Sunday Poster Session
Category: Infections and Microbiome
Breaking Down the Abscess: <i>Nocardia farcinica</i> Behind an Abdominal Mystery
P1355 - Breaking Down the Abscess: Nocardia farcinica Behind an Abdominal Mystery
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Catherine Loehr, MD (she/her/hers)
Louisiana State University
New Orleans, LA
Presenting Author(s)
Catherine Loehr, MD1, Erika Haviland, DO2, Jeffery Anderson, MD2, Christopher Hayden, MD2, Allen Byl, DO2, Leandre Millet, MD2, Mathoula Bilalis, MD3, Benjamin Guider, MD3
1Louisiana State University, New Orleans, LA; 2LSU Health New Orleans, New Orleans, LA; 3Tulane Medical Center, New Orleans, LA
Introduction: Nocardia farcinica is a gram-positive, aerobic, filamentous bacteria. According to the NIH there are only 50-100 cases of Nocardia per year. N. farcinica is distinct from other Nocardia species by its high degree of antibiotic resistance and virulence, particularly in predisposing conditions. Nocardia spp. usually causes primary pulmonary infections, but it can cause infections in other sites resulting from hematogenous dissemination. The central nervous system is the second most frequently involved, but it can lead to rare infections in the abdomen, cornea, heart, joints and bones. Nocardia can lead to significant morbidity, particularly if disseminated and immunosuppressed. This case presents a 39-year-old male with a complex medical history who developed nocardiosis identified in an intrabdominal wall abscess.
Case Description/
Methods: A 39-year-old incarcerated male with large-vessel arteritis (inconsistently on prednisone and methotrexate leading to a complicated vascular history now on rivaroxaban), multiple DVT’s requiring an IVC filter, pyoderma gangrenosum and chronic mesenteric ischemia presented to the ED for two months of hematochezia, 70-lb weight loss, hand rashes with abdominal and leg pain. CT of chest/abdomen found a 1.2 cm nodular area with cavitation in the right middle lobe, development of a complicated left transversalis intramuscular fluid collection, complete occlusion of SMA and other vascular changes. He was started on vancomycin and piperacillin/tazobactam. He underwent abdominal fluid drainage which expressed purulent drainage. The culture had no growth until day 9, resulting positive for N. farcinica. MRI brain showed multifocal enhancing lesions. He was then changed to imipenem-cilastatin and trimethoprim/sulfamethoxazole; however, resistances returned to imipenem-cilastatin and switched to linezolid. He subsequently underwent a native vein SMA bypass. He clinically improved slowly overtime. Discharge plan included IV antibiotics for 6 weeks then switch to PO for one year.
Discussion: This case highlights the complexity of diagnosing and managing nocardial infections in immunocompromised patients. The delayed identification of N. farcinica emphasizes the importance of considering atypical pathogens when standard antimicrobial regimens fail. Targeted antibiotic therapy with surgical intervention led to the patient's clinical improvement. This case demonstrates the necessity for multidisciplinary care in managing complex infections in immunocompromised patients.
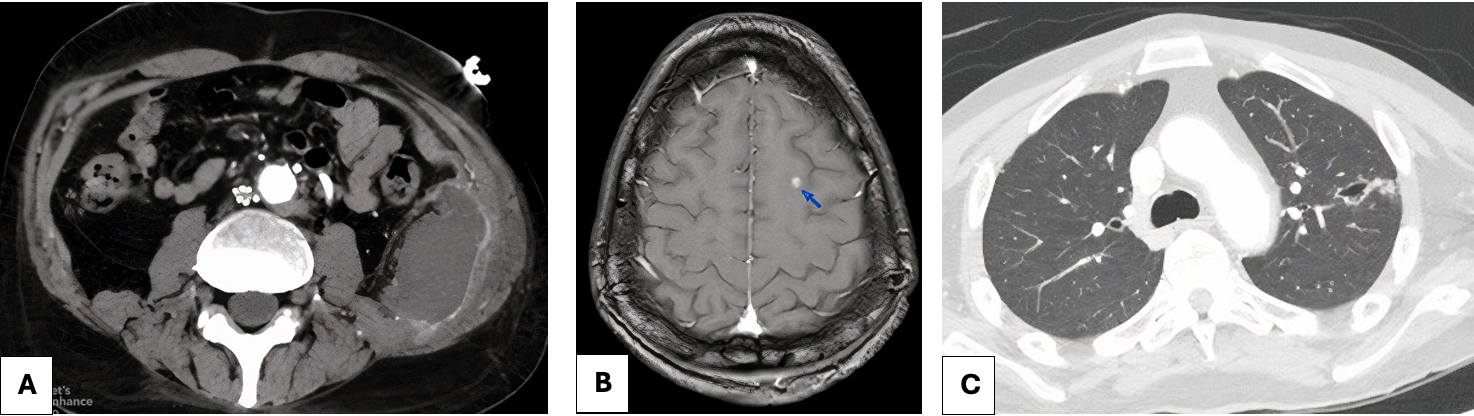
Figure: Figure 1. A) Contrast enhanced CT of the abdomen demonstrating a left transversalis fluid collection. The average Hounsfield unit of this collection is approximately 25 units, higher than expected for a simple collection. B) T1 post-contrast MRI brain demonstrating a left superior frontal gyrus, contrast-enhancing lesion with associated vasogenic edema and diffusion restriction. C) Contrast enhanced CT of the chest demonstrating a right middle lobe cavitating nodule.
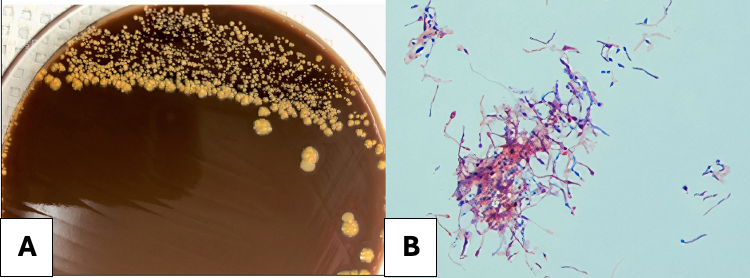
Figure: Figure 2. A) Colonial characteristics of N. farcinica on blood agar plates include pale yellow pigmentation, elevated growth, a rough surface, and opacity. B) Gram staining of N. farcinica revealed Gram-positive bacteria characterized by rod-shaped morphology and visible branches.
Disclosures:
Catherine Loehr indicated no relevant financial relationships.
Erika Haviland indicated no relevant financial relationships.
Jeffery Anderson indicated no relevant financial relationships.
Christopher Hayden indicated no relevant financial relationships.
Allen Byl indicated no relevant financial relationships.
Leandre Millet indicated no relevant financial relationships.
Mathoula Bilalis indicated no relevant financial relationships.
Benjamin Guider indicated no relevant financial relationships.
Catherine Loehr, MD1, Erika Haviland, DO2, Jeffery Anderson, MD2, Christopher Hayden, MD2, Allen Byl, DO2, Leandre Millet, MD2, Mathoula Bilalis, MD3, Benjamin Guider, MD3. P1355 - Breaking Down the Abscess: <i>Nocardia farcinica</i> Behind an Abdominal Mystery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Louisiana State University, New Orleans, LA; 2LSU Health New Orleans, New Orleans, LA; 3Tulane Medical Center, New Orleans, LA
Introduction: Nocardia farcinica is a gram-positive, aerobic, filamentous bacteria. According to the NIH there are only 50-100 cases of Nocardia per year. N. farcinica is distinct from other Nocardia species by its high degree of antibiotic resistance and virulence, particularly in predisposing conditions. Nocardia spp. usually causes primary pulmonary infections, but it can cause infections in other sites resulting from hematogenous dissemination. The central nervous system is the second most frequently involved, but it can lead to rare infections in the abdomen, cornea, heart, joints and bones. Nocardia can lead to significant morbidity, particularly if disseminated and immunosuppressed. This case presents a 39-year-old male with a complex medical history who developed nocardiosis identified in an intrabdominal wall abscess.
Case Description/
Methods: A 39-year-old incarcerated male with large-vessel arteritis (inconsistently on prednisone and methotrexate leading to a complicated vascular history now on rivaroxaban), multiple DVT’s requiring an IVC filter, pyoderma gangrenosum and chronic mesenteric ischemia presented to the ED for two months of hematochezia, 70-lb weight loss, hand rashes with abdominal and leg pain. CT of chest/abdomen found a 1.2 cm nodular area with cavitation in the right middle lobe, development of a complicated left transversalis intramuscular fluid collection, complete occlusion of SMA and other vascular changes. He was started on vancomycin and piperacillin/tazobactam. He underwent abdominal fluid drainage which expressed purulent drainage. The culture had no growth until day 9, resulting positive for N. farcinica. MRI brain showed multifocal enhancing lesions. He was then changed to imipenem-cilastatin and trimethoprim/sulfamethoxazole; however, resistances returned to imipenem-cilastatin and switched to linezolid. He subsequently underwent a native vein SMA bypass. He clinically improved slowly overtime. Discharge plan included IV antibiotics for 6 weeks then switch to PO for one year.
Discussion: This case highlights the complexity of diagnosing and managing nocardial infections in immunocompromised patients. The delayed identification of N. farcinica emphasizes the importance of considering atypical pathogens when standard antimicrobial regimens fail. Targeted antibiotic therapy with surgical intervention led to the patient's clinical improvement. This case demonstrates the necessity for multidisciplinary care in managing complex infections in immunocompromised patients.
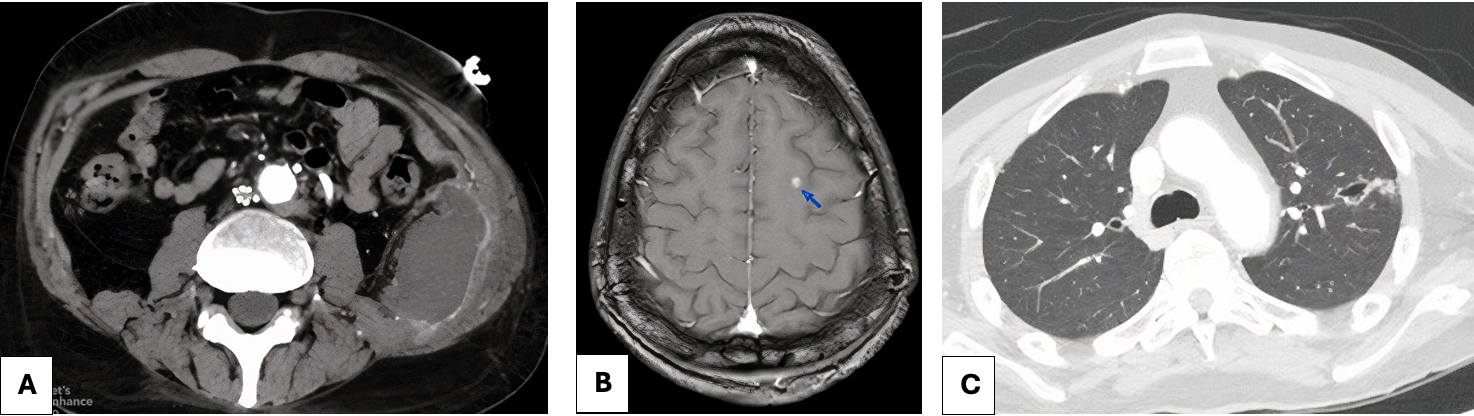
Figure: Figure 1. A) Contrast enhanced CT of the abdomen demonstrating a left transversalis fluid collection. The average Hounsfield unit of this collection is approximately 25 units, higher than expected for a simple collection. B) T1 post-contrast MRI brain demonstrating a left superior frontal gyrus, contrast-enhancing lesion with associated vasogenic edema and diffusion restriction. C) Contrast enhanced CT of the chest demonstrating a right middle lobe cavitating nodule.
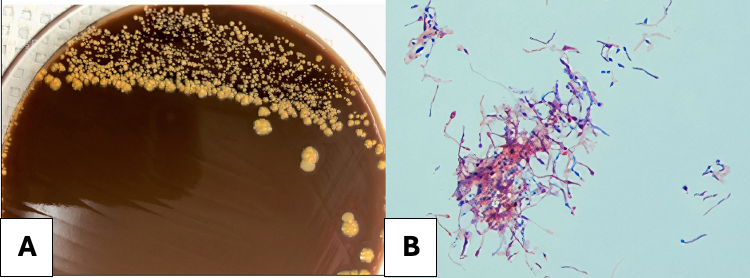
Figure: Figure 2. A) Colonial characteristics of N. farcinica on blood agar plates include pale yellow pigmentation, elevated growth, a rough surface, and opacity. B) Gram staining of N. farcinica revealed Gram-positive bacteria characterized by rod-shaped morphology and visible branches.
Disclosures:
Catherine Loehr indicated no relevant financial relationships.
Erika Haviland indicated no relevant financial relationships.
Jeffery Anderson indicated no relevant financial relationships.
Christopher Hayden indicated no relevant financial relationships.
Allen Byl indicated no relevant financial relationships.
Leandre Millet indicated no relevant financial relationships.
Mathoula Bilalis indicated no relevant financial relationships.
Benjamin Guider indicated no relevant financial relationships.
Catherine Loehr, MD1, Erika Haviland, DO2, Jeffery Anderson, MD2, Christopher Hayden, MD2, Allen Byl, DO2, Leandre Millet, MD2, Mathoula Bilalis, MD3, Benjamin Guider, MD3. P1355 - Breaking Down the Abscess: <i>Nocardia farcinica</i> Behind an Abdominal Mystery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
