Sunday Poster Session
Category: Interventional Endoscopy
P1448 - Endoscopic Management of a Duodenal Perforation From a Partially Migrated Biliary Stent Retained Within the Biliary Tree
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KD
Kartik Devgan, MD
Loyola University Medical Center
Chicago, IL
Presenting Author(s)
Kartik Devgan, MD1, Dinkar Ahuja, MD1, Mohammed Abourahma, MD2, Emma Schnittka, DO1, Michelle Lee, MD3, Rohit Agrawal, MD1
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Willowbrook, IL; 3Loyola University Medical Center, Maywood, IL
Introduction: ERCP with biliary stenting is the standard of care for managing biliary obstruction. Stent migration occurs in up to 10% of cases, with duodenal perforation in about 2.1%. Though rare, this complication carries significant risk, with mortality rates up to 17.4%. Traditionally managed with surgery, endoscopic options now offer less invasive alternatives with comparable outcomes. We present a case of endoscopic repair of a duodenal perforation from a partially migrated biliary stent retained within the biliary tree.
Case Description/
Methods: An 83-year-old woman with a malignant biliary stricture, previously treated with ERCP and stent exchanges, presented with fever and abdominal pain after recent stent replacement. EGD revealed both stents at the major papilla; the left-sided stent had partially migrated, perforating the opposite duodenal wall. The stent was removed by advancing it into the biliary system, then extracting the distal end with forceps, leaving a 3 mm perforation. A nearby ulcer precluded over-the-scope clip placement. Instead, the defect was closed with seven through-the-scope clips. A double pigtail stent was placed into the left hepatic duct to minimize the risk of further duodenal injury. A nasojejunal tube was placed for feeding, and the patient was continued on antibiotics. Follow-up imaging showed no contrast leak, indicating healed perforation.
Discussion: Bowel perforation due to biliary stent migration most commonly occurs in the duodenum. However, perforation of the duodenal wall directly opposite the ampulla is rarely described, and cases in which the stent remains within the biliary tree are even more uncommon. The left biliary system may predispose to this complication due to a steeper angle toward the opposing duodenal wall. Longer stents, like the 12 cm stent used in this case, may increase the risk by providing greater mechanical leverage during migration. Pigtail stents may reduce this risk by minimizing mucosal trauma. This case underscores the effectiveness of endoscopic therapy, with mortality rates comparable to those of surgery at 19.6% and 14.5%, respectively. Studies show endoscopic management enables faster resumption of oral intake and shorter hospital stays, with no compromise in closure strength. This case represents a rare occurrence of a biliary stent perforating the duodenum while remaining within the biliary tree, successfully managed with endoscopic repair, highlighting the role of endoscopy as an effective surgical alternative.
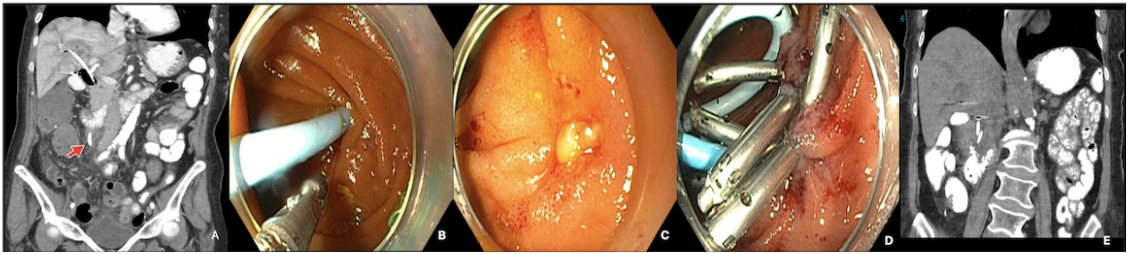
Figure: Figure 1: A: CT showing migrated stent causing duodenal perforation (arrow); B: Endoscopic image showing migrated stent causing duodenal perforation; C: Defect at site of perforation; D: Perforation closed by endoscopic clips; E: Healed perforation on CT with oral contrast
Disclosures:
Kartik Devgan indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Mohammed Abourahma indicated no relevant financial relationships.
Emma Schnittka indicated no relevant financial relationships.
Michelle Lee indicated no relevant financial relationships.
Rohit Agrawal indicated no relevant financial relationships.
Kartik Devgan, MD1, Dinkar Ahuja, MD1, Mohammed Abourahma, MD2, Emma Schnittka, DO1, Michelle Lee, MD3, Rohit Agrawal, MD1. P1448 - Endoscopic Management of a Duodenal Perforation From a Partially Migrated Biliary Stent Retained Within the Biliary Tree, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Chicago, IL; 2Loyola University Medical Center, Willowbrook, IL; 3Loyola University Medical Center, Maywood, IL
Introduction: ERCP with biliary stenting is the standard of care for managing biliary obstruction. Stent migration occurs in up to 10% of cases, with duodenal perforation in about 2.1%. Though rare, this complication carries significant risk, with mortality rates up to 17.4%. Traditionally managed with surgery, endoscopic options now offer less invasive alternatives with comparable outcomes. We present a case of endoscopic repair of a duodenal perforation from a partially migrated biliary stent retained within the biliary tree.
Case Description/
Methods: An 83-year-old woman with a malignant biliary stricture, previously treated with ERCP and stent exchanges, presented with fever and abdominal pain after recent stent replacement. EGD revealed both stents at the major papilla; the left-sided stent had partially migrated, perforating the opposite duodenal wall. The stent was removed by advancing it into the biliary system, then extracting the distal end with forceps, leaving a 3 mm perforation. A nearby ulcer precluded over-the-scope clip placement. Instead, the defect was closed with seven through-the-scope clips. A double pigtail stent was placed into the left hepatic duct to minimize the risk of further duodenal injury. A nasojejunal tube was placed for feeding, and the patient was continued on antibiotics. Follow-up imaging showed no contrast leak, indicating healed perforation.
Discussion: Bowel perforation due to biliary stent migration most commonly occurs in the duodenum. However, perforation of the duodenal wall directly opposite the ampulla is rarely described, and cases in which the stent remains within the biliary tree are even more uncommon. The left biliary system may predispose to this complication due to a steeper angle toward the opposing duodenal wall. Longer stents, like the 12 cm stent used in this case, may increase the risk by providing greater mechanical leverage during migration. Pigtail stents may reduce this risk by minimizing mucosal trauma. This case underscores the effectiveness of endoscopic therapy, with mortality rates comparable to those of surgery at 19.6% and 14.5%, respectively. Studies show endoscopic management enables faster resumption of oral intake and shorter hospital stays, with no compromise in closure strength. This case represents a rare occurrence of a biliary stent perforating the duodenum while remaining within the biliary tree, successfully managed with endoscopic repair, highlighting the role of endoscopy as an effective surgical alternative.
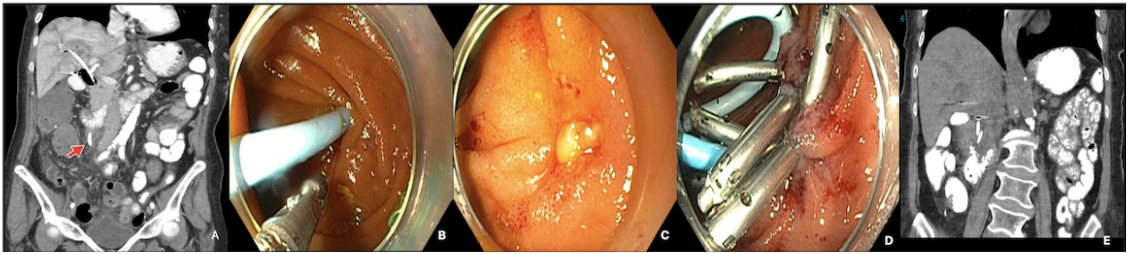
Figure: Figure 1: A: CT showing migrated stent causing duodenal perforation (arrow); B: Endoscopic image showing migrated stent causing duodenal perforation; C: Defect at site of perforation; D: Perforation closed by endoscopic clips; E: Healed perforation on CT with oral contrast
Disclosures:
Kartik Devgan indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Mohammed Abourahma indicated no relevant financial relationships.
Emma Schnittka indicated no relevant financial relationships.
Michelle Lee indicated no relevant financial relationships.
Rohit Agrawal indicated no relevant financial relationships.
Kartik Devgan, MD1, Dinkar Ahuja, MD1, Mohammed Abourahma, MD2, Emma Schnittka, DO1, Michelle Lee, MD3, Rohit Agrawal, MD1. P1448 - Endoscopic Management of a Duodenal Perforation From a Partially Migrated Biliary Stent Retained Within the Biliary Tree, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
