: Cohort 1 included patients with cirrhosis and H. pylori infection (n = 13,282); Cohort 2 included patients with cirrhosis but without H. pylori infection (n = 753,113). Propensity score matching (PSM) was performed between the two cohorts based on demographics, comorbidities, elastography, and fibrosis score, resulting in 13,142 matched individuals in each cohort. Outcomes assessed included the development of hepatocellular carcinoma (HCC), ascites, spontaneous bacterial peritonitis (SBP), esophageal varices, hepatorenal syndrome (HRS), hepatic encephalopathy (HE), mortality, and combined liver-related events. Comparative analyses used risk ratios and Kaplan-Meier survival estimates over a 10-year follow-up period, excluding patients with pre-existing outcomes.
Results: As shown in Table 1, patients with H. pylori had significantly higher risks of HCC (RR 1.33; p< 0.001), ascites (RR 1.06; p=0.03), SBP (RR 1.18; p=0.008), and HRS (RR 1.29; p< 0.001). Interestingly, H. pylori-infected patients had lower all-cause mortality (RR 0.88; p< 0.001). No significant differences were found for hepatic encephalopathy or combined liver-related events.
Discussion: In cirrhotic patients, H. pylori co-infection correlates with a higher incidence of hepatic decompensation and HCC, yet lower all-cause mortality. These findings suggest an association between H. pylori and liver disease progression, requiring further interventional studies to evaluate the strength of this relationship.
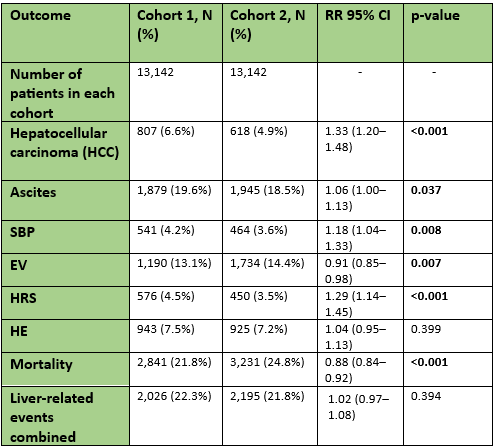
Figure: Table 1: Clinical outcomes in cirrhotic patients with and without H. pylori , cohort 1 and 2 respectively. Statistically significant results were bolded. Patients who had an outcome prior to the time window were excluded from the analysis.
Disclosures:
Mohammed Al-Aquily indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Omar Abureesh indicated no relevant financial relationships.
Mohammed Al-Aquily, MD1, Abdellatif Ismail, MD2, Ahmad Abdulraheem, MD3, Mohammad Kloub, MD4, Omar Abureesh, MD5. P1491 - Impact of <i>Helicobacter pylori</i> on Liver Outcomes in Cirrhotic Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Norwalk Hospital/Yale University, Norwalk, CT; 2University of Maryland, Baltimore, MD; 3MedStar Washington Hospital Center-Georgetown University, Washington, DC; 4New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 5Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Liver cirrhosis is a chronic liver disease that carries a guarded prognosis for affected patients. Helicobacter pylori (H. pylori) infection, while primarily known for causing gastrointestinal disease, has been increasingly reported to affect outcomes in patients with chronic liver disease. This study aims to evaluate whether H. pylori infection worsens clinical outcomes in patients with cirrhosis.
Methods: We conducted a retrospective cohort study using the TriNetX US Collaborative Network, utilizing data from 69 healthcare organizations. Two cohorts were identified: Cohort 1 included patients with cirrhosis and H. pylori infection (n = 13,282); Cohort 2 included patients with cirrhosis but without H. pylori infection (n = 753,113). Propensity score matching (PSM) was performed between the two cohorts based on demographics, comorbidities, elastography, and fibrosis score, resulting in 13,142 matched individuals in each cohort. Outcomes assessed included the development of hepatocellular carcinoma (HCC), ascites, spontaneous bacterial peritonitis (SBP), esophageal varices, hepatorenal syndrome (HRS), hepatic encephalopathy (HE), mortality, and combined liver-related events. Comparative analyses used risk ratios and Kaplan-Meier survival estimates over a 10-year follow-up period, excluding patients with pre-existing outcomes.
Results: As shown in Table 1, patients with H. pylori had significantly higher risks of HCC (RR 1.33; p< 0.001), ascites (RR 1.06; p=0.03), SBP (RR 1.18; p=0.008), and HRS (RR 1.29; p< 0.001). Interestingly, H. pylori-infected patients had lower all-cause mortality (RR 0.88; p< 0.001). No significant differences were found for hepatic encephalopathy or combined liver-related events.
Discussion: In cirrhotic patients, H. pylori co-infection correlates with a higher incidence of hepatic decompensation and HCC, yet lower all-cause mortality. These findings suggest an association between H. pylori and liver disease progression, requiring further interventional studies to evaluate the strength of this relationship.
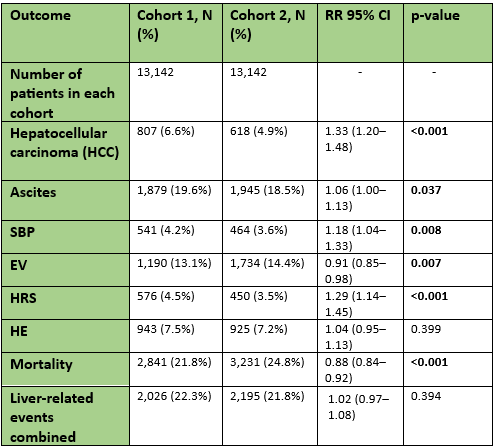
Figure: Table 1: Clinical outcomes in cirrhotic patients with and without H. pylori , cohort 1 and 2 respectively. Statistically significant results were bolded. Patients who had an outcome prior to the time window were excluded from the analysis.
Disclosures:
Mohammed Al-Aquily indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Omar Abureesh indicated no relevant financial relationships.
Mohammed Al-Aquily, MD1, Abdellatif Ismail, MD2, Ahmad Abdulraheem, MD3, Mohammad Kloub, MD4, Omar Abureesh, MD5. P1491 - Impact of <i>Helicobacter pylori</i> on Liver Outcomes in Cirrhotic Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
