Sunday Poster Session
Category: Interventional Endoscopy
P1449 - Small Bowel Obstruction From Ileocecal Anastomotic Stricture Treated With Lumen Apposing Metal Stent (LAMS)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SM
Safia Mohamed, MD (she/her/hers)
University of Massachusetts Chan Medical School - Baystate Health
Frederica, DE
Presenting Author(s)
Safia Mohamed, MD1, Aizaz Khan, MD1, Pranav Ramamurthy, MBBS, MD2, Nha Duong, DO3
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Granby, CT
Introduction: Fibrostenotic anastomotic strictures present a unique therapeutic challenge. Advancements in endoscopic therapy have provided options for management ranging from serial dilations to off label use of LAMS in short segment strictures. Most reported cases of LAMS are limited to the upper gastrointestinal tract. We herein report a case of small bowel obstruction (SBO) due to an ileocecal (IC) anastomotic stricture treated successfully with LAMS.
Case Description/
Methods: A 77-year-old woman with a remote history of ileocecectomy for perforated appendicitis presented with acute abdominal pain, distension, nausea, and vomiting after consuming a large quantity of pumpkin seeds. CT imaging revealed small bowel dilation with a transition point and stool ball at the ileocolic anastomosis with a collapsed colon (FIGURE 1A). The patient deferred surgical management and elected for a non-invasive approach therefore a therapeutic colonoscopy was offered. Due to her inability to tolerate a preparation, we proceeded with an unprepped colonoscopy using a therapeutic scope in anticipation of potential stent placement.
Multiple seeds and stool were seen at the area of the IC anastomosis and this was cleared with forceps. A small 8 mm stricture was seen at the opening which prohibited ileum intubation. In order to alleviate the obstruction and maintain patency without the need for serial dilations, we elected to place a 15 mm x 10 mm LAMS. A wire was advanced deep into the small bowel and the delivery catheter was advanced over wire followed by stent deployment under fluoroscopic guidance (FIGURE 1B). The stent was then dilated to 15 mm with immediate efflux of liquid stool from the ileum. The patient had immediate relief of symptoms with copious bowel movements. Post-procedural CT demonstrated free contrast flow into the colon along with appropriate positioning of the stent (FIGURE 1C). Follow-up colonoscopy at 4 weeks revealed a widely patent anastomosis and no further symptoms.
Discussion: This case highlights a novel, minimally invasive approach to managing benign ileocolonic strictures using LAMS in combination with guidewire-assisted balloon catheter techniques and fluoroscopy. Stepwise confirmation of the stricture and targeted dilation ensured precise stent placement and durable clinical response. This approach may be an effective alternative to surgery in select high-risk patients and warrants further investigation.
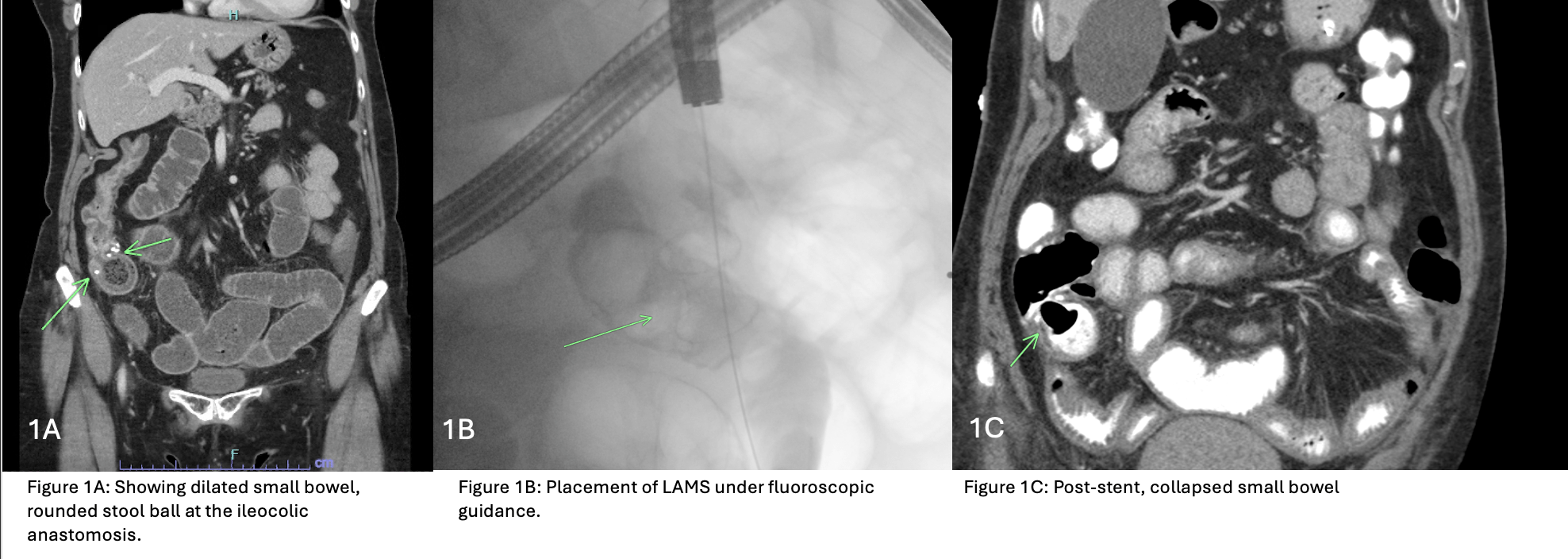
Figure: Figure 1A: Showing dilated small bowel, rounded stool ball at the ileocolic anastomosis. Figure 1B: Placement of LAMS under fluoroscopic guidance.
Figure 1C: Post-stent, collapsed small bowel.
Disclosures:
Safia Mohamed indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Pranav Ramamurthy indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Safia Mohamed, MD1, Aizaz Khan, MD1, Pranav Ramamurthy, MBBS, MD2, Nha Duong, DO3. P1449 - Small Bowel Obstruction From Ileocecal Anastomotic Stricture Treated With Lumen Apposing Metal Stent (LAMS), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 2University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Granby, CT
Introduction: Fibrostenotic anastomotic strictures present a unique therapeutic challenge. Advancements in endoscopic therapy have provided options for management ranging from serial dilations to off label use of LAMS in short segment strictures. Most reported cases of LAMS are limited to the upper gastrointestinal tract. We herein report a case of small bowel obstruction (SBO) due to an ileocecal (IC) anastomotic stricture treated successfully with LAMS.
Case Description/
Methods: A 77-year-old woman with a remote history of ileocecectomy for perforated appendicitis presented with acute abdominal pain, distension, nausea, and vomiting after consuming a large quantity of pumpkin seeds. CT imaging revealed small bowel dilation with a transition point and stool ball at the ileocolic anastomosis with a collapsed colon (FIGURE 1A). The patient deferred surgical management and elected for a non-invasive approach therefore a therapeutic colonoscopy was offered. Due to her inability to tolerate a preparation, we proceeded with an unprepped colonoscopy using a therapeutic scope in anticipation of potential stent placement.
Multiple seeds and stool were seen at the area of the IC anastomosis and this was cleared with forceps. A small 8 mm stricture was seen at the opening which prohibited ileum intubation. In order to alleviate the obstruction and maintain patency without the need for serial dilations, we elected to place a 15 mm x 10 mm LAMS. A wire was advanced deep into the small bowel and the delivery catheter was advanced over wire followed by stent deployment under fluoroscopic guidance (FIGURE 1B). The stent was then dilated to 15 mm with immediate efflux of liquid stool from the ileum. The patient had immediate relief of symptoms with copious bowel movements. Post-procedural CT demonstrated free contrast flow into the colon along with appropriate positioning of the stent (FIGURE 1C). Follow-up colonoscopy at 4 weeks revealed a widely patent anastomosis and no further symptoms.
Discussion: This case highlights a novel, minimally invasive approach to managing benign ileocolonic strictures using LAMS in combination with guidewire-assisted balloon catheter techniques and fluoroscopy. Stepwise confirmation of the stricture and targeted dilation ensured precise stent placement and durable clinical response. This approach may be an effective alternative to surgery in select high-risk patients and warrants further investigation.
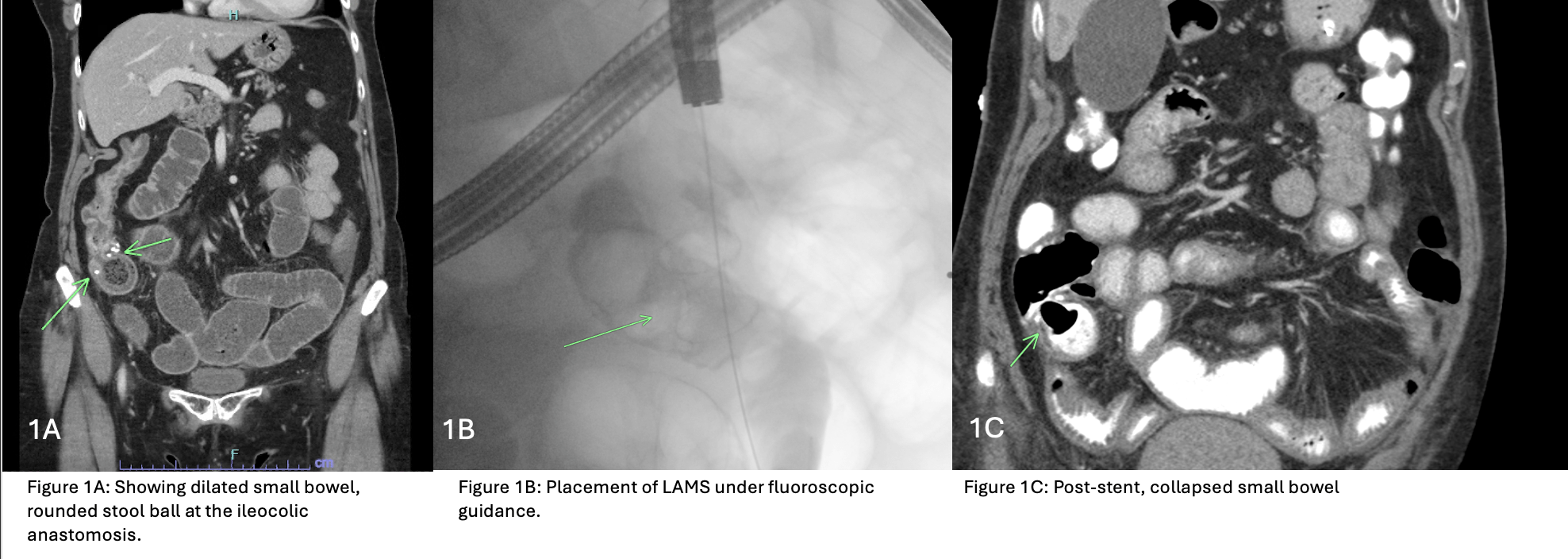
Figure: Figure 1A: Showing dilated small bowel, rounded stool ball at the ileocolic anastomosis. Figure 1B: Placement of LAMS under fluoroscopic guidance.
Figure 1C: Post-stent, collapsed small bowel.
Disclosures:
Safia Mohamed indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Pranav Ramamurthy indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Safia Mohamed, MD1, Aizaz Khan, MD1, Pranav Ramamurthy, MBBS, MD2, Nha Duong, DO3. P1449 - Small Bowel Obstruction From Ileocecal Anastomotic Stricture Treated With Lumen Apposing Metal Stent (LAMS), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
