Sunday Poster Session
Category: Interventional Endoscopy
P1432 - Use of Endoscopic Ultrasound (EUS) Guided-Gastro-Gastric Lumen Apposing Metal Stent (LAMS) as a Gateway for Resection of Large Duodenal Polyp in a Patient With Roux-en-Y-Gastric Bypass: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamad Khaled Almujarkesh, MD
AdventHealth
Orlando, FL
Presenting Author(s)
Mohamad Khaled Almujarkesh, MD1, Abdullah Abbasi, MD2, Saurabh Chandan, MD2, Mustafa Arain, MD2, Muhammad Hasan, MD, FACG2
1AdventHealth, Orlando, FL; 2Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL
Introduction: Management of duodenal polyps in patients with Roux-en-Y gastric bypass (RYGB) can be challenging due to altered anatomy. We report a case of successful endoscopic resection of a large duodenal polyp, using a novel approach that involves endoscopic ultrasound (EUS)-guided gastro-gastric lumen-apposing metal stent (LAMS) placement as a gateway.
Case Description/
Methods: A 60-year-old woman with multiple comorbidities and a remote history of RYGB presented with iron deficiency anemia. Esophagogastroduodenoscopy showed a normal gastric pouch with an intact staple line and healthy anastomoses, while colonoscopy revealed diverticulosis and non-bleeding hemorrhoids. Capsule endoscopy identified mid-jejunum ulcers. Double-balloon enteroscopy found a large ( >50 mm), semi-pedunculated duodenal bulb polyp (Paris Is, Pit III), which biopsy confirmed as a tubulovillous adenoma (TVA) without high-grade dysplasia.
Due to the polyp’s size, location, scope looping, and lack of compatible tools, endoscopic resection was not possible. Due to her comorbidities, the Whipple procedure was considered too risky. After a multidisciplinary discussion, a staged, minimally invasive approach was taken. First, EUS-guided placement of a 20 mm × 10 mm LAMS provided access to the excluded stomach and duodenum. Endoscopic resection was performed through the stent four weeks after tract maturation. After submucosal injection of hetastarch and methylene blue, piecemeal snare resection of a 55 mm area was performed, and tissue retrieval. Hemostasis was achieved with four clips and a coagulation grasper. Pathology confirmed TVA without high-grade dysplasia or malignancy. At follow-up, there was no recurrence, and the gastro-gastric LAMS was removed.
Discussion: Although Device-Assisted Enteroscopy (DAE), including spiral and balloon-assisted techniques, improves visualization in altered anatomy, Endotherapy and polyp resection using DAE can be challenging and carry risks such as perforation and incomplete resection.
EUS-guided LAMS placement offers a novel solution by creating a temporary gastro-gastric fistula, allowing access to standard endoscopic interventions. Our case highlights its potential utility in approaching duodenal polyps and performing resection in patients with altered anatomy.

Figure: Figure 1: Endoscopic image showing a duodenal polyp measuring 17 × 17 mm at its largest cross-sectional dimension.
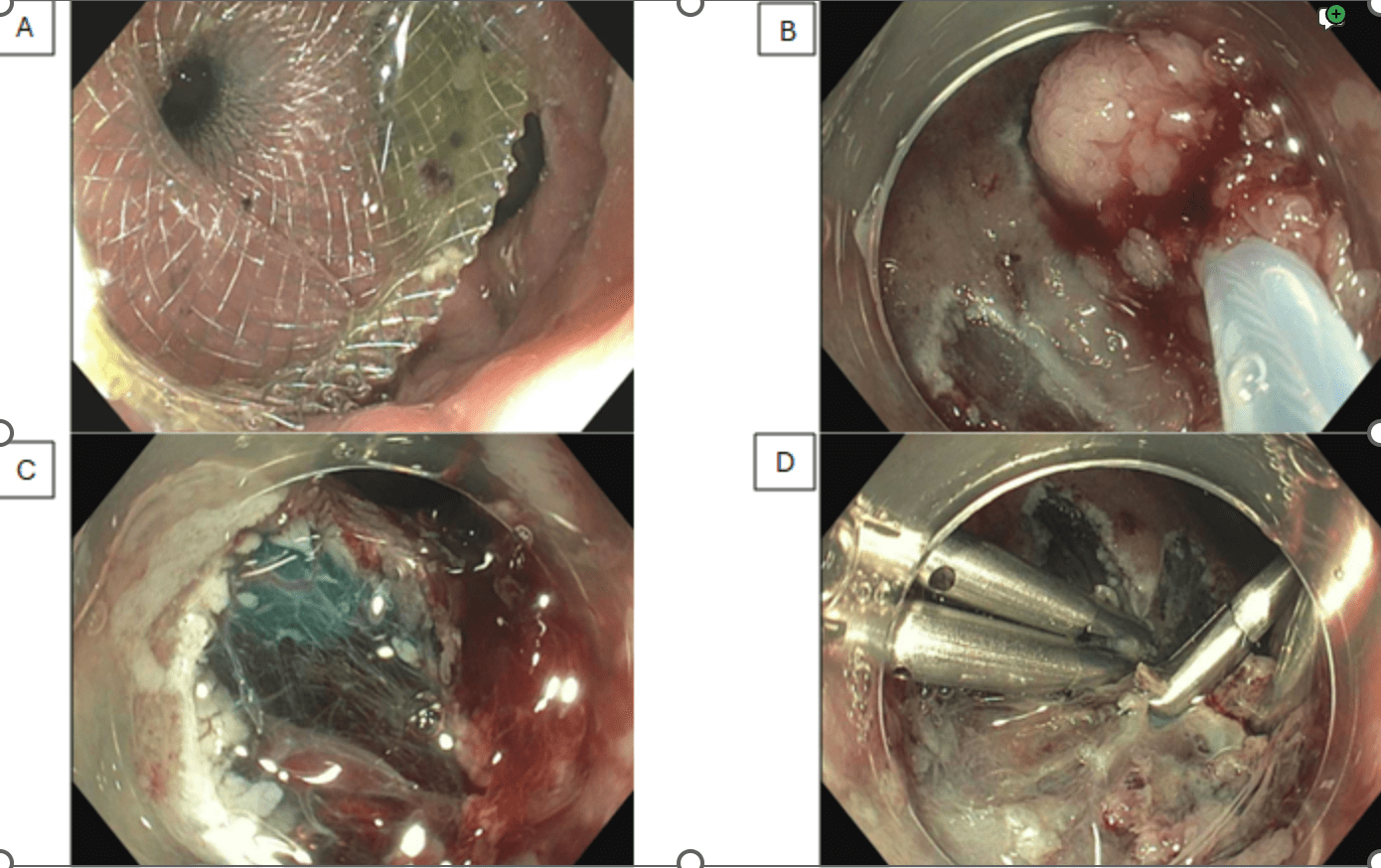
Figure: Figure 2: A. EUS-guided placement of a 20 mm × 10 mm gastro-gastric lumen-apposing metal stent (LAMS). B. showing piecemeal mucosal resection of a 50 mm sessile duodenal polyp (Paris Is, Pit pattern Type III) C. A 55 mm area was successfully resected using a snare. D. Successful closure of the post-resection mucosal defect. Four hemostatic clips were applied to achieve effective hemostasis and defect approximation
Disclosures:
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Abdullah Abbasi indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
Muhammad Hasan: Boston Scientific – Consultant. MicroTech Endoscopy – Consultant. Olympus America – Consultant.
Mohamad Khaled Almujarkesh, MD1, Abdullah Abbasi, MD2, Saurabh Chandan, MD2, Mustafa Arain, MD2, Muhammad Hasan, MD, FACG2. P1432 - Use of Endoscopic Ultrasound (EUS) Guided-Gastro-Gastric Lumen Apposing Metal Stent (LAMS) as a Gateway for Resection of Large Duodenal Polyp in a Patient With Roux-en-Y-Gastric Bypass: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1AdventHealth, Orlando, FL; 2Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL
Introduction: Management of duodenal polyps in patients with Roux-en-Y gastric bypass (RYGB) can be challenging due to altered anatomy. We report a case of successful endoscopic resection of a large duodenal polyp, using a novel approach that involves endoscopic ultrasound (EUS)-guided gastro-gastric lumen-apposing metal stent (LAMS) placement as a gateway.
Case Description/
Methods: A 60-year-old woman with multiple comorbidities and a remote history of RYGB presented with iron deficiency anemia. Esophagogastroduodenoscopy showed a normal gastric pouch with an intact staple line and healthy anastomoses, while colonoscopy revealed diverticulosis and non-bleeding hemorrhoids. Capsule endoscopy identified mid-jejunum ulcers. Double-balloon enteroscopy found a large ( >50 mm), semi-pedunculated duodenal bulb polyp (Paris Is, Pit III), which biopsy confirmed as a tubulovillous adenoma (TVA) without high-grade dysplasia.
Due to the polyp’s size, location, scope looping, and lack of compatible tools, endoscopic resection was not possible. Due to her comorbidities, the Whipple procedure was considered too risky. After a multidisciplinary discussion, a staged, minimally invasive approach was taken. First, EUS-guided placement of a 20 mm × 10 mm LAMS provided access to the excluded stomach and duodenum. Endoscopic resection was performed through the stent four weeks after tract maturation. After submucosal injection of hetastarch and methylene blue, piecemeal snare resection of a 55 mm area was performed, and tissue retrieval. Hemostasis was achieved with four clips and a coagulation grasper. Pathology confirmed TVA without high-grade dysplasia or malignancy. At follow-up, there was no recurrence, and the gastro-gastric LAMS was removed.
Discussion: Although Device-Assisted Enteroscopy (DAE), including spiral and balloon-assisted techniques, improves visualization in altered anatomy, Endotherapy and polyp resection using DAE can be challenging and carry risks such as perforation and incomplete resection.
EUS-guided LAMS placement offers a novel solution by creating a temporary gastro-gastric fistula, allowing access to standard endoscopic interventions. Our case highlights its potential utility in approaching duodenal polyps and performing resection in patients with altered anatomy.

Figure: Figure 1: Endoscopic image showing a duodenal polyp measuring 17 × 17 mm at its largest cross-sectional dimension.
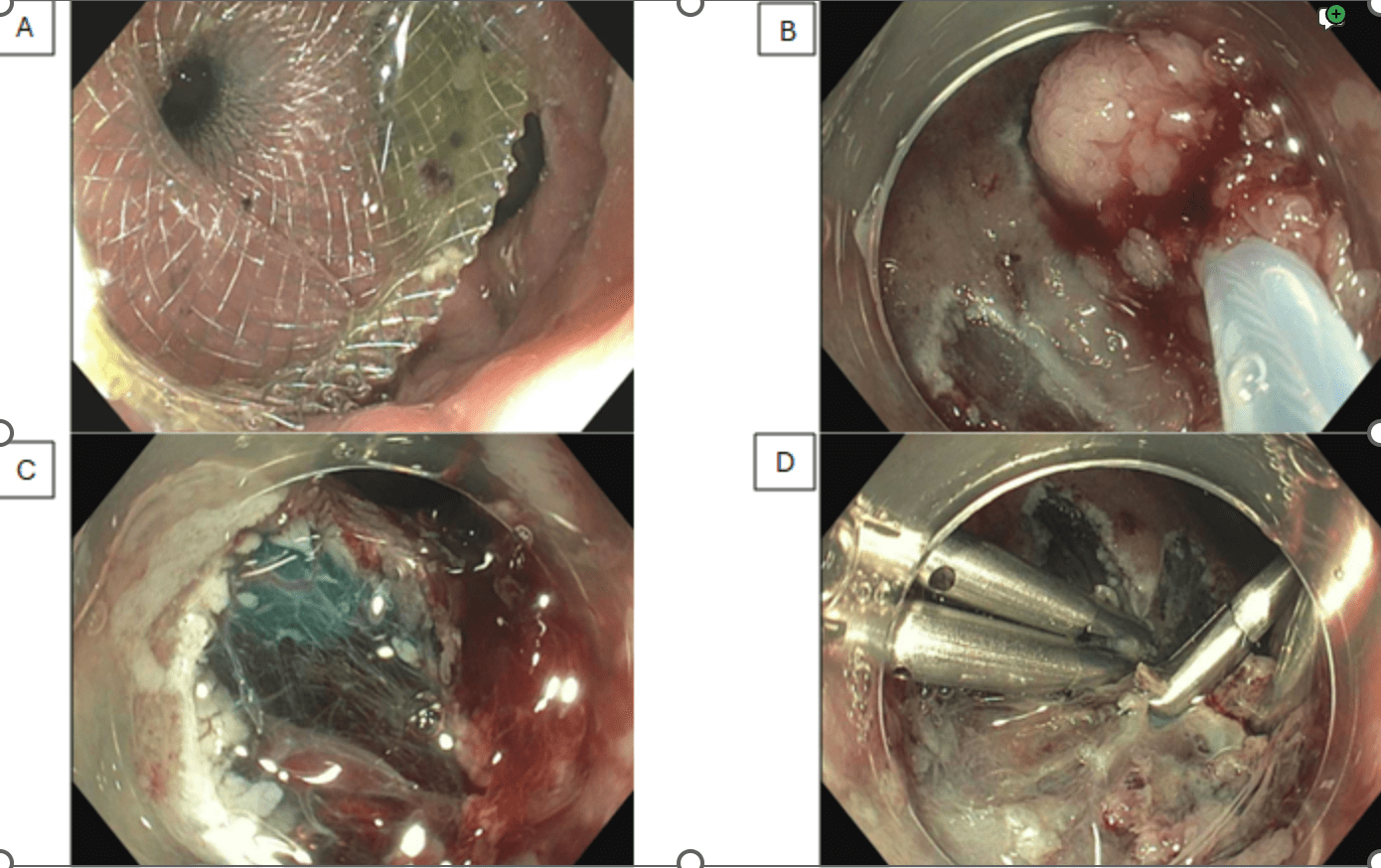
Figure: Figure 2: A. EUS-guided placement of a 20 mm × 10 mm gastro-gastric lumen-apposing metal stent (LAMS). B. showing piecemeal mucosal resection of a 50 mm sessile duodenal polyp (Paris Is, Pit pattern Type III) C. A 55 mm area was successfully resected using a snare. D. Successful closure of the post-resection mucosal defect. Four hemostatic clips were applied to achieve effective hemostasis and defect approximation
Disclosures:
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Abdullah Abbasi indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
Muhammad Hasan: Boston Scientific – Consultant. MicroTech Endoscopy – Consultant. Olympus America – Consultant.
Mohamad Khaled Almujarkesh, MD1, Abdullah Abbasi, MD2, Saurabh Chandan, MD2, Mustafa Arain, MD2, Muhammad Hasan, MD, FACG2. P1432 - Use of Endoscopic Ultrasound (EUS) Guided-Gastro-Gastric Lumen Apposing Metal Stent (LAMS) as a Gateway for Resection of Large Duodenal Polyp in a Patient With Roux-en-Y-Gastric Bypass: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
