Sunday Poster Session
Category: Infections and Microbiome
P1349 - Evolving Diagnosis in Persistent Diarrhea: The Critical Role of Ongoing Re-Evaluation in Identifying Infectious Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Griffin Sansbury, BS (he/him/his)
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Griffin Sansbury, BS1, William McGonigle, BS1, Myra Quiroga, MD2, Grigoriy Rapoport, MD3
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 3University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: In patients presenting with subacute diarrhea, infectious and inflammatory causes are commonly considered. When clinical features are unclear, infectious workup is typically prioritized - particularly testing for Clostridioides difficile (C. diff) in hospitalized patients or those with recent antibiotic exposure. This distinction is crucial, as initiating immunosuppressive therapy for presumed inflammatory diarrhea may exacerbate undiagnosed infections and worsen outcomes.
Case Description/
Methods: We present an 80-year-old female with a history of diverticulitis and suspected segmental colitis associated with diverticulosis (SCAD) who presented with one day of acute non-bloody diarrhea, reporting 20 episodes with abdominal pain, fever and chills. She endorsed six months of chronic, mild diarrhea previously attributed to SCAD based on endoscopic findings and unresponsive to antibiotics two weeks prior.
Initial labs showed marked leukocytosis (WBC 27.9K) and elevated CRP (10.6 mg/dL). Abdominal CT revealed new pancolitis. Empiric intravenous vancomycin and cefepime were started. An enteric pathogen panel, including PCR for C. diff toxin genes, was negative and enzyme immunoassay (EIA) testing was not reflexed. Given these findings, SCAD versus new-onset inflammatory bowel disease was considered and mesalamine was initiated.
Colonoscopy revealed rectosigmoid nodular plaques and punctate mucosal nodules. Biopsies demonstrated active colitis with ulcerative exudates. Intravenous steroids were started for presumed inflammatory colitis. However, her symptoms persisted and leukocytosis worsened, peaking at 46.8K. Surgery was consulted to evaluate for possible laparoscopic sigmoidectomy versus total colectomy. Given ongoing clinical decline and endoscopic findings, repeat stool studies were sent, which resulted positive for C. diff toxin B by PCR with a positive reflex EIA. Steroids and mesalamine were promptly discontinued and oral vancomycin was initiated. The patient demonstrated marked clinical improvement and normalization of WBC.
Discussion: This case highlights the diagnostic challenge of distinguishing inflammatory from infectious colitis, particularly in patients with chronic symptoms and known colonic pathology. Early, accurate identification of C. diff is critical, as misdiagnosis can lead to inappropriate immunosuppression and clinical deterioration. This case underscores the importance of considering C. diff retesting if clinical suspicion remains high and the patient is not improving.
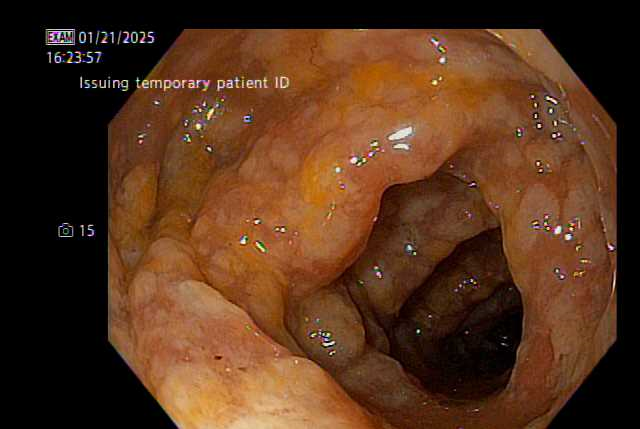
Figure: Figure 1: Diffuse congested, granular, nodular mucosa in the sigmoid colon.

Figure: Figure 2: White plaques and punctate nodules in the sigmoid colon.
Disclosures:
Griffin Sansbury indicated no relevant financial relationships.
William McGonigle indicated no relevant financial relationships.
Myra Quiroga indicated no relevant financial relationships.
Grigoriy Rapoport indicated no relevant financial relationships.
Griffin Sansbury, BS1, William McGonigle, BS1, Myra Quiroga, MD2, Grigoriy Rapoport, MD3. P1349 - Evolving Diagnosis in Persistent Diarrhea: The Critical Role of Ongoing Re-Evaluation in Identifying Infectious Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 3University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: In patients presenting with subacute diarrhea, infectious and inflammatory causes are commonly considered. When clinical features are unclear, infectious workup is typically prioritized - particularly testing for Clostridioides difficile (C. diff) in hospitalized patients or those with recent antibiotic exposure. This distinction is crucial, as initiating immunosuppressive therapy for presumed inflammatory diarrhea may exacerbate undiagnosed infections and worsen outcomes.
Case Description/
Methods: We present an 80-year-old female with a history of diverticulitis and suspected segmental colitis associated with diverticulosis (SCAD) who presented with one day of acute non-bloody diarrhea, reporting 20 episodes with abdominal pain, fever and chills. She endorsed six months of chronic, mild diarrhea previously attributed to SCAD based on endoscopic findings and unresponsive to antibiotics two weeks prior.
Initial labs showed marked leukocytosis (WBC 27.9K) and elevated CRP (10.6 mg/dL). Abdominal CT revealed new pancolitis. Empiric intravenous vancomycin and cefepime were started. An enteric pathogen panel, including PCR for C. diff toxin genes, was negative and enzyme immunoassay (EIA) testing was not reflexed. Given these findings, SCAD versus new-onset inflammatory bowel disease was considered and mesalamine was initiated.
Colonoscopy revealed rectosigmoid nodular plaques and punctate mucosal nodules. Biopsies demonstrated active colitis with ulcerative exudates. Intravenous steroids were started for presumed inflammatory colitis. However, her symptoms persisted and leukocytosis worsened, peaking at 46.8K. Surgery was consulted to evaluate for possible laparoscopic sigmoidectomy versus total colectomy. Given ongoing clinical decline and endoscopic findings, repeat stool studies were sent, which resulted positive for C. diff toxin B by PCR with a positive reflex EIA. Steroids and mesalamine were promptly discontinued and oral vancomycin was initiated. The patient demonstrated marked clinical improvement and normalization of WBC.
Discussion: This case highlights the diagnostic challenge of distinguishing inflammatory from infectious colitis, particularly in patients with chronic symptoms and known colonic pathology. Early, accurate identification of C. diff is critical, as misdiagnosis can lead to inappropriate immunosuppression and clinical deterioration. This case underscores the importance of considering C. diff retesting if clinical suspicion remains high and the patient is not improving.
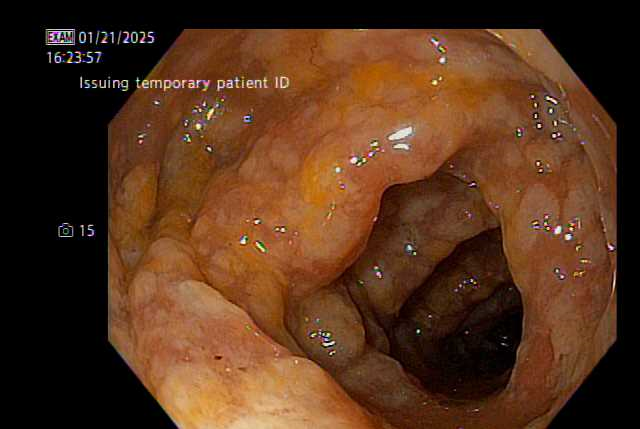
Figure: Figure 1: Diffuse congested, granular, nodular mucosa in the sigmoid colon.

Figure: Figure 2: White plaques and punctate nodules in the sigmoid colon.
Disclosures:
Griffin Sansbury indicated no relevant financial relationships.
William McGonigle indicated no relevant financial relationships.
Myra Quiroga indicated no relevant financial relationships.
Grigoriy Rapoport indicated no relevant financial relationships.
Griffin Sansbury, BS1, William McGonigle, BS1, Myra Quiroga, MD2, Grigoriy Rapoport, MD3. P1349 - Evolving Diagnosis in Persistent Diarrhea: The Critical Role of Ongoing Re-Evaluation in Identifying Infectious Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
