Sunday Poster Session
Category: Interventional Endoscopy
P1430 - Esophageal Stenting for Dysphagia in Aggressive Multicentric Castleman’s Disease: A Case Complicated by Perforation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- HS
Hamzah Shariff, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Hamzah Shariff, MD, Tina Boortalary, MD, Anand Kumar, MD, MPH
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Multicentric Castleman’s disease (MCD) is a rare lymphoproliferative disorder marked by systemic inflammation and widespread lymphadenopathy. While multi-organ involvement is common, structural gastrointestinal compression—particularly esophageal—is infrequently reported. We present a rare case of idiopathic MCD complicated by superior vena cava (SVC) syndrome that progressed to esophageal compression requiring stenting, further complicated by esophageal perforation post-treatment.
Case Description/
Methods: A 54-year-old male with untreated idiopathic MCD complicated by SVC syndrome managed with radiotherapy and SVC stenting presented with acute dysphagia to solids and liquids and weight loss. On exam, he was tachycardic and cachectic, without palpable lymphadenopathy. Labs showed WBC 15, CRP 17, and IL-6 787. CT chest and esophagogram revealed bulky mediastinal lymphadenopathy and a right hilar mass causing esophageal compression confirmed on esophagogastroduodenoscopy (EGD) (Figure 1). Endoscopic ultrasound showed a 4x2 cm mediastinal mass invading the esophageal wall. A fully covered self-expanding metal stent (FCSEMS) was placed, and cytology confirmed lymphoid tissue. His dysphagia resolved, and he was discharged on steroids with a plan for routine siltuximab infusions.
Two months later, the patient re-presented with hemoptysis. CT chest suggested a fistula between the right mainstem bronchus and esophagus with T1–T2 osteomyelitis. Right bronchial artery embolization resolved the bleeding. EGD confirmed a mediastinal fistula upon stent removal, and a new FCSEMS was placed (Figure 2.). The patient declined endoscopic vacuum therapy (EVT) and definitive esophageal surgery at this time. He will have an endoscopy with stent removal in 2 months for reassessment.
Discussion: Esophageal compression from MCD is rare and often reported in unicentric forms. Dysphagia is an uncommon symptom in MCD, with limited reports of stenting for such presentations. The advanced nature of MCD with esophageal wall involvement, use of steroids, and compression of the esophageal wall between the MCD and stent may have increased the risk for mediastinal fistula. Stent-related fistulas not amenable to primary endoscopic repair may require stent replacement or EVT, definitive surgical bypass and nutritional support. This case emphasizes endoscopic evaluation of dysphagia in MCD, an unusual finding, and if possible, to avoid stenting in aggressive disease to reduce the risk of complications.
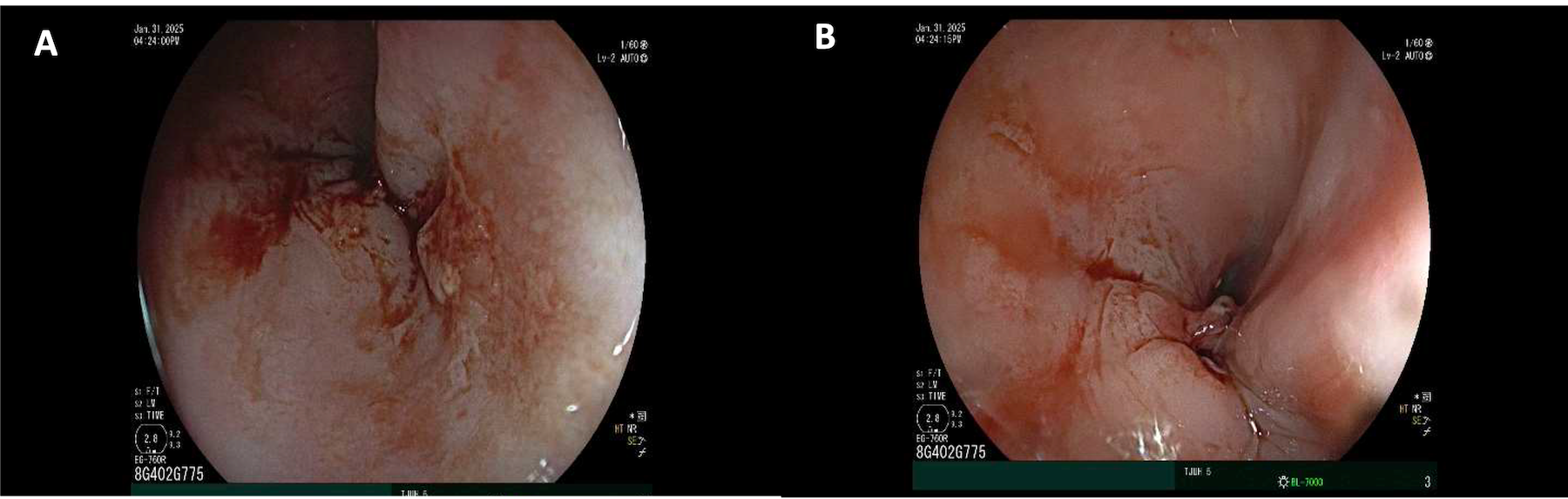
Figure: Figure 1. Upper endoscopy confirming partial stenosis of the middle esophagus from compression by enlarging lymph nodes
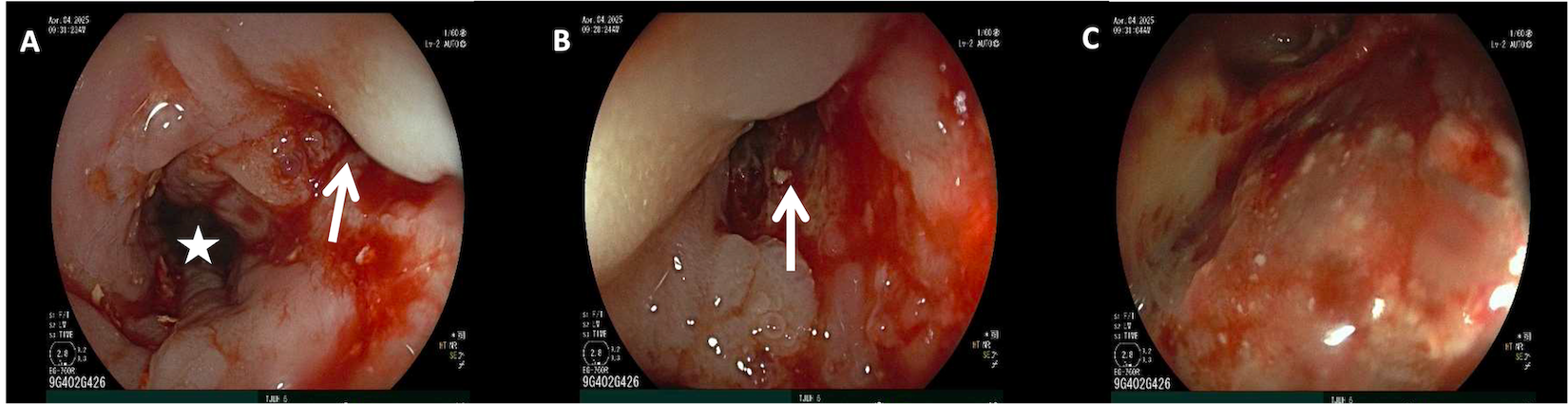
Figure: Figure 2. Upper endoscopy post-FCSEMS removal demonstrated narrow but open esophageal lumen (* in A) with a perforation (arrows in A and B) that led into a mediastinal cavity (C) with moderate liquid debris
Disclosures:
Hamzah Shariff indicated no relevant financial relationships.
Tina Boortalary indicated no relevant financial relationships.
Anand Kumar: Boston Scientific – Consultant. Olympus – Consultant. Pentax – Paid Speaker.
Hamzah Shariff, MD, Tina Boortalary, MD, Anand Kumar, MD, MPH. P1430 - Esophageal Stenting for Dysphagia in Aggressive Multicentric Castleman’s Disease: A Case Complicated by Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Multicentric Castleman’s disease (MCD) is a rare lymphoproliferative disorder marked by systemic inflammation and widespread lymphadenopathy. While multi-organ involvement is common, structural gastrointestinal compression—particularly esophageal—is infrequently reported. We present a rare case of idiopathic MCD complicated by superior vena cava (SVC) syndrome that progressed to esophageal compression requiring stenting, further complicated by esophageal perforation post-treatment.
Case Description/
Methods: A 54-year-old male with untreated idiopathic MCD complicated by SVC syndrome managed with radiotherapy and SVC stenting presented with acute dysphagia to solids and liquids and weight loss. On exam, he was tachycardic and cachectic, without palpable lymphadenopathy. Labs showed WBC 15, CRP 17, and IL-6 787. CT chest and esophagogram revealed bulky mediastinal lymphadenopathy and a right hilar mass causing esophageal compression confirmed on esophagogastroduodenoscopy (EGD) (Figure 1). Endoscopic ultrasound showed a 4x2 cm mediastinal mass invading the esophageal wall. A fully covered self-expanding metal stent (FCSEMS) was placed, and cytology confirmed lymphoid tissue. His dysphagia resolved, and he was discharged on steroids with a plan for routine siltuximab infusions.
Two months later, the patient re-presented with hemoptysis. CT chest suggested a fistula between the right mainstem bronchus and esophagus with T1–T2 osteomyelitis. Right bronchial artery embolization resolved the bleeding. EGD confirmed a mediastinal fistula upon stent removal, and a new FCSEMS was placed (Figure 2.). The patient declined endoscopic vacuum therapy (EVT) and definitive esophageal surgery at this time. He will have an endoscopy with stent removal in 2 months for reassessment.
Discussion: Esophageal compression from MCD is rare and often reported in unicentric forms. Dysphagia is an uncommon symptom in MCD, with limited reports of stenting for such presentations. The advanced nature of MCD with esophageal wall involvement, use of steroids, and compression of the esophageal wall between the MCD and stent may have increased the risk for mediastinal fistula. Stent-related fistulas not amenable to primary endoscopic repair may require stent replacement or EVT, definitive surgical bypass and nutritional support. This case emphasizes endoscopic evaluation of dysphagia in MCD, an unusual finding, and if possible, to avoid stenting in aggressive disease to reduce the risk of complications.
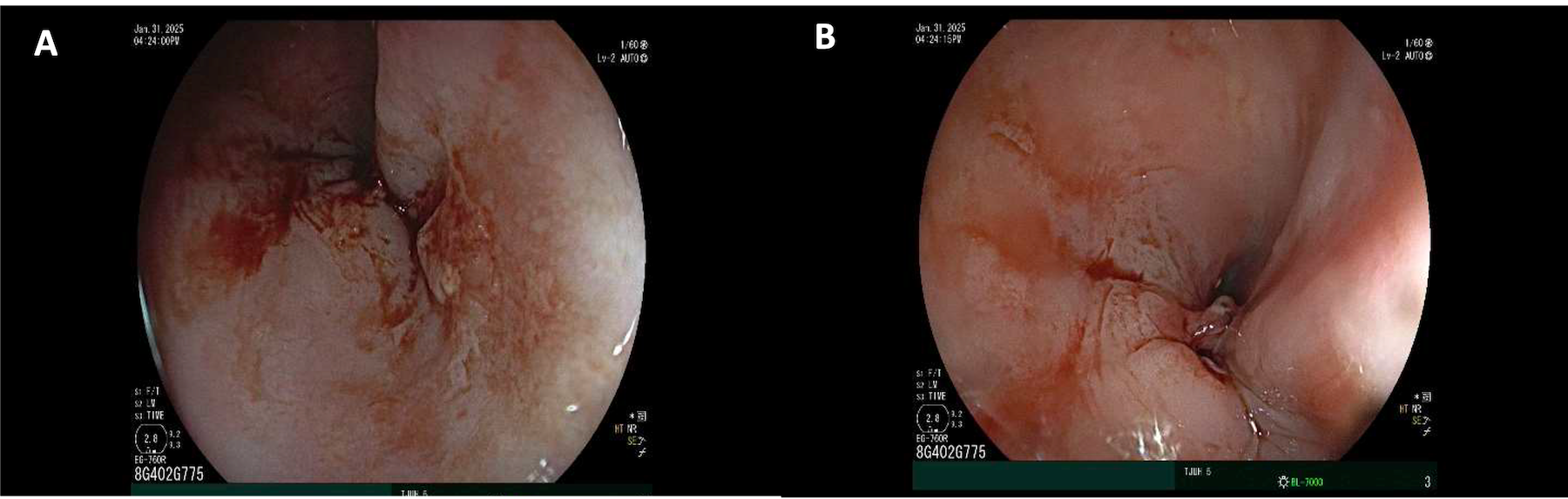
Figure: Figure 1. Upper endoscopy confirming partial stenosis of the middle esophagus from compression by enlarging lymph nodes
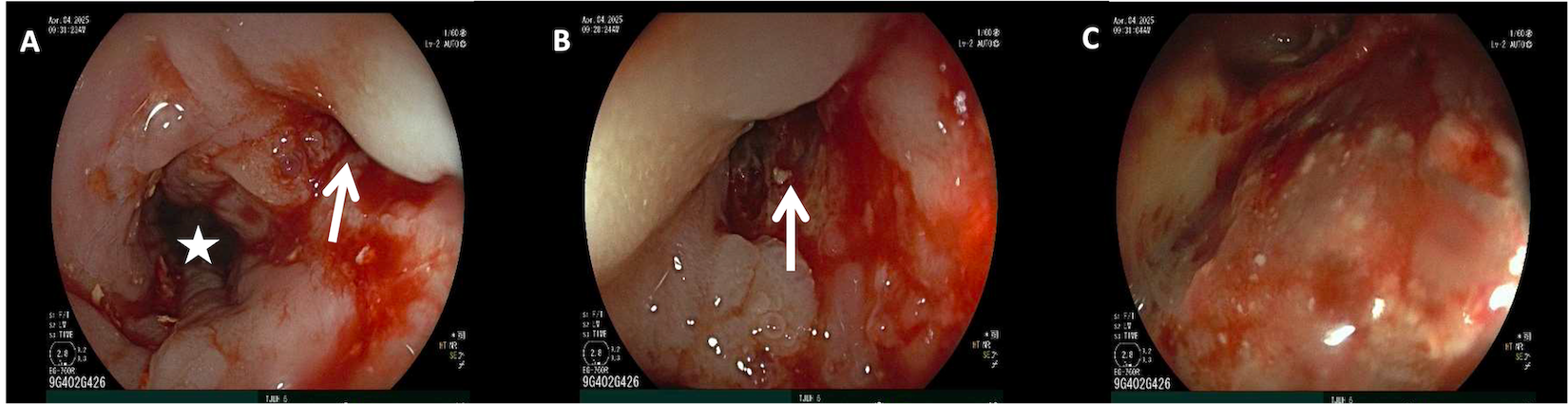
Figure: Figure 2. Upper endoscopy post-FCSEMS removal demonstrated narrow but open esophageal lumen (* in A) with a perforation (arrows in A and B) that led into a mediastinal cavity (C) with moderate liquid debris
Disclosures:
Hamzah Shariff indicated no relevant financial relationships.
Tina Boortalary indicated no relevant financial relationships.
Anand Kumar: Boston Scientific – Consultant. Olympus – Consultant. Pentax – Paid Speaker.
Hamzah Shariff, MD, Tina Boortalary, MD, Anand Kumar, MD, MPH. P1430 - Esophageal Stenting for Dysphagia in Aggressive Multicentric Castleman’s Disease: A Case Complicated by Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
