Sunday Poster Session
Category: Interventional Endoscopy
P1371 - Cannabis Use Does Not Increase the Risk of Post-Procedural Outcomes in Patients Undergoing ERCP or EUS: A Propensity Score-Matched Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Yassine Kilani, MD
Saint Louis University School of Medicine
Saint Louis, MO
Presenting Author(s)
Yassine Kilani, MD1, Pradeep Yarra, MD1, Priscila Castro Puello, MD2, Shravya R. Ginnaram, MD3, Ahmad Basil Nasir, MD1, Wissam Kiwan, MD1, Alfred Nelson, MD1
1Saint Louis University School of Medicine, Saint Louis, MO; 2Lincoln- Weill Cornell Medical College, Bronx, NY; 3University of Nebraska Medical Center, Omaha, NE
Introduction: Cannabis use is increasingly recognized for its complex effect on gastrointestinal function and inflammation. Despite the rising prevalence of cannabis use among patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) or endoscopic ultrasound (EUS), there is a lack of clinical studies evaluation its impact on post- procedural complications including post-ERCP pancreatitis, remains poorly understood. This study aims to address this knowledge gap by evaluating the incidence of post procedural complications in patients using cannabis compared to those non-users.
Methods: We conducted a retrospective cohort study in the United States using the TriNetX database to identify adults (≥18 years) undergoing ERCP or EUS and using cannabis. This cohort was matched with patients undergoing ERCP and not using cannabis using 1:1 propensity score matching. The primary outcome was the incidence of post-ERCP pancreatitis within 10 days after ERCP. Secondary outcomes were emergency intubation, aspiration pneumonia, and perforation. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
Results: A total of 6564 patients undergoing ERCP and using cannabis were identified and propensity matched with 343,542 non-users undergoing ERCP or EUS, resulting in 6525 matched pairs. Patients treated with cannabis were younger, and had higher rates of cholecystitis, cholelithiasis, and cholangitis (p < 0.001) as compared to controls (Table 1). After matching, patients undergoing ERCP or EUS and using cannabis had no significant differences in the risk of post-ERCP pancreatitis (1.2% vs. 1.5%; adjusted hazard ratio (aHR) = 0.77, 95% CI: 0.53–1.10), without significant differences in aspiration pneumonia (aHR = 1.19, 95% CI: 0.68–2.07), emergency intubations (aHR = 1.16, 95% CI: 0.42–3.19), and gastrointestinal perforations (aHR = 0.86, 95% CI: 0.29–2.55) at 10 days follow-up (Table 2).
Discussion: Our findings provide real-world evidence that cannabis use in patients undergoing ERCP or EUS does not significantly increase or reduce the risk of post-ERCP pancreatitis compared to non-users. These results suggest that cannabis use may not be an independent risk factor for other post-procedural complications, though further prospective studies are needed to clarify its role in outcomes and potential interactions with patient risk profiles
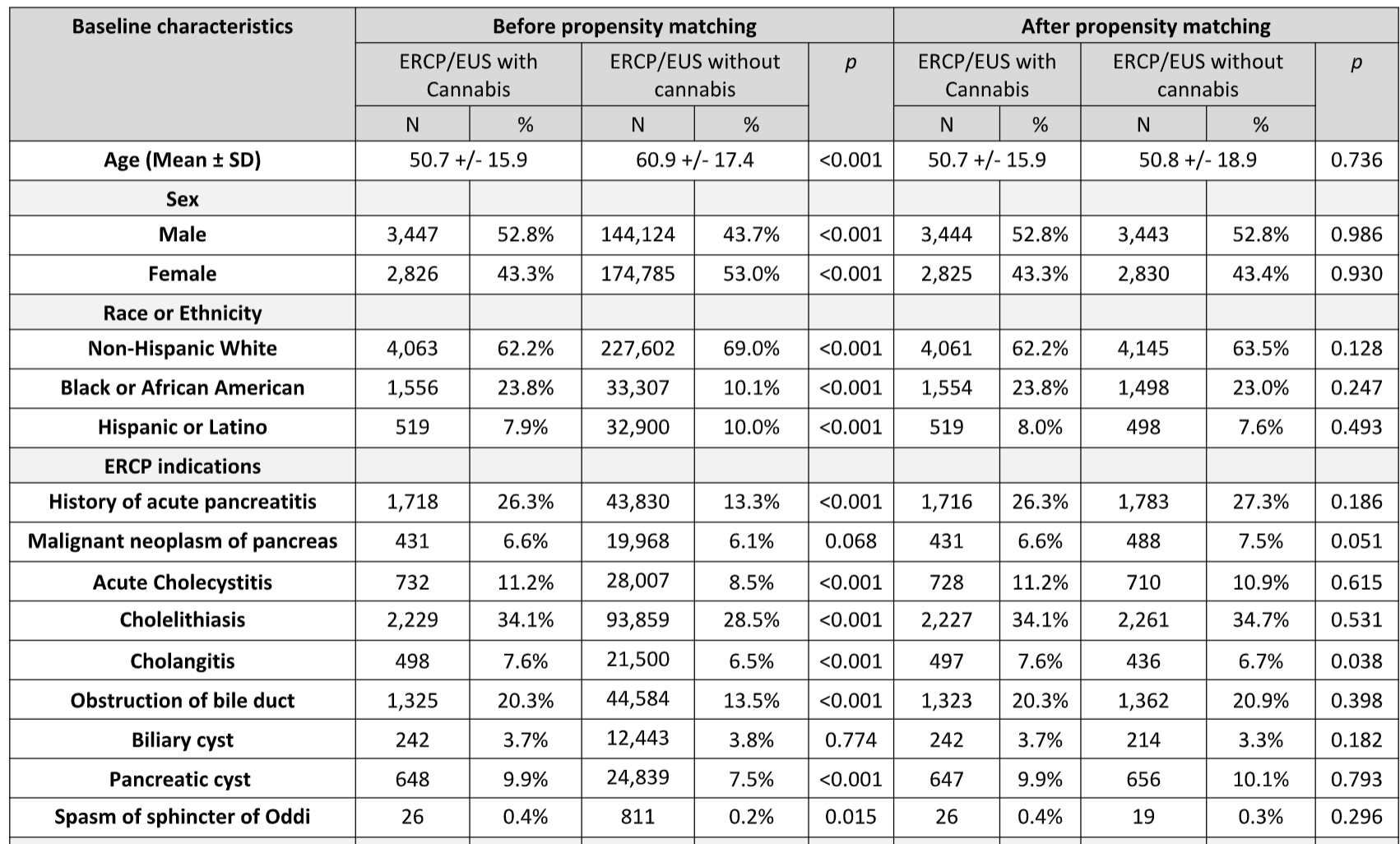
Figure: Baseline Characteristics
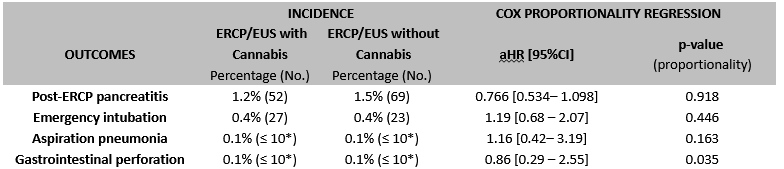
Figure: Post procedural complications; * To protect patient privacy, the TriNetX Analytics platform rounds up incidences ≤ 10 cases, displaying them as “≤ 10”.
Disclosures:
Yassine Kilani indicated no relevant financial relationships.
Pradeep Yarra indicated no relevant financial relationships.
Priscila Castro Puello indicated no relevant financial relationships.
Shravya Ginnaram indicated no relevant financial relationships.
Ahmad Basil Nasir indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Alfred Nelson indicated no relevant financial relationships.
Yassine Kilani, MD1, Pradeep Yarra, MD1, Priscila Castro Puello, MD2, Shravya R. Ginnaram, MD3, Ahmad Basil Nasir, MD1, Wissam Kiwan, MD1, Alfred Nelson, MD1. P1371 - Cannabis Use Does Not Increase the Risk of Post-Procedural Outcomes in Patients Undergoing ERCP or EUS: A Propensity Score-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Louis University School of Medicine, Saint Louis, MO; 2Lincoln- Weill Cornell Medical College, Bronx, NY; 3University of Nebraska Medical Center, Omaha, NE
Introduction: Cannabis use is increasingly recognized for its complex effect on gastrointestinal function and inflammation. Despite the rising prevalence of cannabis use among patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) or endoscopic ultrasound (EUS), there is a lack of clinical studies evaluation its impact on post- procedural complications including post-ERCP pancreatitis, remains poorly understood. This study aims to address this knowledge gap by evaluating the incidence of post procedural complications in patients using cannabis compared to those non-users.
Methods: We conducted a retrospective cohort study in the United States using the TriNetX database to identify adults (≥18 years) undergoing ERCP or EUS and using cannabis. This cohort was matched with patients undergoing ERCP and not using cannabis using 1:1 propensity score matching. The primary outcome was the incidence of post-ERCP pancreatitis within 10 days after ERCP. Secondary outcomes were emergency intubation, aspiration pneumonia, and perforation. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
Results: A total of 6564 patients undergoing ERCP and using cannabis were identified and propensity matched with 343,542 non-users undergoing ERCP or EUS, resulting in 6525 matched pairs. Patients treated with cannabis were younger, and had higher rates of cholecystitis, cholelithiasis, and cholangitis (p < 0.001) as compared to controls (Table 1). After matching, patients undergoing ERCP or EUS and using cannabis had no significant differences in the risk of post-ERCP pancreatitis (1.2% vs. 1.5%; adjusted hazard ratio (aHR) = 0.77, 95% CI: 0.53–1.10), without significant differences in aspiration pneumonia (aHR = 1.19, 95% CI: 0.68–2.07), emergency intubations (aHR = 1.16, 95% CI: 0.42–3.19), and gastrointestinal perforations (aHR = 0.86, 95% CI: 0.29–2.55) at 10 days follow-up (Table 2).
Discussion: Our findings provide real-world evidence that cannabis use in patients undergoing ERCP or EUS does not significantly increase or reduce the risk of post-ERCP pancreatitis compared to non-users. These results suggest that cannabis use may not be an independent risk factor for other post-procedural complications, though further prospective studies are needed to clarify its role in outcomes and potential interactions with patient risk profiles
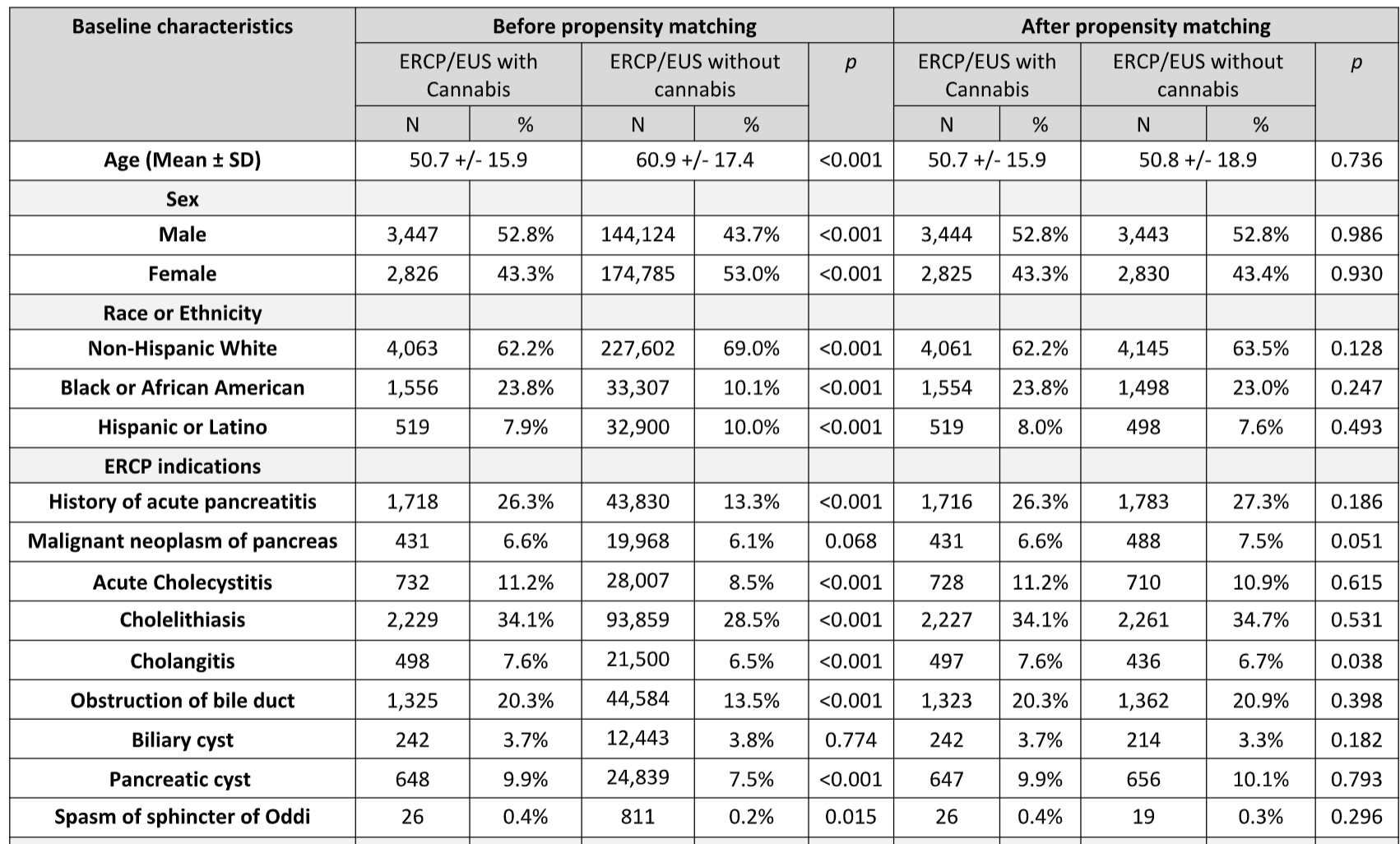
Figure: Baseline Characteristics
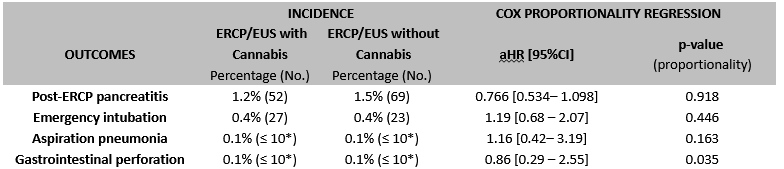
Figure: Post procedural complications; * To protect patient privacy, the TriNetX Analytics platform rounds up incidences ≤ 10 cases, displaying them as “≤ 10”.
Disclosures:
Yassine Kilani indicated no relevant financial relationships.
Pradeep Yarra indicated no relevant financial relationships.
Priscila Castro Puello indicated no relevant financial relationships.
Shravya Ginnaram indicated no relevant financial relationships.
Ahmad Basil Nasir indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Alfred Nelson indicated no relevant financial relationships.
Yassine Kilani, MD1, Pradeep Yarra, MD1, Priscila Castro Puello, MD2, Shravya R. Ginnaram, MD3, Ahmad Basil Nasir, MD1, Wissam Kiwan, MD1, Alfred Nelson, MD1. P1371 - Cannabis Use Does Not Increase the Risk of Post-Procedural Outcomes in Patients Undergoing ERCP or EUS: A Propensity Score-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
