Sunday Poster Session
Category: Interventional Endoscopy
P1444 - A Stent on the Move: Endoscopic Repair of Duodenal Perforation Due to Biliary Stent Migration
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Alexander Satinsky, DO (he/him/his)
Riverside Medical Center
Kankakee, IL
Presenting Author(s)
Alexander Satinsky, DO1, Paul Kozak, DO1, Ashish Shah, MD2
1Riverside Medical Center, Kankakee, IL; 2Digestive Disease Consultants, Bourbonnais, IL
Introduction: Complications from ERCP can rarely include gastrointestinal perforation due to migrated biliary stent. Surgical repair is often used to repair duodenal perforations, however, minimally invasive endoscopic stent retrieval in the appropriate setting has become the preferred intervention. We present a case of a duodenal perforation resulting from a migrated biliary stent that was successfully repaired endoscopically.
Case Description/
Methods: A 66-year-old female with chronic conditions of COPD, CHF, and chronic Hepatitis C infection presented with right-sided abdominal pain radiating to her back. She was found to have an 8 mm calculus at the level of the pancreatic head with upstream intrahepatic and extrahepatic biliary ductal dilation. ERCP with sphincterotomy, balloon sweep, and 10 F x 7 cm plastic biliary stent placement was performed. She was deemed to be a poor surgical candidate for cholecystectomy given her comorbidities. Two weeks after discharge, the patient returned with severe left-sided flank pain. CT showed migration of the biliary stent with perforation of the duodenum. It was determined that the best course of action would be to remove the stent and clip the area of perforation endoscopically, with surgery available for emergent open laparotomy. On endoscopy, a migrated plastic biliary stent was observed puncturing through the anterior duodenal wall with mild ulceration in the second portion of the duodenum (figure 1). The intact stent was removed using rat toothed forceps. Afterward, a small 3 mm fistula was evident where the stent had punctured through the duodenal wall. One endoscopic clip was used with complete closure of the fistula (figure 2). The patient recovered remarkably well and was discharged one week after presentation.
Discussion: Stent migration typically results in benign passage through the GI tract; rarely, it can result in perforation. Intrinsic risks can include adhesions, hernias, and diverticula, and extrinsic can include material used. Management depends on several factors such as mechanism of perforation and clinical severity. While surgery is usually reserved for patients with peritonitis, endoscopy is a safe and effective therapy for migrated stent-associated perforation and is associated with faster recovery than a surgical approach. As the capabilities and expertise of endoscopy continue to evolve, management plans should be individualized and involve a minimally invasive approach when appropriate to maximize patient outcomes.
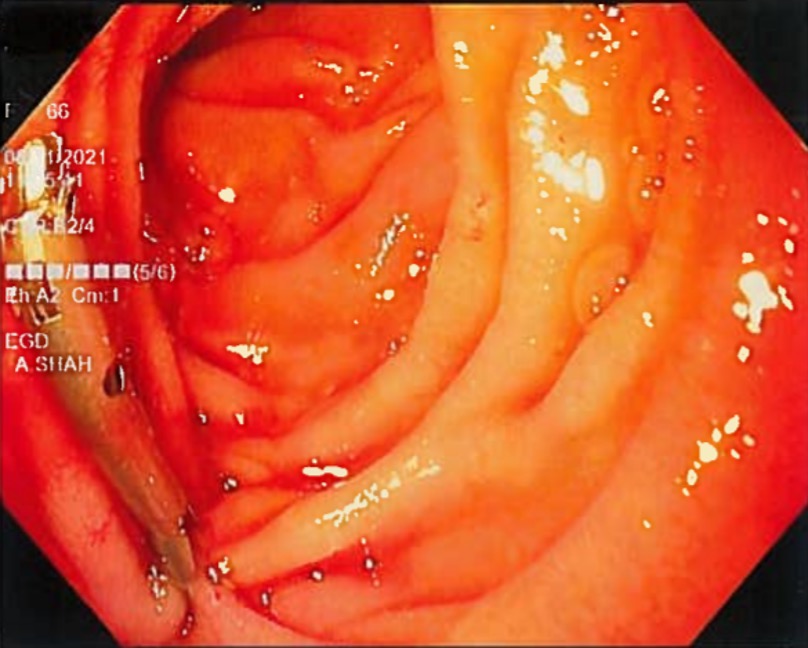
Figure: Figure 1: Migrated biliary stent puncturing anterior duodenal wall
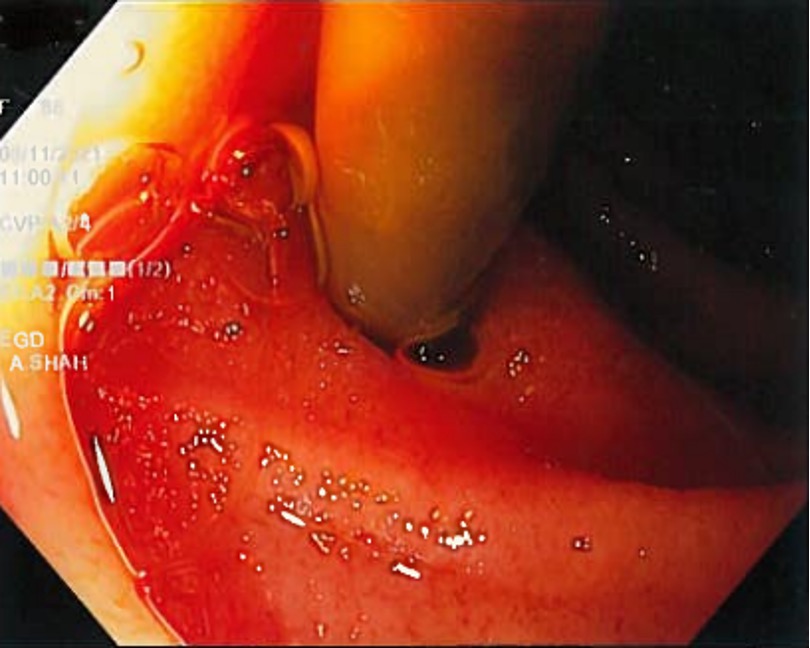
Figure: Figure 2: Endoscopic clip used with complete closure of fistula
Disclosures:
Alexander Satinsky indicated no relevant financial relationships.
Paul Kozak indicated no relevant financial relationships.
Ashish Shah indicated no relevant financial relationships.
Alexander Satinsky, DO1, Paul Kozak, DO1, Ashish Shah, MD2. P1444 - A Stent on the Move: Endoscopic Repair of Duodenal Perforation Due to Biliary Stent Migration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Riverside Medical Center, Kankakee, IL; 2Digestive Disease Consultants, Bourbonnais, IL
Introduction: Complications from ERCP can rarely include gastrointestinal perforation due to migrated biliary stent. Surgical repair is often used to repair duodenal perforations, however, minimally invasive endoscopic stent retrieval in the appropriate setting has become the preferred intervention. We present a case of a duodenal perforation resulting from a migrated biliary stent that was successfully repaired endoscopically.
Case Description/
Methods: A 66-year-old female with chronic conditions of COPD, CHF, and chronic Hepatitis C infection presented with right-sided abdominal pain radiating to her back. She was found to have an 8 mm calculus at the level of the pancreatic head with upstream intrahepatic and extrahepatic biliary ductal dilation. ERCP with sphincterotomy, balloon sweep, and 10 F x 7 cm plastic biliary stent placement was performed. She was deemed to be a poor surgical candidate for cholecystectomy given her comorbidities. Two weeks after discharge, the patient returned with severe left-sided flank pain. CT showed migration of the biliary stent with perforation of the duodenum. It was determined that the best course of action would be to remove the stent and clip the area of perforation endoscopically, with surgery available for emergent open laparotomy. On endoscopy, a migrated plastic biliary stent was observed puncturing through the anterior duodenal wall with mild ulceration in the second portion of the duodenum (figure 1). The intact stent was removed using rat toothed forceps. Afterward, a small 3 mm fistula was evident where the stent had punctured through the duodenal wall. One endoscopic clip was used with complete closure of the fistula (figure 2). The patient recovered remarkably well and was discharged one week after presentation.
Discussion: Stent migration typically results in benign passage through the GI tract; rarely, it can result in perforation. Intrinsic risks can include adhesions, hernias, and diverticula, and extrinsic can include material used. Management depends on several factors such as mechanism of perforation and clinical severity. While surgery is usually reserved for patients with peritonitis, endoscopy is a safe and effective therapy for migrated stent-associated perforation and is associated with faster recovery than a surgical approach. As the capabilities and expertise of endoscopy continue to evolve, management plans should be individualized and involve a minimally invasive approach when appropriate to maximize patient outcomes.
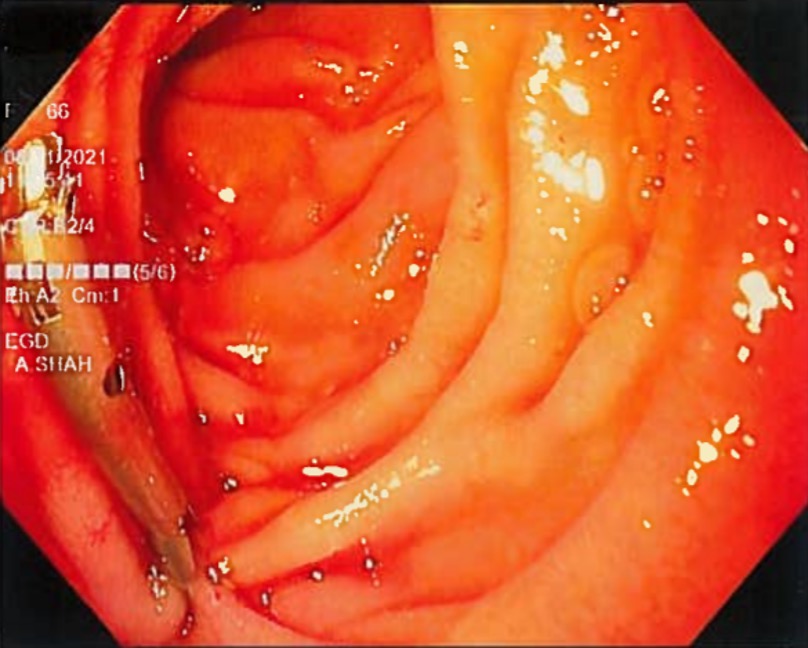
Figure: Figure 1: Migrated biliary stent puncturing anterior duodenal wall
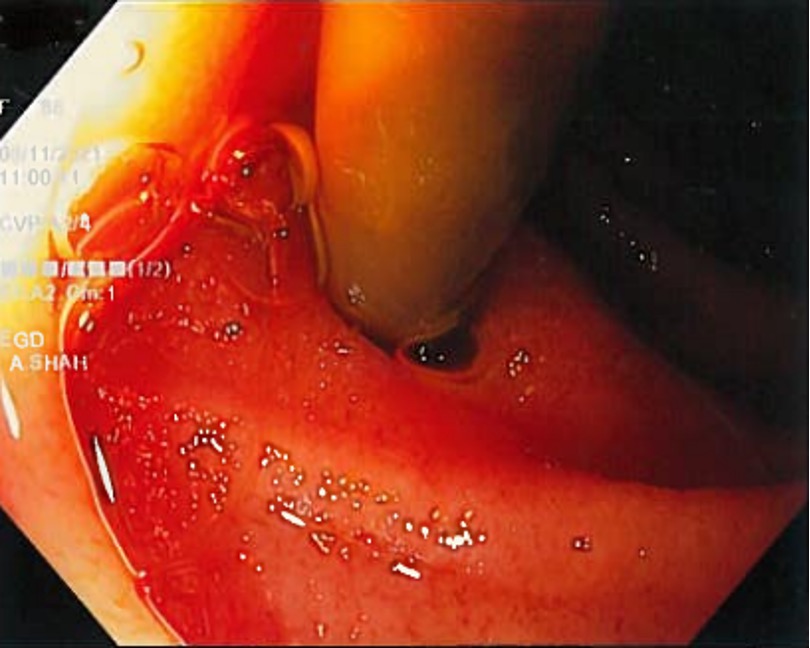
Figure: Figure 2: Endoscopic clip used with complete closure of fistula
Disclosures:
Alexander Satinsky indicated no relevant financial relationships.
Paul Kozak indicated no relevant financial relationships.
Ashish Shah indicated no relevant financial relationships.
Alexander Satinsky, DO1, Paul Kozak, DO1, Ashish Shah, MD2. P1444 - A Stent on the Move: Endoscopic Repair of Duodenal Perforation Due to Biliary Stent Migration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
