Sunday Poster Session
Category: Interventional Endoscopy
P1442 - High-grade Pyloric Stenosis in Adult Causing Partial Gastric Outlet Obstruction – Successfully Managed With Lumen Apposing Metal Stent (LAMS)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- ME
Muhammad Waqar Elahi, MD
West Virginia University School of Medicine
Morgantown, WV
Presenting Author(s)
Muhammad Waqar Elahi, MD1, Sundas Zahid, MD1, David Shi, MD1, Eric Huang, MD1, Bharath Bhushan, MD1, Hira Hameed, MD2, Aamer Ahmad, MD3, Ahmad Khan, 3, Shahryar Khan, MD4, Arooj Fatima, MD5
1West Virginia University School of Medicine, Morgantown, WV; 2Jinnah Hospital Lahore, Lahore, Punjab, Pakistan; 3Khyber Medical University, Peshawar, North-West Frontier, Pakistan; 4University of Kansas Medical Center, Kansas City, KS; 5Khyber Medical University, Morgantown, WV
Introduction: Idiopathic hypertrophic pyloric stenosis (IHPS) is a relatively common congenital disorder, usually presenting within the first few weeks of birth. However, adult idiopathic hypertrophic pyloric stenosis (AIHPS) is an extremely rare entity with only handful cases reported so far in the literature. We present a rare case of AIHPS with partial gastric outlet obstruction that was successfully managed with lumen apposing metal stent.
Case Description/
Methods: A female patient in 40s with complaints of chronic postprandial nausea, vomiting, dysphagia to solids, abdominal bloating, and discomfort initially presented to the outpatient gastroenterology office. Laboratory examination showed normal results. Barium swallow did not show any evidence of webs, rings, or strictures. The patient was admitted to our hospital for an EGD, which showed severe pyloric stenosis causing partial gastric outlet obstruction (GOO) [Figure-A]. Dilation up to 10 mm was then performed with simple pyloric balloon dilatation [Figure-B].
The patient was discharged home, but her symptoms persisted without any improvement. Three weeks later, a repeat EGD was performed which revealed similar findings of high-grade pyloric stenosis and GOO [Figure-C, 2 images]. A trans-pyloric Lumen Apposing Metal Stent (LAMS) was deployed and post-dilated to 15 mm with balloon catheter [Figure-D, 2 images].
After LAMS insertion, the patient was managed supportively during hospitalization and was discharged home. The patient reported gradual improvement in her symptoms at 3-month outpatient follow up visit in GI office and was tolerating regular solid diet well.
Discussion: We present an extremely rare case of high-grade adult idiopathic hypertrophic pyloric stenosis (AIHPS) with partial gastric outlet obstruction whose symptoms were significantly improved after endoscopic LAMS deployment. Although, currently, surgery is the preferred treatment modality, further research is warranted to compare endoscopic vs surgical techniques before finalizing a standard of care.
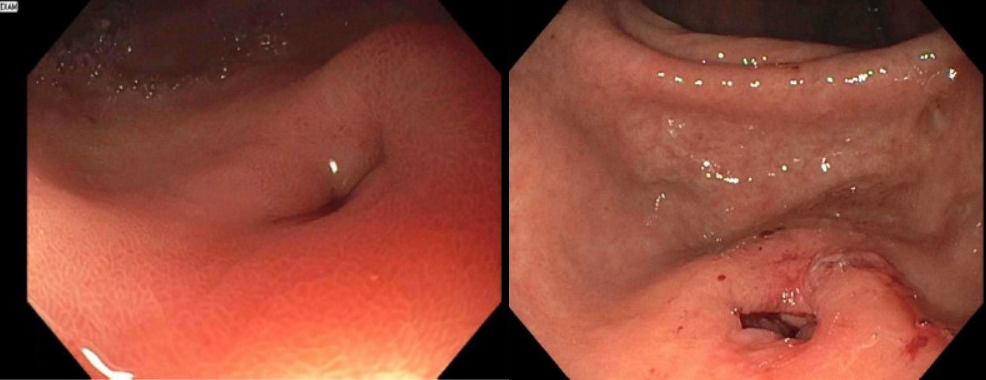
Figure: Figure-A (1st image): Endoscopic image showing severe pyloric stenosis and partial gastric outlet obstruction.
Figure-B (2nd image): EGD image showing pylorus after dilation with 8-9-10 mm pyloric balloon dilator.
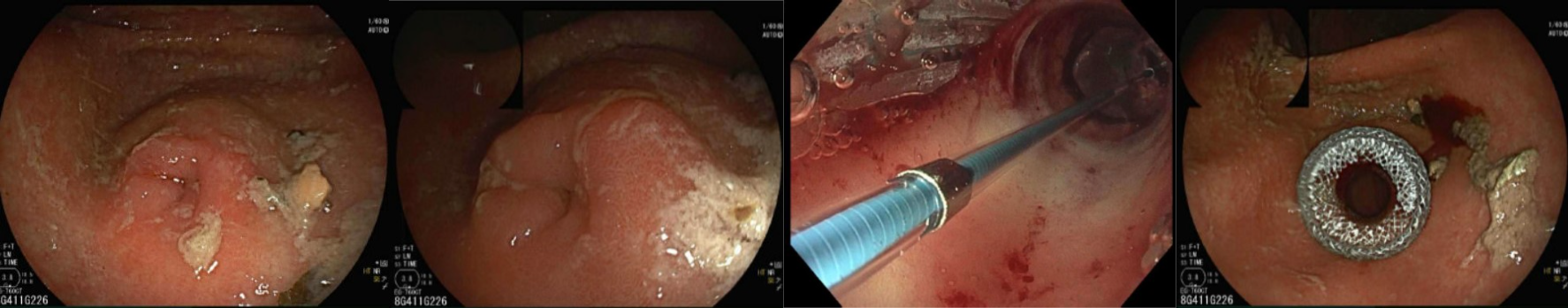
Figure: Figure-C (first 2 images): Images showing high-grade pyloric stenosis with partial gastric outlet obstruction and retained food particles.
Figure D (last 2 images): EGD images showing trans-pyloric Lumen Apposing Metal Stent (LAMS), dilated to 15 mm with balloon catheter.
Disclosures:
Muhammad Waqar Elahi indicated no relevant financial relationships.
Sundas Zahid indicated no relevant financial relationships.
David Shi indicated no relevant financial relationships.
Eric Huang indicated no relevant financial relationships.
Bharath Bhushan indicated no relevant financial relationships.
Hira Hameed indicated no relevant financial relationships.
Aamer Ahmad indicated no relevant financial relationships.
Ahmad Khan indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Arooj Fatima indicated no relevant financial relationships.
Muhammad Waqar Elahi, MD1, Sundas Zahid, MD1, David Shi, MD1, Eric Huang, MD1, Bharath Bhushan, MD1, Hira Hameed, MD2, Aamer Ahmad, MD3, Ahmad Khan, 3, Shahryar Khan, MD4, Arooj Fatima, MD5. P1442 - High-grade Pyloric Stenosis in Adult Causing Partial Gastric Outlet Obstruction – Successfully Managed With Lumen Apposing Metal Stent (LAMS), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1West Virginia University School of Medicine, Morgantown, WV; 2Jinnah Hospital Lahore, Lahore, Punjab, Pakistan; 3Khyber Medical University, Peshawar, North-West Frontier, Pakistan; 4University of Kansas Medical Center, Kansas City, KS; 5Khyber Medical University, Morgantown, WV
Introduction: Idiopathic hypertrophic pyloric stenosis (IHPS) is a relatively common congenital disorder, usually presenting within the first few weeks of birth. However, adult idiopathic hypertrophic pyloric stenosis (AIHPS) is an extremely rare entity with only handful cases reported so far in the literature. We present a rare case of AIHPS with partial gastric outlet obstruction that was successfully managed with lumen apposing metal stent.
Case Description/
Methods: A female patient in 40s with complaints of chronic postprandial nausea, vomiting, dysphagia to solids, abdominal bloating, and discomfort initially presented to the outpatient gastroenterology office. Laboratory examination showed normal results. Barium swallow did not show any evidence of webs, rings, or strictures. The patient was admitted to our hospital for an EGD, which showed severe pyloric stenosis causing partial gastric outlet obstruction (GOO) [Figure-A]. Dilation up to 10 mm was then performed with simple pyloric balloon dilatation [Figure-B].
The patient was discharged home, but her symptoms persisted without any improvement. Three weeks later, a repeat EGD was performed which revealed similar findings of high-grade pyloric stenosis and GOO [Figure-C, 2 images]. A trans-pyloric Lumen Apposing Metal Stent (LAMS) was deployed and post-dilated to 15 mm with balloon catheter [Figure-D, 2 images].
After LAMS insertion, the patient was managed supportively during hospitalization and was discharged home. The patient reported gradual improvement in her symptoms at 3-month outpatient follow up visit in GI office and was tolerating regular solid diet well.
Discussion: We present an extremely rare case of high-grade adult idiopathic hypertrophic pyloric stenosis (AIHPS) with partial gastric outlet obstruction whose symptoms were significantly improved after endoscopic LAMS deployment. Although, currently, surgery is the preferred treatment modality, further research is warranted to compare endoscopic vs surgical techniques before finalizing a standard of care.
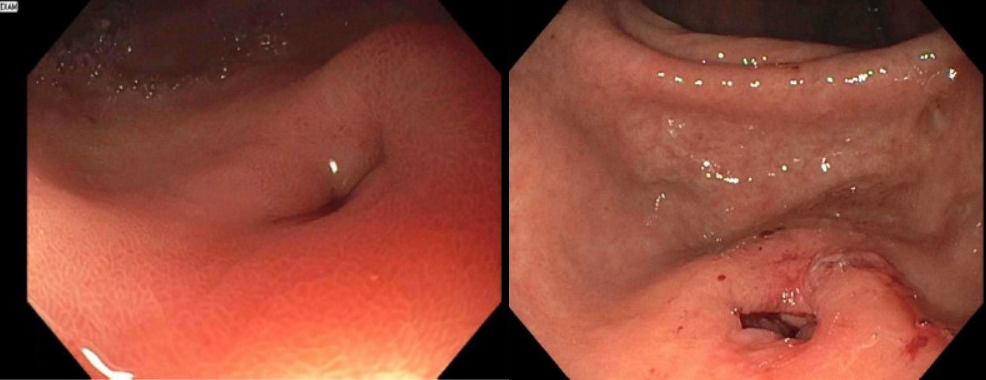
Figure: Figure-A (1st image): Endoscopic image showing severe pyloric stenosis and partial gastric outlet obstruction.
Figure-B (2nd image): EGD image showing pylorus after dilation with 8-9-10 mm pyloric balloon dilator.
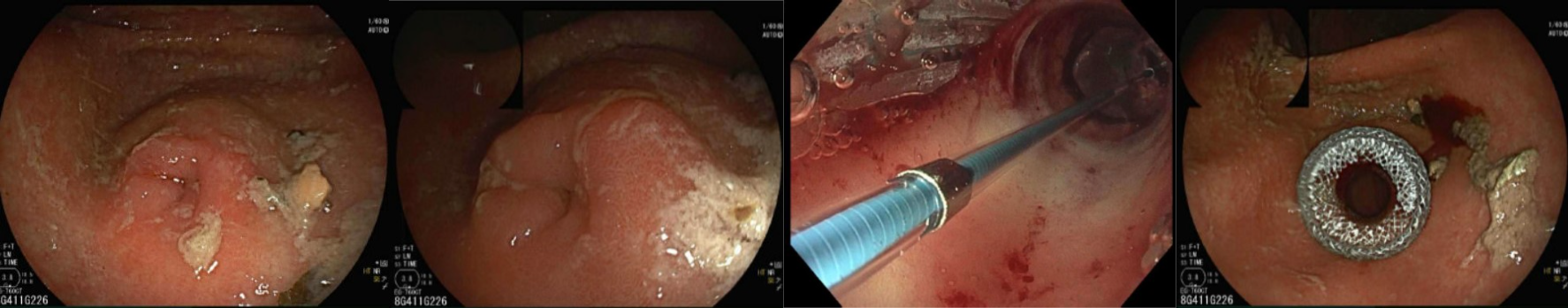
Figure: Figure-C (first 2 images): Images showing high-grade pyloric stenosis with partial gastric outlet obstruction and retained food particles.
Figure D (last 2 images): EGD images showing trans-pyloric Lumen Apposing Metal Stent (LAMS), dilated to 15 mm with balloon catheter.
Disclosures:
Muhammad Waqar Elahi indicated no relevant financial relationships.
Sundas Zahid indicated no relevant financial relationships.
David Shi indicated no relevant financial relationships.
Eric Huang indicated no relevant financial relationships.
Bharath Bhushan indicated no relevant financial relationships.
Hira Hameed indicated no relevant financial relationships.
Aamer Ahmad indicated no relevant financial relationships.
Ahmad Khan indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Arooj Fatima indicated no relevant financial relationships.
Muhammad Waqar Elahi, MD1, Sundas Zahid, MD1, David Shi, MD1, Eric Huang, MD1, Bharath Bhushan, MD1, Hira Hameed, MD2, Aamer Ahmad, MD3, Ahmad Khan, 3, Shahryar Khan, MD4, Arooj Fatima, MD5. P1442 - High-grade Pyloric Stenosis in Adult Causing Partial Gastric Outlet Obstruction – Successfully Managed With Lumen Apposing Metal Stent (LAMS), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
