Sunday Poster Session
Category: Interventional Endoscopy
P1417 - Peptide-Based Hemostatic Gel for Bleeding Prophylaxis in Non-Ampullary Duodenal Adenoma Resection: Single Center Experience
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JL
Jake Levne, MD
University of Florida Health Shands Hospital
Gainesville, FL
Presenting Author(s)
Jake Levne, MD1, Tiffany Chua, MD2, Matthew Giansiracusa, DO1, Aleksey Novikov, MD3
1University of Florida Health Shands Hospital, Gainesville, FL; 2University of Florida, Gainesville, FL; 3University of Florida College of Medicine, Gainesville, FL
Introduction: Non-ampullary duodenal adenomas can cause malignancy and are removed if they are >6 mm via endoscopic mucosal resection (EMR). EMR can cause bleeding and perforation. Traditionally, hemostatic clips have been used to decrease these risks. A novel peptide hemostatic gel holds promise as an effective hemostatic agent. This study sought to evaluate our experience with this novel agent.
Methods: All non-ampullary duodenal adenomas of size 10 mm or greater that were resected at our center between 01/01/2020 to 10/31/2024 were included. In total, 70 adenomas resected from 59 patients were included. Patient, polyp, and procedural characteristics are described in Table 1. Normality was assessed using the Shapiro-Wilk test. Comparisons for continuous variables were conducted using the Mann-Whitney U test for non-parametric data. Categorical data were analyzed using the chi-square test. A p-value < 0.05 was considered statistically significant. All analyses were performed using Stata 16.1 (College Station, Tx).
Results: Patient demographics were similar between groups (table 1). 82.9% (58/70) patients did not get hemostatic gel vs 17.1% (12/70) who did. En bloc resection was achieved in 32.8% (19/58) and 16.7% (2/12) of cases, respectively. Lesion characteristics, including location, size, morphology, were comparable between groups. There were no instances of malignancy on histology. Lesions >25 mm were present in 44.8% (26/58) of the non-gel group and 33.3% (4/12) of the gel group. Most lesions were in the second part of the duodenum: 58.6% (34/58) in the non-gel group vs. 66.7% (8/12) in the gel group. Lesions involving >50% of the duodenal circumference were more common in the non-gel group: 29.3% (17/58) vs. 16.7% (2/12). Recurrence among those who underwent repeat EGD (N=48) was observed in 39.5% (15/38) of cases in the non-gel group and 20% (2/10) in the gel group over median 6 month endoscopic follow up. Bleeding occurred in 13.8% (8/58) and 16.7% (2/12) of cases in the non-gel and gel groups, respectively.
Discussion: The statistical analysis did not find that peptide hemostatic gel was independently associated with a change in the risk of bleeding or adenoma recurrence. It is possible that hemostatic gel is non-inferior to other methodologies. We want to point out the trend towards decreased adenoma recurrence with use of the hemostatic gel. Future randomized controlled trials evaluating role of the hemostatic gel should include adenoma recurrence.
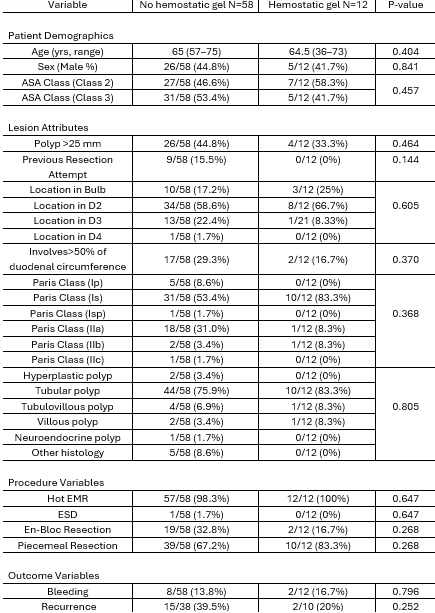
Figure: Table 1: Comparisons of Hemostatic Gel Vs No Hemostatic Gel
Disclosures:
Jake Levne indicated no relevant financial relationships.
Tiffany Chua indicated no relevant financial relationships.
Matthew Giansiracusa indicated no relevant financial relationships.
Aleksey Novikov indicated no relevant financial relationships.
Jake Levne, MD1, Tiffany Chua, MD2, Matthew Giansiracusa, DO1, Aleksey Novikov, MD3. P1417 - Peptide-Based Hemostatic Gel for Bleeding Prophylaxis in Non-Ampullary Duodenal Adenoma Resection: Single Center Experience, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Florida Health Shands Hospital, Gainesville, FL; 2University of Florida, Gainesville, FL; 3University of Florida College of Medicine, Gainesville, FL
Introduction: Non-ampullary duodenal adenomas can cause malignancy and are removed if they are >6 mm via endoscopic mucosal resection (EMR). EMR can cause bleeding and perforation. Traditionally, hemostatic clips have been used to decrease these risks. A novel peptide hemostatic gel holds promise as an effective hemostatic agent. This study sought to evaluate our experience with this novel agent.
Methods: All non-ampullary duodenal adenomas of size 10 mm or greater that were resected at our center between 01/01/2020 to 10/31/2024 were included. In total, 70 adenomas resected from 59 patients were included. Patient, polyp, and procedural characteristics are described in Table 1. Normality was assessed using the Shapiro-Wilk test. Comparisons for continuous variables were conducted using the Mann-Whitney U test for non-parametric data. Categorical data were analyzed using the chi-square test. A p-value < 0.05 was considered statistically significant. All analyses were performed using Stata 16.1 (College Station, Tx).
Results: Patient demographics were similar between groups (table 1). 82.9% (58/70) patients did not get hemostatic gel vs 17.1% (12/70) who did. En bloc resection was achieved in 32.8% (19/58) and 16.7% (2/12) of cases, respectively. Lesion characteristics, including location, size, morphology, were comparable between groups. There were no instances of malignancy on histology. Lesions >25 mm were present in 44.8% (26/58) of the non-gel group and 33.3% (4/12) of the gel group. Most lesions were in the second part of the duodenum: 58.6% (34/58) in the non-gel group vs. 66.7% (8/12) in the gel group. Lesions involving >50% of the duodenal circumference were more common in the non-gel group: 29.3% (17/58) vs. 16.7% (2/12). Recurrence among those who underwent repeat EGD (N=48) was observed in 39.5% (15/38) of cases in the non-gel group and 20% (2/10) in the gel group over median 6 month endoscopic follow up. Bleeding occurred in 13.8% (8/58) and 16.7% (2/12) of cases in the non-gel and gel groups, respectively.
Discussion: The statistical analysis did not find that peptide hemostatic gel was independently associated with a change in the risk of bleeding or adenoma recurrence. It is possible that hemostatic gel is non-inferior to other methodologies. We want to point out the trend towards decreased adenoma recurrence with use of the hemostatic gel. Future randomized controlled trials evaluating role of the hemostatic gel should include adenoma recurrence.
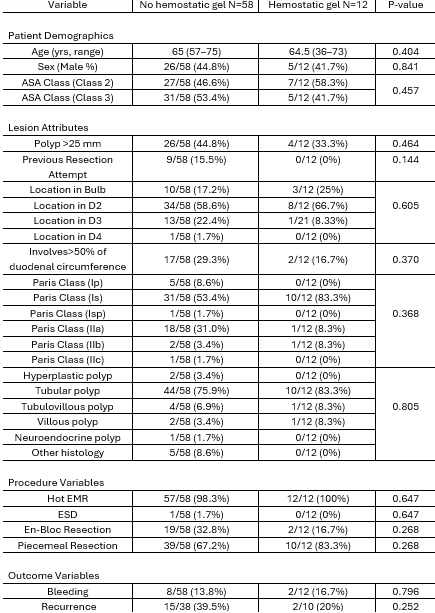
Figure: Table 1: Comparisons of Hemostatic Gel Vs No Hemostatic Gel
Disclosures:
Jake Levne indicated no relevant financial relationships.
Tiffany Chua indicated no relevant financial relationships.
Matthew Giansiracusa indicated no relevant financial relationships.
Aleksey Novikov indicated no relevant financial relationships.
Jake Levne, MD1, Tiffany Chua, MD2, Matthew Giansiracusa, DO1, Aleksey Novikov, MD3. P1417 - Peptide-Based Hemostatic Gel for Bleeding Prophylaxis in Non-Ampullary Duodenal Adenoma Resection: Single Center Experience, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
