Sunday Poster Session
Category: Interventional Endoscopy
P1374 - Critical Timing of Endoscopic Retrograde Cholangiopancreatography in Acute Cholangitis: Early Procedures Yield Better Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Dinuka Bandara, DO
Creighton University School of Medicine
Scottsdale, AZ
Presenting Author(s)
Silpa Choday, MD1, Dinuka Bandara, DO2, Gautam Maddineni, MD3, Osama Abdur Rehman, MD3, Fnu Aakash, MD3, Ramandeep Sandhu, MD1, Indu Srinivasan, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University School of Medicine, Scottsdale, AZ; 3Florida State University, Cape Coral, FL
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is a critical procedure for diagnosing and treating various pancreatobiliary disorders. This study assesses the effect of early vs late ERCP on mortality and readmissions in acute cholangitis.
Methods: We used a National Readmissions Database (2016 -2021) to identify acute cholangitis who underwent therapeutic ERCP within one week of admission. Early ERCP was defined as ERCP performed on the same day of admission or the next day (days 0 or 1, < 48 h), and late ERCP was performed on days 2 to 7 of admission. Multivariate logistic regression was used to calculate the ERCP timing
Results: A total of 330,046 records are analyzed, out of which 38,339 have 30-day readmissions with acute cholangitis. Of these, 53% had early ERCP, while 47% had late ERCP. Patients undergoing early ERCP were significantly younger than those undergoing late ERCP (mean age 29 vs. 42 years, p=0.01). The late ERCP group had a significantly higher proportion of males (55% vs. 49%, p=0.03) and differing health insurance distributions (e.g., Medicare: 37% late vs. 16% early, p=0.04). Indications significantly more prevalent in the late ERCP group included abdominal pain (6.6% vs. 0.2%, p=0.03), cholelithiasis (63.6% vs. 53.6%, p=0.04), biliary obstruction (20.5% vs. 3.3%, p=0.02), acute pancreatitis (15% vs. 3.3%, p=0.01), and pancreatic neoplasm (4.5% vs. 0%, p=0.03). Conversely, chronic pancreatitis was significantly more common in the early ERCP group (17.7% vs. 2.4%, p=0.01).
The late ERCP group experienced significantly higher overall mortality (10.9% vs. 0%, p=0.01). A more granular analysis of mortality based on the day of ERCP revealed an increasing trend with delay: mortality was approximately 2-3% for ERCP on Day 1, 15% on Day 2, 2-3% on Days 3-5, rising to approximately 22% on Day 6, and 50% on Day 7. The late ERCP group also had significantly longer stay (18 vs. 4.2 days, p=0.01) and greater total charges ($291,517 vs. $70,307, p=0.01).
Discussion: Patients in the late ERCP group were older, more frequently male, and presented with a higher burden of acute conditions such as biliary obstruction and acute pancreatitis. Late ERCP is associated with worse outcomes including higher mortality that increased with each day of delay, longer hospital stays, and greater total healthcare charges. Conversely, early ERCP was associated with younger patients, a higher prevalence of chronic pancreatitis, and notably better outcomes across all measured parameters.
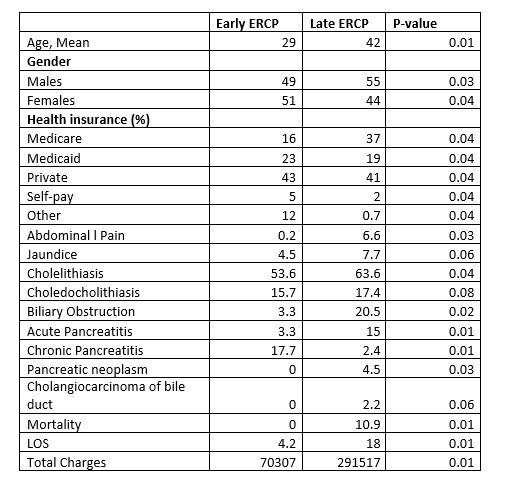
Figure: Comparison of Early Versus Late ERCP
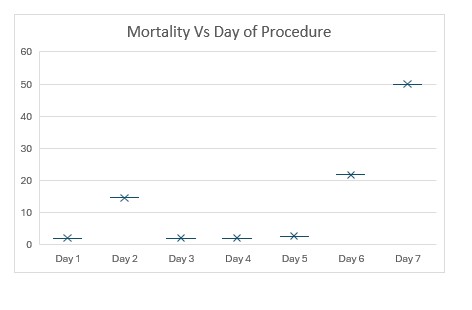
Figure: Day of Procedure of ERCP versus Mortality
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Dinuka Bandara indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Ramandeep Sandhu indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Silpa Choday, MD1, Dinuka Bandara, DO2, Gautam Maddineni, MD3, Osama Abdur Rehman, MD3, Fnu Aakash, MD3, Ramandeep Sandhu, MD1, Indu Srinivasan, MD1. P1374 - Critical Timing of Endoscopic Retrograde Cholangiopancreatography in Acute Cholangitis: Early Procedures Yield Better Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University School of Medicine, Scottsdale, AZ; 3Florida State University, Cape Coral, FL
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is a critical procedure for diagnosing and treating various pancreatobiliary disorders. This study assesses the effect of early vs late ERCP on mortality and readmissions in acute cholangitis.
Methods: We used a National Readmissions Database (2016 -2021) to identify acute cholangitis who underwent therapeutic ERCP within one week of admission. Early ERCP was defined as ERCP performed on the same day of admission or the next day (days 0 or 1, < 48 h), and late ERCP was performed on days 2 to 7 of admission. Multivariate logistic regression was used to calculate the ERCP timing
Results: A total of 330,046 records are analyzed, out of which 38,339 have 30-day readmissions with acute cholangitis. Of these, 53% had early ERCP, while 47% had late ERCP. Patients undergoing early ERCP were significantly younger than those undergoing late ERCP (mean age 29 vs. 42 years, p=0.01). The late ERCP group had a significantly higher proportion of males (55% vs. 49%, p=0.03) and differing health insurance distributions (e.g., Medicare: 37% late vs. 16% early, p=0.04). Indications significantly more prevalent in the late ERCP group included abdominal pain (6.6% vs. 0.2%, p=0.03), cholelithiasis (63.6% vs. 53.6%, p=0.04), biliary obstruction (20.5% vs. 3.3%, p=0.02), acute pancreatitis (15% vs. 3.3%, p=0.01), and pancreatic neoplasm (4.5% vs. 0%, p=0.03). Conversely, chronic pancreatitis was significantly more common in the early ERCP group (17.7% vs. 2.4%, p=0.01).
The late ERCP group experienced significantly higher overall mortality (10.9% vs. 0%, p=0.01). A more granular analysis of mortality based on the day of ERCP revealed an increasing trend with delay: mortality was approximately 2-3% for ERCP on Day 1, 15% on Day 2, 2-3% on Days 3-5, rising to approximately 22% on Day 6, and 50% on Day 7. The late ERCP group also had significantly longer stay (18 vs. 4.2 days, p=0.01) and greater total charges ($291,517 vs. $70,307, p=0.01).
Discussion: Patients in the late ERCP group were older, more frequently male, and presented with a higher burden of acute conditions such as biliary obstruction and acute pancreatitis. Late ERCP is associated with worse outcomes including higher mortality that increased with each day of delay, longer hospital stays, and greater total healthcare charges. Conversely, early ERCP was associated with younger patients, a higher prevalence of chronic pancreatitis, and notably better outcomes across all measured parameters.
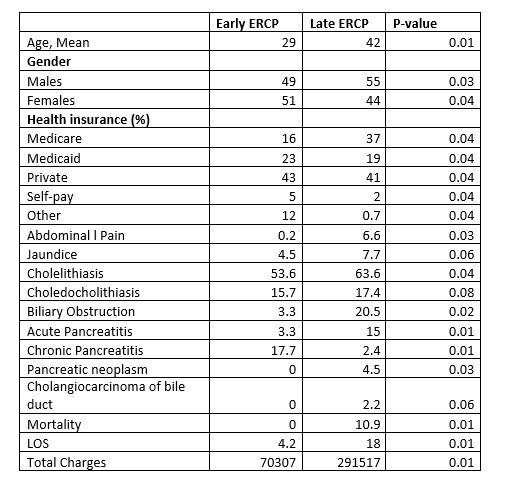
Figure: Comparison of Early Versus Late ERCP
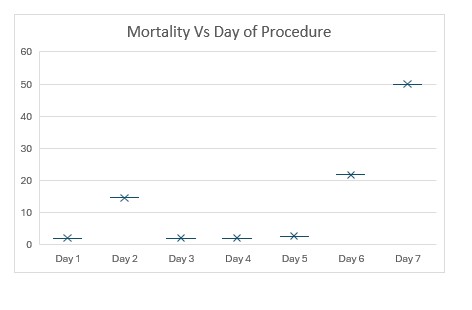
Figure: Day of Procedure of ERCP versus Mortality
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Dinuka Bandara indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Ramandeep Sandhu indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Silpa Choday, MD1, Dinuka Bandara, DO2, Gautam Maddineni, MD3, Osama Abdur Rehman, MD3, Fnu Aakash, MD3, Ramandeep Sandhu, MD1, Indu Srinivasan, MD1. P1374 - Critical Timing of Endoscopic Retrograde Cholangiopancreatography in Acute Cholangitis: Early Procedures Yield Better Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
