Sunday Poster Session
Category: Interventional Endoscopy
P1472 - Successful Percutaneous Endoscopic Gastrostomy in a Pemphigus Vulgaris Patient With Severe Dysphagia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- TA
Taimur Aslam, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Taimur Aslam, MD1, Joelle Sleiman, MD1, Sabeen Jafri, MD2, Mohammad Abureesh, MD1, Ali Sohail, DO3, Sherif Andrawes, MD1, Jean Chalhoub, MD1, Youssef El Douaihy, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Touro College of Osteopathic Medicine, Staten Island, NY; 3Staten Island University Hospital, Northwell Health, Brooklyn, NY
Introduction: Pemphigus vulgaris (PV) is an autoimmune blistering disease that can cause painful mucocutaneous lesions leading to dysphagia, odynophagia and malnutrition in severe cases, necessitating nutritional support. Percutaneous Endoscopic Gastrostomy (PEG) tube placement, a common method for long-term enteral nutrition, can be challenging with severe gastrointestinal wall inflammation, as seen in PV. This report describes the successful PEG tube placement in a patient with active PV and significant aerodigestive involvement. This case is relevant as it highlights individualized decision-making and procedural expertise in managing nutritional challenges in PV patients.
Case Description/
Methods: 76-year-old male, recently diagnosed with PV presented with decreased oral intake for two weeks due to painful buccal lesions. Physical examination revealed ill-defined palatine erosions, oral mucosal ulcers, lip crusting, tongue and nose erosions, generalized erythema, and crusting on forearms and elbows. A modified barium swallow showed profound pharyngeal dysphagia with aspiration. Nasogastric tube (NG) was contraindicated due to severe ulcerations and crusts noted on nose. An initial EGD for PEG placement revealed friable esophageal mucosa, ulcerations, and spontaneous bleeding, leading to procedure abortion. Partial Parenteral Nutrition (PPN) was initiated on day 10 of the hospital stay. A second PEG tube attempt on day 16, under general anesthesia, showed improved, though still friable, esophageal mucosa. A 20 Fr PEG tube was successfully placed, and its position confirmed endoscopically (fig A & B). The patient tolerated the procedure well without complications.
Discussion: This case demonstrates the successful PEG tube placement in a patient with severe oral and esophageal PV, a scenario with limited literature guidance. The decision to proceed with PEG placement, despite initial abortive attempt due to severe mucosal friability and bleeding risk, was weighed against the necessity for enteral nutritional support, as Total Parental Nutrition (TPN) has less favorable outcomes. The successful outcome underscores the importance of individualized assessment, re-evaluation of mucosal condition, and skilled execution in complex PV cases. This experience suggests PEG tubes can be safely placed in active PV with upper GI involvement with appropriate expertise and a multidisciplinary approach, warranting further research into optimal management for such complicated presentations.
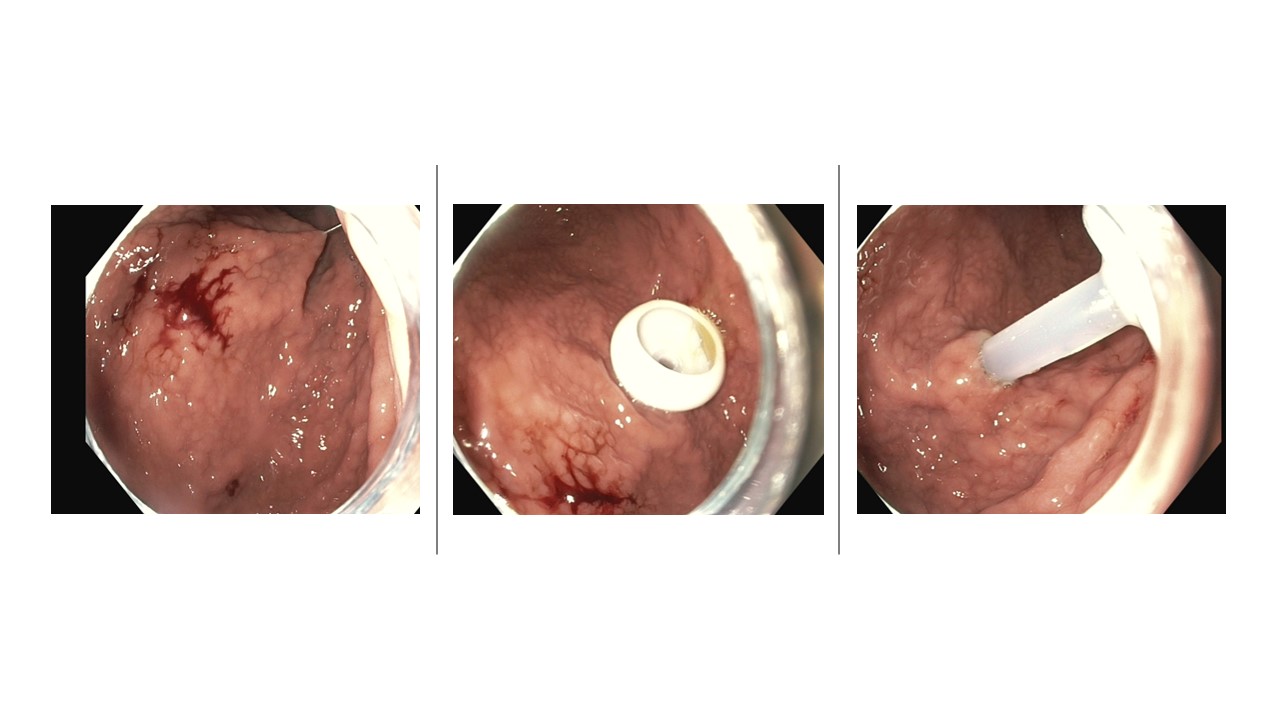
Figure: Fig A
Esophagogastroduodenoscopy showing diffusely inflamed and friable esophageal mucosa, indicative of mucosal involvement secondary to pemphigus vulgaris
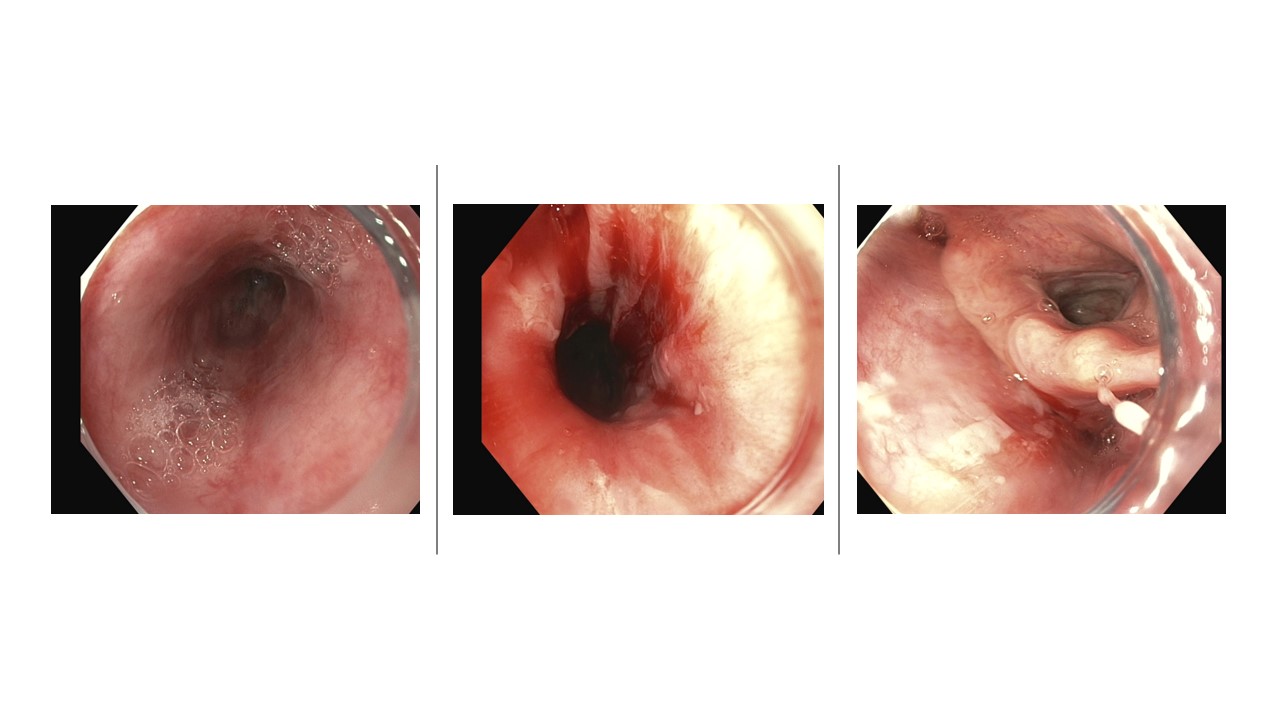
Figure: Fig B
Endoscopic confirmation of successful percutaneous endoscopic gastrostomy (PEG) tube placement.
Disclosures:
Taimur Aslam indicated no relevant financial relationships.
Joelle Sleiman indicated no relevant financial relationships.
Sabeen Jafri indicated no relevant financial relationships.
Mohammad Abureesh indicated no relevant financial relationships.
Ali Sohail indicated no relevant financial relationships.
Sherif Andrawes indicated no relevant financial relationships.
Jean Chalhoub indicated no relevant financial relationships.
Youssef El Douaihy indicated no relevant financial relationships.
Taimur Aslam, MD1, Joelle Sleiman, MD1, Sabeen Jafri, MD2, Mohammad Abureesh, MD1, Ali Sohail, DO3, Sherif Andrawes, MD1, Jean Chalhoub, MD1, Youssef El Douaihy, MD1. P1472 - Successful Percutaneous Endoscopic Gastrostomy in a Pemphigus Vulgaris Patient With Severe Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Touro College of Osteopathic Medicine, Staten Island, NY; 3Staten Island University Hospital, Northwell Health, Brooklyn, NY
Introduction: Pemphigus vulgaris (PV) is an autoimmune blistering disease that can cause painful mucocutaneous lesions leading to dysphagia, odynophagia and malnutrition in severe cases, necessitating nutritional support. Percutaneous Endoscopic Gastrostomy (PEG) tube placement, a common method for long-term enteral nutrition, can be challenging with severe gastrointestinal wall inflammation, as seen in PV. This report describes the successful PEG tube placement in a patient with active PV and significant aerodigestive involvement. This case is relevant as it highlights individualized decision-making and procedural expertise in managing nutritional challenges in PV patients.
Case Description/
Methods: 76-year-old male, recently diagnosed with PV presented with decreased oral intake for two weeks due to painful buccal lesions. Physical examination revealed ill-defined palatine erosions, oral mucosal ulcers, lip crusting, tongue and nose erosions, generalized erythema, and crusting on forearms and elbows. A modified barium swallow showed profound pharyngeal dysphagia with aspiration. Nasogastric tube (NG) was contraindicated due to severe ulcerations and crusts noted on nose. An initial EGD for PEG placement revealed friable esophageal mucosa, ulcerations, and spontaneous bleeding, leading to procedure abortion. Partial Parenteral Nutrition (PPN) was initiated on day 10 of the hospital stay. A second PEG tube attempt on day 16, under general anesthesia, showed improved, though still friable, esophageal mucosa. A 20 Fr PEG tube was successfully placed, and its position confirmed endoscopically (fig A & B). The patient tolerated the procedure well without complications.
Discussion: This case demonstrates the successful PEG tube placement in a patient with severe oral and esophageal PV, a scenario with limited literature guidance. The decision to proceed with PEG placement, despite initial abortive attempt due to severe mucosal friability and bleeding risk, was weighed against the necessity for enteral nutritional support, as Total Parental Nutrition (TPN) has less favorable outcomes. The successful outcome underscores the importance of individualized assessment, re-evaluation of mucosal condition, and skilled execution in complex PV cases. This experience suggests PEG tubes can be safely placed in active PV with upper GI involvement with appropriate expertise and a multidisciplinary approach, warranting further research into optimal management for such complicated presentations.
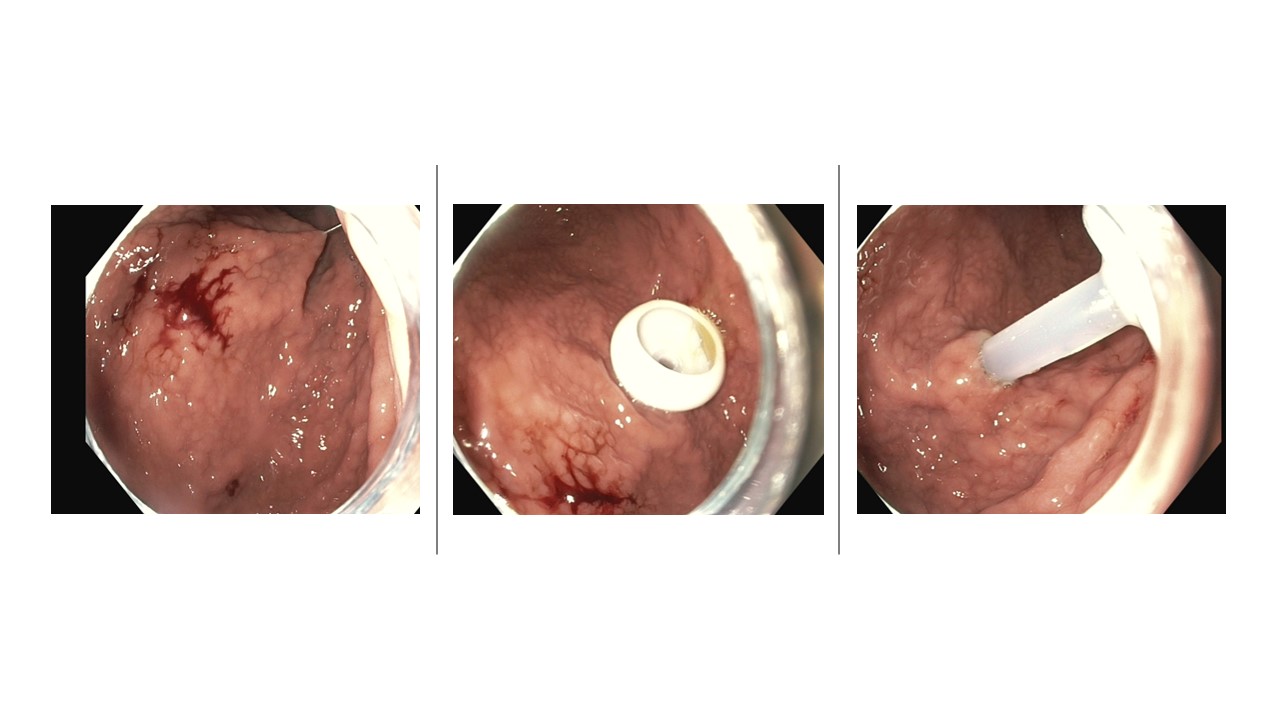
Figure: Fig A
Esophagogastroduodenoscopy showing diffusely inflamed and friable esophageal mucosa, indicative of mucosal involvement secondary to pemphigus vulgaris
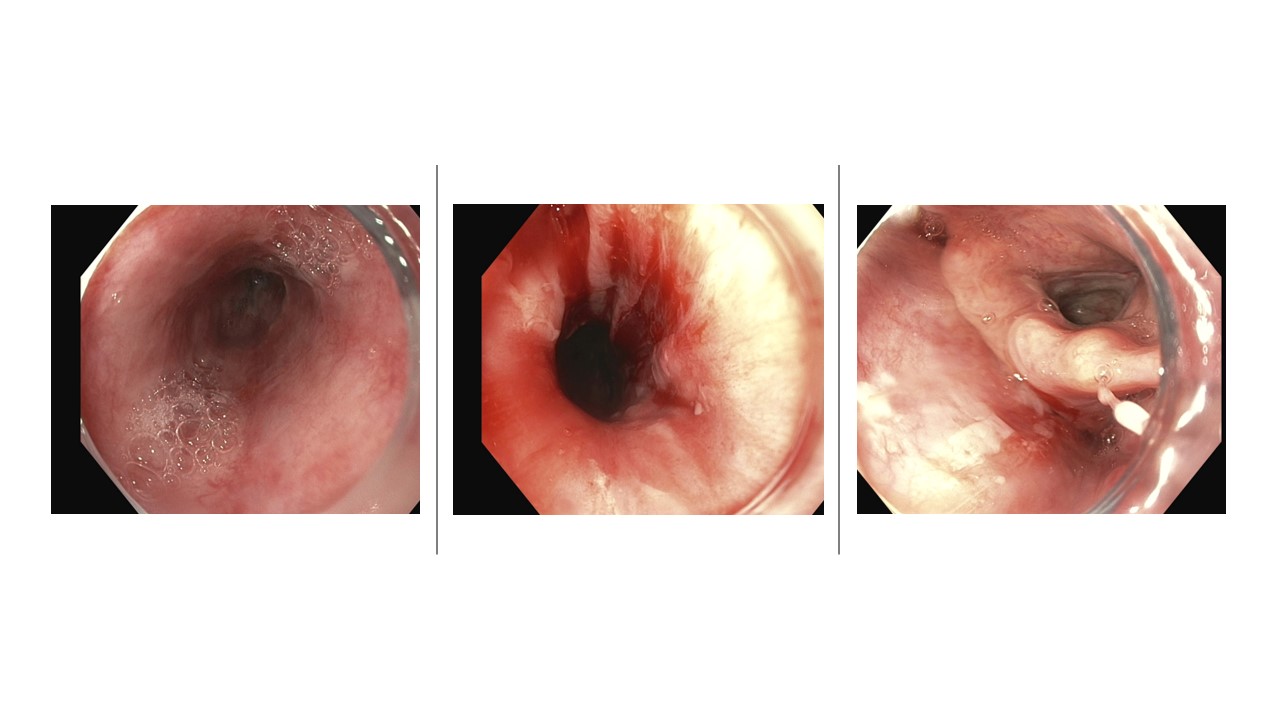
Figure: Fig B
Endoscopic confirmation of successful percutaneous endoscopic gastrostomy (PEG) tube placement.
Disclosures:
Taimur Aslam indicated no relevant financial relationships.
Joelle Sleiman indicated no relevant financial relationships.
Sabeen Jafri indicated no relevant financial relationships.
Mohammad Abureesh indicated no relevant financial relationships.
Ali Sohail indicated no relevant financial relationships.
Sherif Andrawes indicated no relevant financial relationships.
Jean Chalhoub indicated no relevant financial relationships.
Youssef El Douaihy indicated no relevant financial relationships.
Taimur Aslam, MD1, Joelle Sleiman, MD1, Sabeen Jafri, MD2, Mohammad Abureesh, MD1, Ali Sohail, DO3, Sherif Andrawes, MD1, Jean Chalhoub, MD1, Youssef El Douaihy, MD1. P1472 - Successful Percutaneous Endoscopic Gastrostomy in a Pemphigus Vulgaris Patient With Severe Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
