Sunday Poster Session
Category: Interventional Endoscopy
P1375 - Comparative Outcomes of Endoscopic Ultrasound-Guided vs Endoscopic Retrograde Cholangiopancreatography Biliary Drainage in Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis of RCTs
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Prince K. Darko, MD, MSc
Piedmont Athens Regional
Athens, GA
Presenting Author(s)
Prince Darko, MD, MSc1, Elizabeth Soladoye, MD, MPH1, Samuel Acheampong, MD, MSc1, Naveen Anand, MD2
1Piedmont Athens Regional, Athens, GA; 2Piedmont Advanced Gastroenterology Atlanta, Atlanta, GA
Introduction: Malignant biliary obstruction (MBO) is a serious complication of cancers involving the pancreas, bile ducts, or ampullary area. Endoscopic retrograde cholangiopancreatography (ERCP) remains the traditional approach to biliary drainage but is sometimes limited by tumor-related anatomical challenges and advanced tumor progression. Endoscopic ultrasound-guided biliary drainage (EUS-BD), initially used after failed ERCP, has gained traction as a primary option due to its potential to bypass these challenges
Methods: A meta-analysis was performed according to PRISMA guidelines. Seven randomized controlled trials (RCTs) comparing EUS-BD and ERCP-BD in patients with MBO were included. Primary outcome was technical success while secondary outcomes included clinical success, adverse events, procedural duration, hospital stay, stent patency, and need for subsequent reintervention. Statistical analysis was performed using RevMan 5.4. Heterogeneity was assessed with the I² statistic, and random- or fixed-effects models were applied accordingly.
Results: Seven RCTs encompassing 621 patients (313 EUS-BD, 308 ERCP-BD) were analyzed. Technical success was significantly higher in the EUS-BD group (OR: 2.33; 95% CI: 1.32–4.13; P=0.004). Clinical success was similar between groups (OR: 1.12; 95% CI: 0.65–1.95; P=0.68). EUS-BD had shorter procedure time (MD: -6.89 minutes; P=0.004) and shorter hospital stay (MD: -1.23 days; P=0.006). Reintervention was significantly lower with EUS-BD (OR: 0.54; P=0.02), while adverse event rates and stent patency showed no significant difference.
Discussion: EUS-BD had higher technical success and lower reintervention compared to ERCP-BD, suggesting it may be a viable first-line alternative, especially in complex cases. Despite similar safety and efficacy, the procedural and therapeutic advantages of EUS-BD;shorter duration and higher technical success, highlight its growing clinical relevance. Further large-scale, multicenter trials are needed to confirm long-term benefits and standardize outcome definitions.
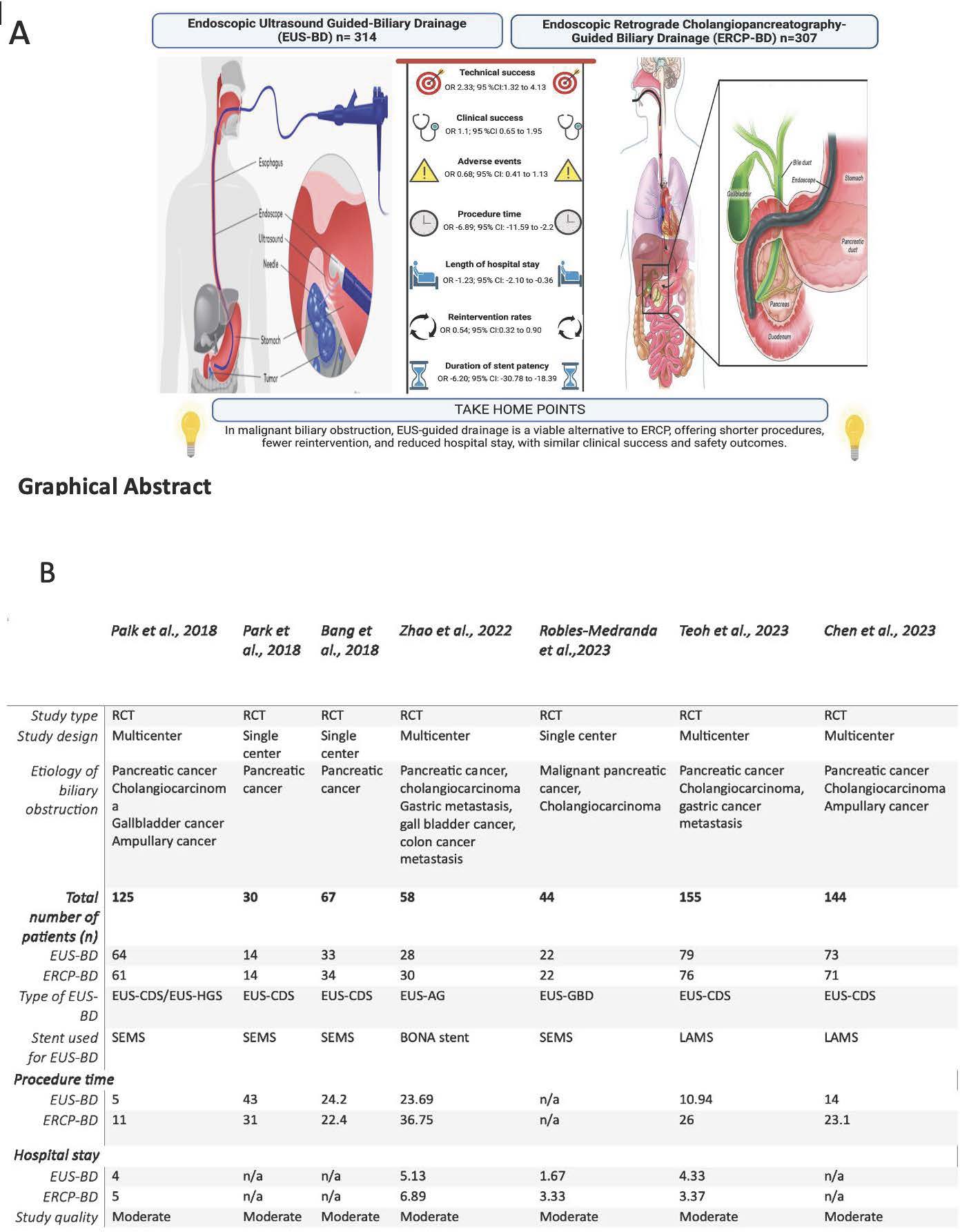
Figure: A- Graphical Abstract and B-Table showing data characteristics of included studies.

Figure: Forest plots of endoscopic ultrasound-guided biliary drainage versus endoscopic retrograde cholangiopancreatography guided drainage. (A) Technical success , (B) Clinical success (C) Adverse Effects, (D) Procedural time and (E)Length of hospital stay . Technical success was significantly higher with EUS-BD compared with ERCP-BD. CI, Confidence interval; df, degrees of freedom; ERCP-BD, Endoscopic retrograde cholangiopancreatography-guided biliary drainage; EUS-BD, Endoscopic ultrasound-guided biliary drainage; MH, Mantel-Haenszel; OR, risk ratio
Disclosures:
Prince Darko indicated no relevant financial relationships.
Elizabeth Soladoye indicated no relevant financial relationships.
Samuel Acheampong indicated no relevant financial relationships.
Naveen Anand indicated no relevant financial relationships.
Prince Darko, MD, MSc1, Elizabeth Soladoye, MD, MPH1, Samuel Acheampong, MD, MSc1, Naveen Anand, MD2. P1375 - Comparative Outcomes of Endoscopic Ultrasound-Guided vs Endoscopic Retrograde Cholangiopancreatography Biliary Drainage in Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis of RCTs, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Piedmont Athens Regional, Athens, GA; 2Piedmont Advanced Gastroenterology Atlanta, Atlanta, GA
Introduction: Malignant biliary obstruction (MBO) is a serious complication of cancers involving the pancreas, bile ducts, or ampullary area. Endoscopic retrograde cholangiopancreatography (ERCP) remains the traditional approach to biliary drainage but is sometimes limited by tumor-related anatomical challenges and advanced tumor progression. Endoscopic ultrasound-guided biliary drainage (EUS-BD), initially used after failed ERCP, has gained traction as a primary option due to its potential to bypass these challenges
Methods: A meta-analysis was performed according to PRISMA guidelines. Seven randomized controlled trials (RCTs) comparing EUS-BD and ERCP-BD in patients with MBO were included. Primary outcome was technical success while secondary outcomes included clinical success, adverse events, procedural duration, hospital stay, stent patency, and need for subsequent reintervention. Statistical analysis was performed using RevMan 5.4. Heterogeneity was assessed with the I² statistic, and random- or fixed-effects models were applied accordingly.
Results: Seven RCTs encompassing 621 patients (313 EUS-BD, 308 ERCP-BD) were analyzed. Technical success was significantly higher in the EUS-BD group (OR: 2.33; 95% CI: 1.32–4.13; P=0.004). Clinical success was similar between groups (OR: 1.12; 95% CI: 0.65–1.95; P=0.68). EUS-BD had shorter procedure time (MD: -6.89 minutes; P=0.004) and shorter hospital stay (MD: -1.23 days; P=0.006). Reintervention was significantly lower with EUS-BD (OR: 0.54; P=0.02), while adverse event rates and stent patency showed no significant difference.
Discussion: EUS-BD had higher technical success and lower reintervention compared to ERCP-BD, suggesting it may be a viable first-line alternative, especially in complex cases. Despite similar safety and efficacy, the procedural and therapeutic advantages of EUS-BD;shorter duration and higher technical success, highlight its growing clinical relevance. Further large-scale, multicenter trials are needed to confirm long-term benefits and standardize outcome definitions.
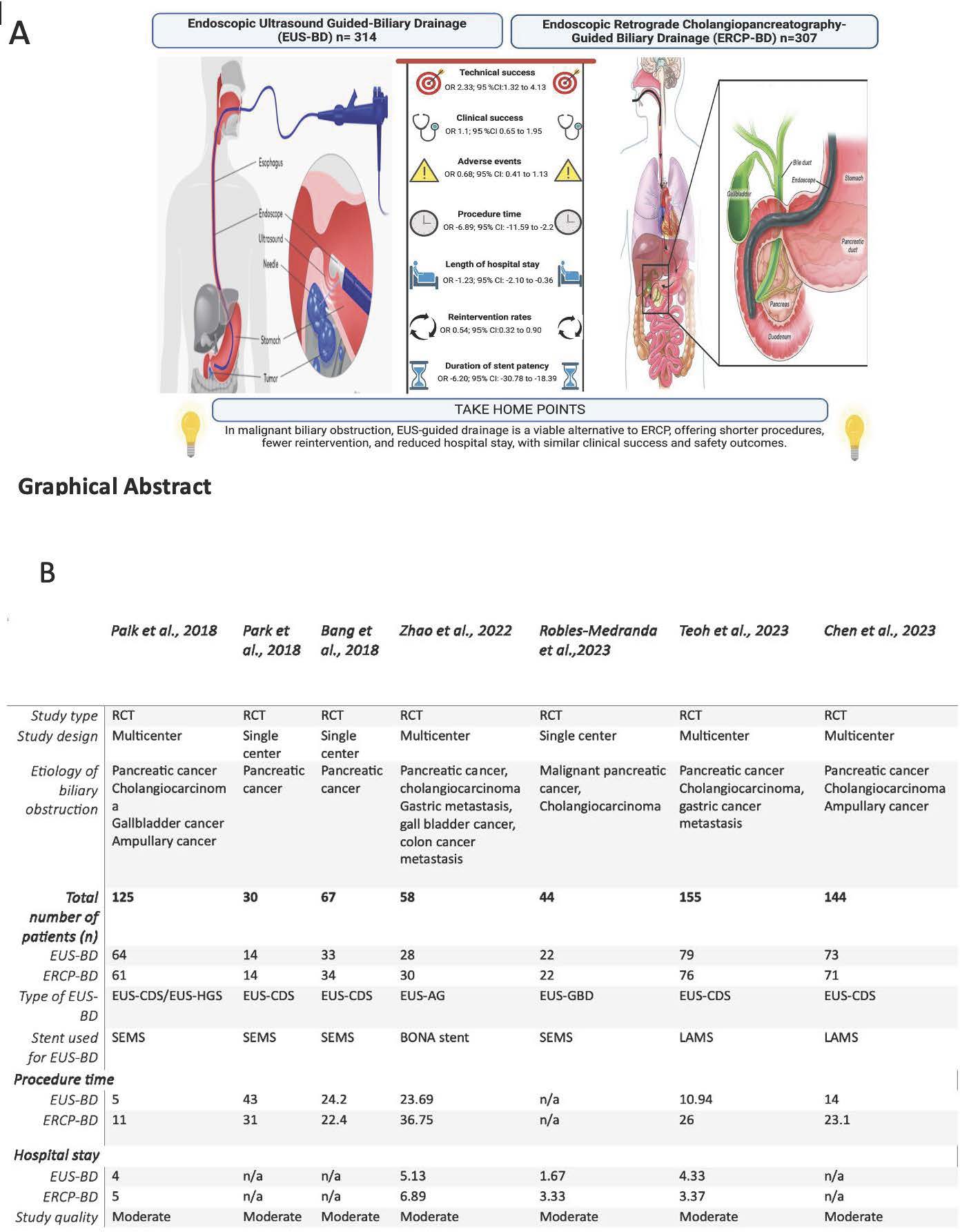
Figure: A- Graphical Abstract and B-Table showing data characteristics of included studies.

Figure: Forest plots of endoscopic ultrasound-guided biliary drainage versus endoscopic retrograde cholangiopancreatography guided drainage. (A) Technical success , (B) Clinical success (C) Adverse Effects, (D) Procedural time and (E)Length of hospital stay . Technical success was significantly higher with EUS-BD compared with ERCP-BD. CI, Confidence interval; df, degrees of freedom; ERCP-BD, Endoscopic retrograde cholangiopancreatography-guided biliary drainage; EUS-BD, Endoscopic ultrasound-guided biliary drainage; MH, Mantel-Haenszel; OR, risk ratio
Disclosures:
Prince Darko indicated no relevant financial relationships.
Elizabeth Soladoye indicated no relevant financial relationships.
Samuel Acheampong indicated no relevant financial relationships.
Naveen Anand indicated no relevant financial relationships.
Prince Darko, MD, MSc1, Elizabeth Soladoye, MD, MPH1, Samuel Acheampong, MD, MSc1, Naveen Anand, MD2. P1375 - Comparative Outcomes of Endoscopic Ultrasound-Guided vs Endoscopic Retrograde Cholangiopancreatography Biliary Drainage in Malignant Biliary Obstruction: A Systematic Review and Meta-Analysis of RCTs, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
