Sunday Poster Session
Category: Interventional Endoscopy
P1451 - Stuck in Transit: A Conservative Approach to a Migrated Biliary Stent
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Xavier Pollard
Uniformed Services University of the Health Sciences
Rockville, MD
Presenting Author(s)
Xavier Pollard, 1, Kathryn Driggers, MD2, Seth Dukes, MD2
1Uniformed Services University of the Health Sciences, Rockville, MD; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Fully covered biliary stents have a known high migration rate (up to 40%). However, they very rarely cause small bowel obstruction (SBO) after migration, with this complication being catalogued exclusively in case reports. Management of endoscopically unretrievable stents requires a careful approach, balancing the risks of surgical removal versus conservative management.
Case Description/
Methods: A 53-year-old man with metastatic pancreatic neuroendocrine tumor status post palliative radiation presented for one month of colicky abdominal pain. A choledochoduodenostomy had been previously created with a fully covered self-expanding metal stent for malignant biliary obstruction not amenable to transpapillary drainage. Endoscopic ultrasound for possible stent exchange and celiac plexus block was planned. During the procedure, the previously placed stent was found to have migrated into the mid-small bowel. He was admitted for monitoring but was clinically not obstructed and the stent location was unfavorable for endoscopic removal, so was discharged with close follow up. However, he re-presented for recurrent severe abdominal pain and repeat imaging revealed an SBO proximal to an intraluminal biliary stent surrounded by fecalization. He was admitted to the surgical service with overnight discussion about the safety of conservative management versus need for urgent surgery. Shortly after admission he had a bowel movement and abdominal pain improved, decreasing the urgency of definitive management. Both retrograde single-balloon and antegrade double-balloon enteroscopy failed to visualize the stent. The patient was now asymptomatic, so was discharged with planned possible repeat colonoscopy depending on ultimate stent location. 35 days after radiographic evidence of stent migration, serial X-rays confirmed its passage through the GI tract.
Discussion: Obstruction secondary to migrated biliary stents is rare, however, complications of this include hemorrhage and perforation. Thus, symptomatic presentations are typically treated urgently with endoscopic or surgical management. However, surgical management in these cases is often complicated, carrying high operative risks due to radiation associated changes and metastatic malignancy itself. While data are limited, watchful waiting may be appropriate for evolving SBOs. This approach can prevent surgical complications, which for this patient, would have meant delays in therapy for his metastatic cancer.
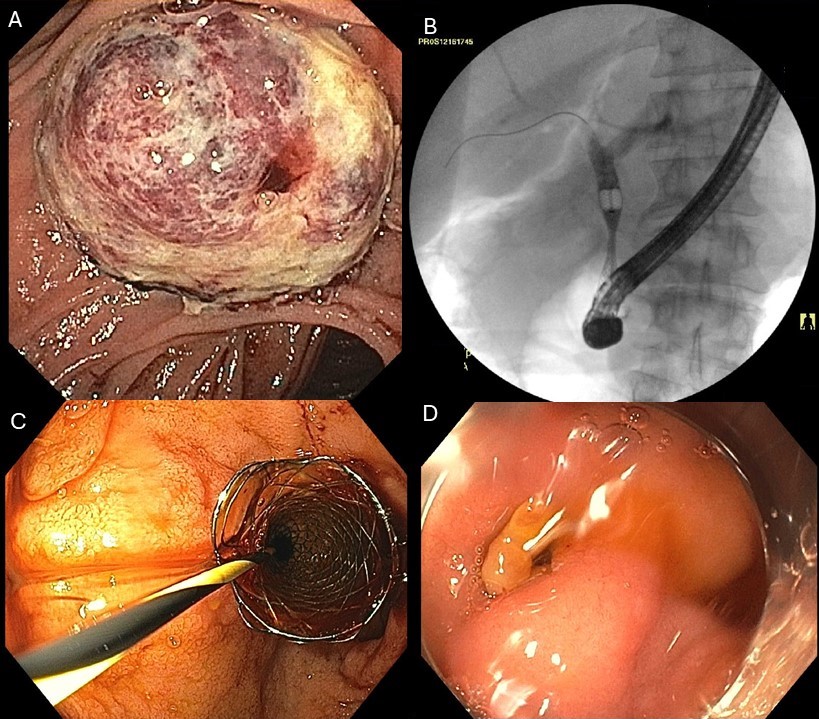
Figure: A. Sagittal view of stent obstruction and colonic dilation
B. Coronal View of stent obstruction and colonic dilation
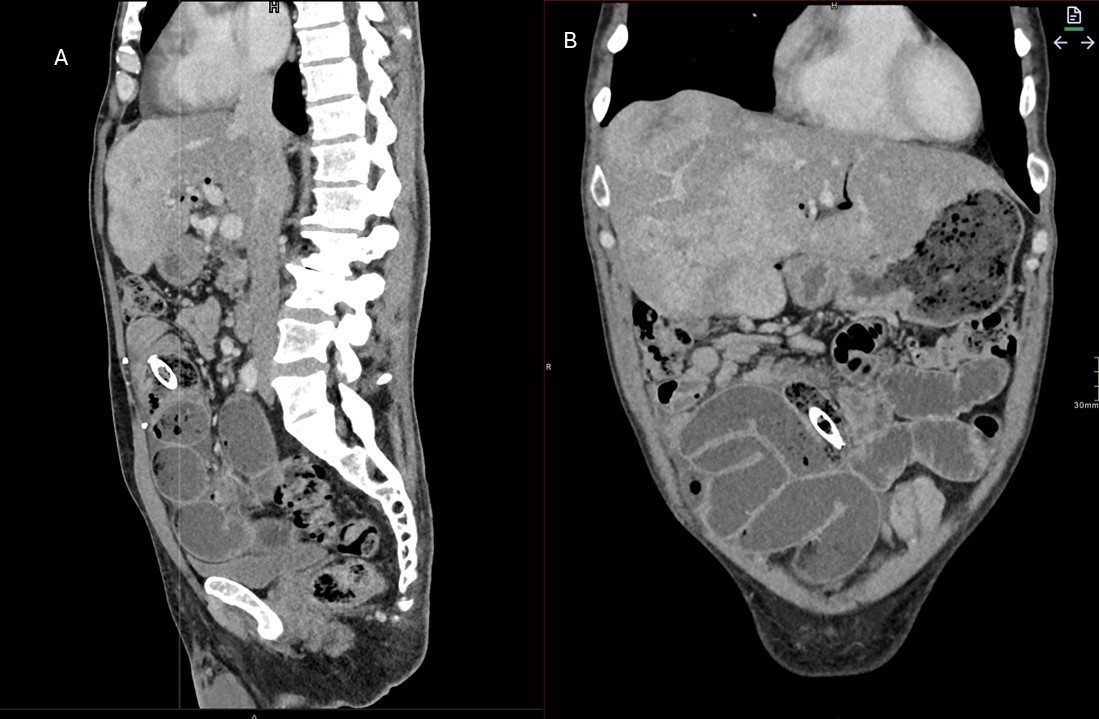
Figure: A. Ampullary mass
B. Stent placement under fluoroscopy
C. Stent endoscopic view
D. Choledochoduodenostomy fistula
Disclosures:
Xavier Pollard indicated no relevant financial relationships.
Kathryn Driggers indicated no relevant financial relationships.
Seth Dukes indicated no relevant financial relationships.
Xavier Pollard, 1, Kathryn Driggers, MD2, Seth Dukes, MD2. P1451 - Stuck in Transit: A Conservative Approach to a Migrated Biliary Stent, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Uniformed Services University of the Health Sciences, Rockville, MD; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Fully covered biliary stents have a known high migration rate (up to 40%). However, they very rarely cause small bowel obstruction (SBO) after migration, with this complication being catalogued exclusively in case reports. Management of endoscopically unretrievable stents requires a careful approach, balancing the risks of surgical removal versus conservative management.
Case Description/
Methods: A 53-year-old man with metastatic pancreatic neuroendocrine tumor status post palliative radiation presented for one month of colicky abdominal pain. A choledochoduodenostomy had been previously created with a fully covered self-expanding metal stent for malignant biliary obstruction not amenable to transpapillary drainage. Endoscopic ultrasound for possible stent exchange and celiac plexus block was planned. During the procedure, the previously placed stent was found to have migrated into the mid-small bowel. He was admitted for monitoring but was clinically not obstructed and the stent location was unfavorable for endoscopic removal, so was discharged with close follow up. However, he re-presented for recurrent severe abdominal pain and repeat imaging revealed an SBO proximal to an intraluminal biliary stent surrounded by fecalization. He was admitted to the surgical service with overnight discussion about the safety of conservative management versus need for urgent surgery. Shortly after admission he had a bowel movement and abdominal pain improved, decreasing the urgency of definitive management. Both retrograde single-balloon and antegrade double-balloon enteroscopy failed to visualize the stent. The patient was now asymptomatic, so was discharged with planned possible repeat colonoscopy depending on ultimate stent location. 35 days after radiographic evidence of stent migration, serial X-rays confirmed its passage through the GI tract.
Discussion: Obstruction secondary to migrated biliary stents is rare, however, complications of this include hemorrhage and perforation. Thus, symptomatic presentations are typically treated urgently with endoscopic or surgical management. However, surgical management in these cases is often complicated, carrying high operative risks due to radiation associated changes and metastatic malignancy itself. While data are limited, watchful waiting may be appropriate for evolving SBOs. This approach can prevent surgical complications, which for this patient, would have meant delays in therapy for his metastatic cancer.
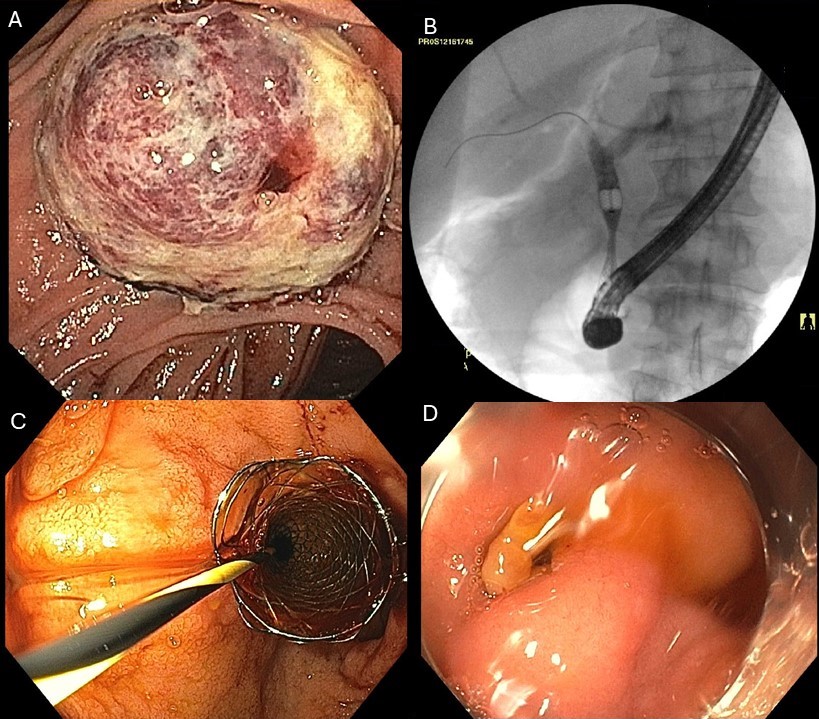
Figure: A. Sagittal view of stent obstruction and colonic dilation
B. Coronal View of stent obstruction and colonic dilation
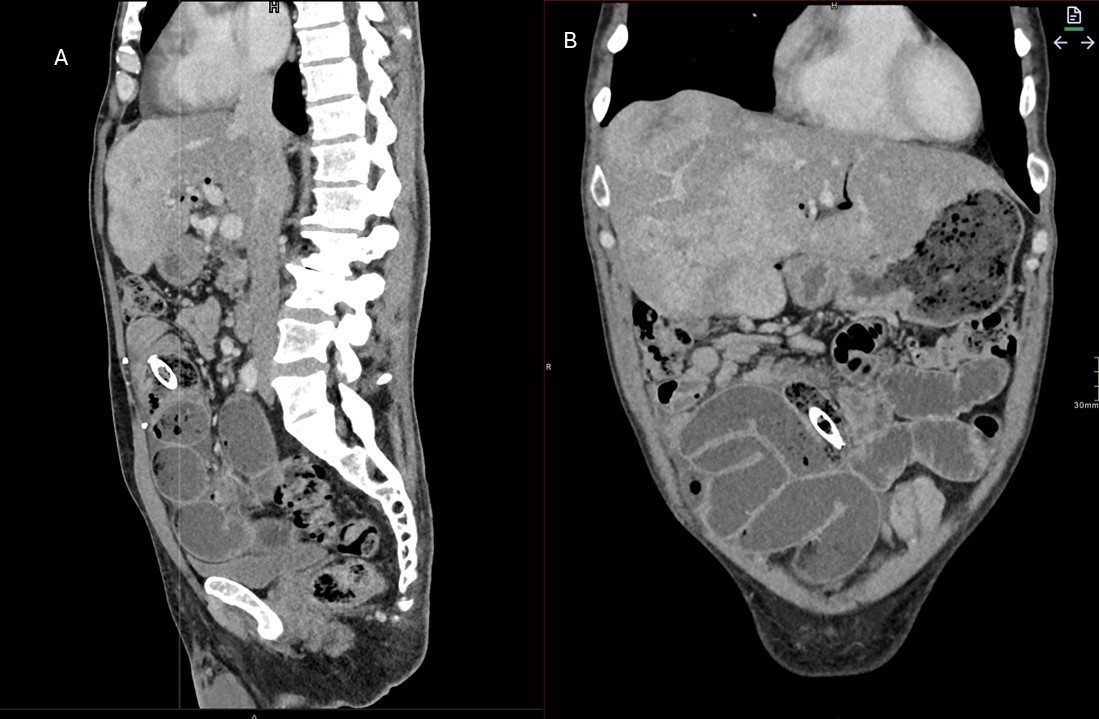
Figure: A. Ampullary mass
B. Stent placement under fluoroscopy
C. Stent endoscopic view
D. Choledochoduodenostomy fistula
Disclosures:
Xavier Pollard indicated no relevant financial relationships.
Kathryn Driggers indicated no relevant financial relationships.
Seth Dukes indicated no relevant financial relationships.
Xavier Pollard, 1, Kathryn Driggers, MD2, Seth Dukes, MD2. P1451 - Stuck in Transit: A Conservative Approach to a Migrated Biliary Stent, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
