Sunday Poster Session
Category: Interventional Endoscopy
P1401 - To Close or Not to Close: A Systematic Review and Meta-Analysis of Outcomes Following Mucosal Defect Closure After Gastric ESD
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Harsimran Kalsi, MD (she/her/hers)
University of Central Florida
Gainesville, FL
Presenting Author(s)
Harsimran Kalsi, MD1, Yeshika Thapa, MD1, Smit Deliwala, MD2, Tony Brar, MD1, Yaseen Perbtani, DO3, Saurabh Chandan, MD4, Amrita Sethi, MD5, Rashmi Advani, MD6
1University of Central Florida, Gainesville, FL; 2Emory University School of Medicine, Atlanta, GA; 3University of Central Florida, HCA Healthcare GME, Gainesville, FL; 4Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Orlando, FL; 5Columbia University Irving Medical Center, New York, NY; 6Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Endoscopic submucosal dissection (ESD) is a widely accepted therapeutic modality for the management of precancerous and early gastric cancer. However, it results in artificial ulcers, which increase the risk of delayed bleeding and perforation. While prophylactic closure of post-ESD defects has demonstrated benefit in colonic lesions, the clinical value of defect closure in the gastric setting remains uncertain. We conducted a systematic review and meta-analysis to evaluate the impact of defect closure versus non-closure following gastric ESD on clinical outcomes.
Methods: A systematically searched databases to identify studies comparing closure versus non-closure of mucosal defects following gastric ESD. Primary outcomes included delayed bleeding and delayed perforation. Pooled estimates were calculated using a random-effects model. Effect measures were reported as risk ratios (RR) and standardized mean differences (SMD), with 95% confidence intervals (CI). Statistical heterogeneity was assessed using the I² statistic.
Results: A total of 7 studies comprising 1,951 patients (N=888 Closure, N=1063 Non-Closure) were included. The closure group had 77.3% males, while the non-closure group had 79.4%. Mean age was 73.3 ± 6.5 years in the closure and 71.8 ± 6.2 in the non-closure group. Analysis revealed a significantly lower delayed bleeding rate in the closure group compared to the non-closure group (3.0% vs. 12.4%; RR 0.29, 95% CI: 0.11–0.73, p = 0.009; I² = 68.9). The rate of delayed perforation was 0% in both groups. There were no significant differences between groups in specimen size (SMD -0.17, 95% CI: -0.52–0.77; p = 0.34) or procedure time (SMD 0.34, 95% CI: -0.52–1.19; p = 0.45). In the closure group, complete closure rate was 90% (75.7–96.3), sustained closure rate was 69.9% (45.3–86.6), and mean closure time was 23.8 minutes (17.8–29.8).
Discussion: Closure of the mucosal defect following gastric ESD significantly reduces the risk of delayed bleeding. This benefit appears consistent across closure techniques and diverse patient populations, supporting its consideration as a routine adjunct, particularly in patients at elevated bleeding risk. Further studies are warranted to determine the optimal closure methods and to establish standardized protocols.
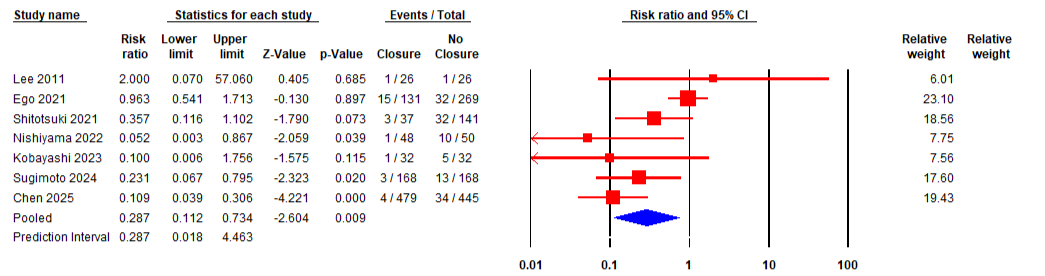
Figure: Figure 1: Forest Plot of Delayed Bleeding
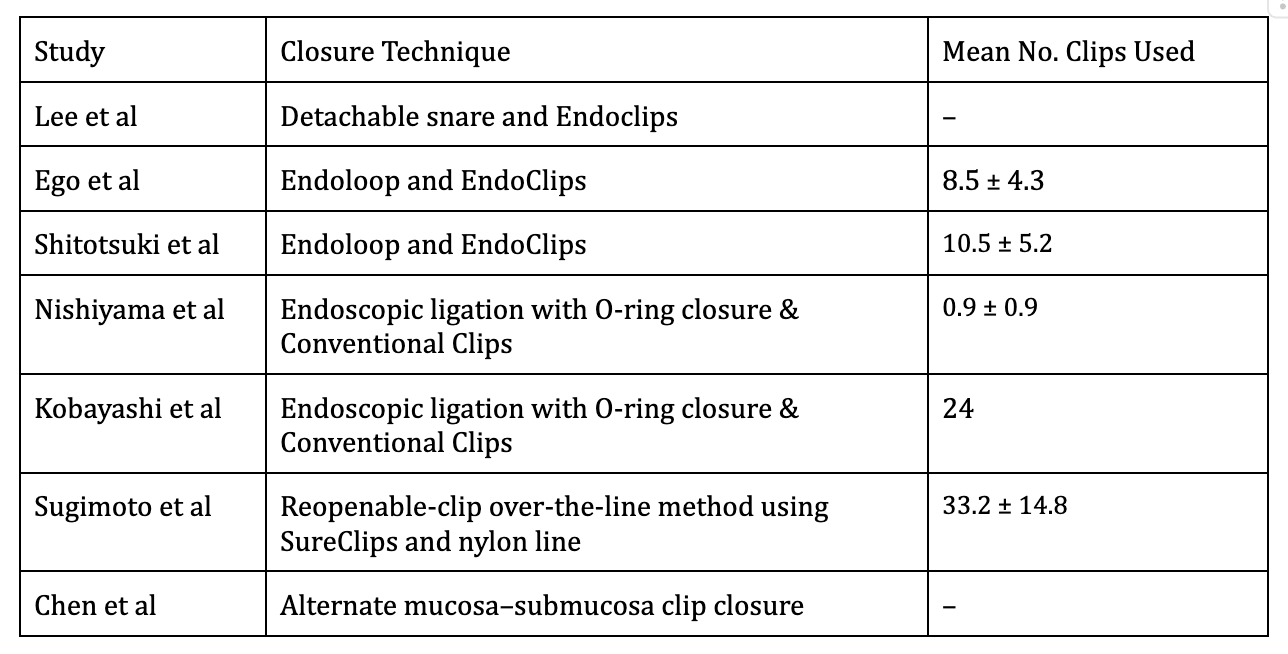
Figure: Table 1: Gastric ESD closure methods along with mean number of clips used across the studies
Disclosures:
Harsimran Kalsi indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Smit Deliwala indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Amrita Sethi indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Harsimran Kalsi, MD1, Yeshika Thapa, MD1, Smit Deliwala, MD2, Tony Brar, MD1, Yaseen Perbtani, DO3, Saurabh Chandan, MD4, Amrita Sethi, MD5, Rashmi Advani, MD6. P1401 - To Close or Not to Close: A Systematic Review and Meta-Analysis of Outcomes Following Mucosal Defect Closure After Gastric ESD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, Gainesville, FL; 2Emory University School of Medicine, Atlanta, GA; 3University of Central Florida, HCA Healthcare GME, Gainesville, FL; 4Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Orlando, FL; 5Columbia University Irving Medical Center, New York, NY; 6Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Endoscopic submucosal dissection (ESD) is a widely accepted therapeutic modality for the management of precancerous and early gastric cancer. However, it results in artificial ulcers, which increase the risk of delayed bleeding and perforation. While prophylactic closure of post-ESD defects has demonstrated benefit in colonic lesions, the clinical value of defect closure in the gastric setting remains uncertain. We conducted a systematic review and meta-analysis to evaluate the impact of defect closure versus non-closure following gastric ESD on clinical outcomes.
Methods: A systematically searched databases to identify studies comparing closure versus non-closure of mucosal defects following gastric ESD. Primary outcomes included delayed bleeding and delayed perforation. Pooled estimates were calculated using a random-effects model. Effect measures were reported as risk ratios (RR) and standardized mean differences (SMD), with 95% confidence intervals (CI). Statistical heterogeneity was assessed using the I² statistic.
Results: A total of 7 studies comprising 1,951 patients (N=888 Closure, N=1063 Non-Closure) were included. The closure group had 77.3% males, while the non-closure group had 79.4%. Mean age was 73.3 ± 6.5 years in the closure and 71.8 ± 6.2 in the non-closure group. Analysis revealed a significantly lower delayed bleeding rate in the closure group compared to the non-closure group (3.0% vs. 12.4%; RR 0.29, 95% CI: 0.11–0.73, p = 0.009; I² = 68.9). The rate of delayed perforation was 0% in both groups. There were no significant differences between groups in specimen size (SMD -0.17, 95% CI: -0.52–0.77; p = 0.34) or procedure time (SMD 0.34, 95% CI: -0.52–1.19; p = 0.45). In the closure group, complete closure rate was 90% (75.7–96.3), sustained closure rate was 69.9% (45.3–86.6), and mean closure time was 23.8 minutes (17.8–29.8).
Discussion: Closure of the mucosal defect following gastric ESD significantly reduces the risk of delayed bleeding. This benefit appears consistent across closure techniques and diverse patient populations, supporting its consideration as a routine adjunct, particularly in patients at elevated bleeding risk. Further studies are warranted to determine the optimal closure methods and to establish standardized protocols.
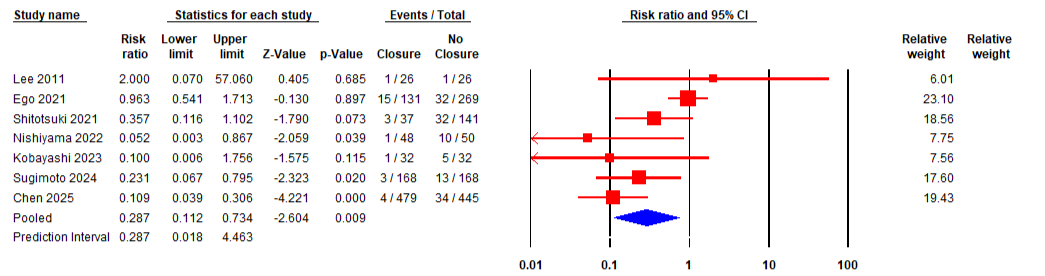
Figure: Figure 1: Forest Plot of Delayed Bleeding
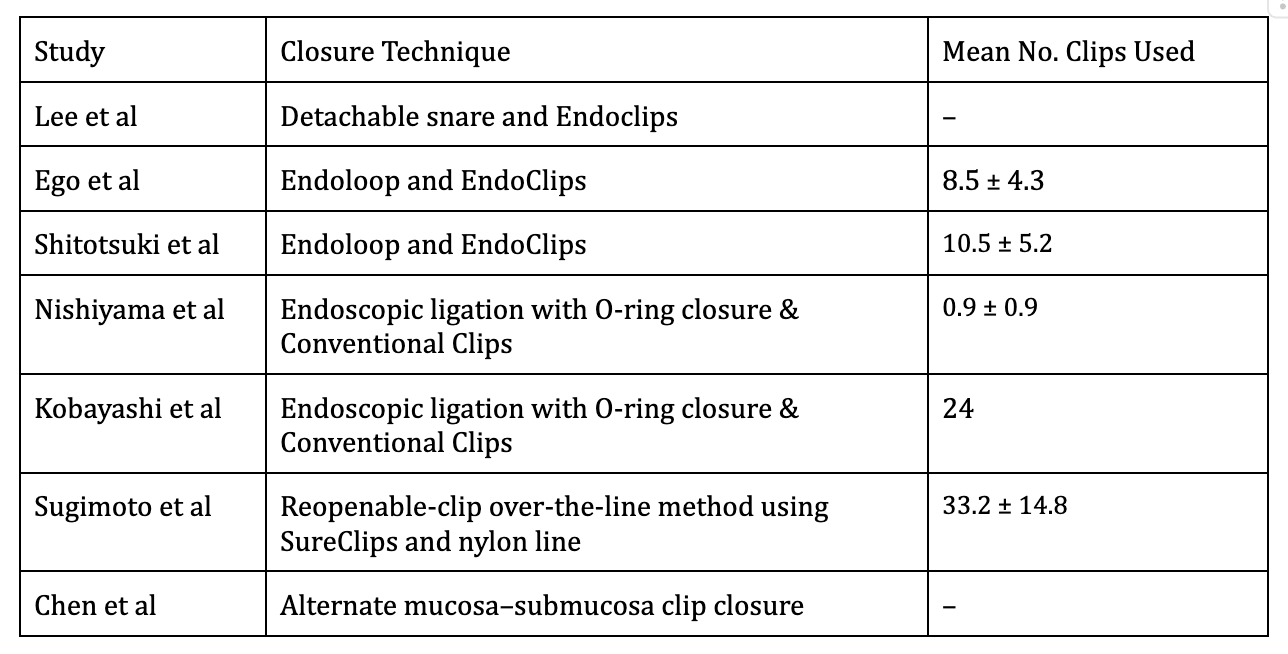
Figure: Table 1: Gastric ESD closure methods along with mean number of clips used across the studies
Disclosures:
Harsimran Kalsi indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Smit Deliwala indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Amrita Sethi indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Harsimran Kalsi, MD1, Yeshika Thapa, MD1, Smit Deliwala, MD2, Tony Brar, MD1, Yaseen Perbtani, DO3, Saurabh Chandan, MD4, Amrita Sethi, MD5, Rashmi Advani, MD6. P1401 - To Close or Not to Close: A Systematic Review and Meta-Analysis of Outcomes Following Mucosal Defect Closure After Gastric ESD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
