Sunday Poster Session
Category: Infections and Microbiome
When a Stomach Bug Stirs the Blood: A Case of <i>H. pylori</i> Induced Hypereosinophilic Syndrome
P1348 - When a Stomach Bug Stirs the Blood: A Case of H. pylori Induced Hypereosinophilic Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ashley Serjilus, MD (she/her/hers)
Naval Medical Center Portsmouth
Portsmouth, VA
Presenting Author(s)
Ashley Serjilus, MD, Rachel Dennis, DO, John Mattingly, MD, Michael Burns, DO
Naval Medical Center Portsmouth, Portsmouth, VA
Introduction: Hypereosinophilia is defined as an absolute eosinophil count (AEC) >1500 cells/μL. Hypereosinophilic syndromes (HES) are a group of disorders characterized by persistent eosinophilia, leading to eosinophil-related organ damage. Common causes include parasitic infections, drug hypersensitivity, allergic reactions, and hematologic malignancies. While Helicobacter pylori (H. pylori) is usually associated with gastritis and peptic ulcers, its connection to systemic inflammation is not widely acknowledged. We present a case of HES linked to H. pylori, resulting in extensive gastrointestinal (GI) symptoms and eosinophilia, which resolved after treatment.
Case Description/
Methods: A 25-year-old male presented with epigastric pain, nausea, vomiting, fever, diarrhea, and dyspnea. Labs revealed WBC 24.7 K/μL with AEC 14.5 K/μL, CRP 11.2 mg/dL, and ESR 45 mm/hr. Computed tomography (CT) imaging demonstrated diffuse GI tract inflammation, small bowel wall thickening, moderate ascites, and a small right pleural effusion. Infectious workup, including stool studies and serologies, was negative for parasites and viruses. Esophagogastroduodenoscopy (EGD) showed moderate chronic gastritis with biopsy-confirmed H. pylori. Duodenal biopsies had increased intraepithelial lymphocytes but minimal eosinophilic infiltration; colon biopsies revealed mild colitis with scattered eosinophils. Bone marrow biopsy and flow cytometry were unremarkable, and FIP1L1-PDGFRA testing was negative, ruling out myeloproliferative variants of HES. The patient was diagnosed with secondary hypereosinophilia related to H. pylori infection. He was started on quadruple therapy and oral prednisone. At the one-month follow-up, AEC decreased to 420 cells/μL, CRP levels 3.2 mg/dL, and ESR 12 mm/hr. Symptom resolution persisted over the next 10 months.
Discussion: This case highlights a rare instance of HES with significant GI involvement, likely triggered by an H. pylori infection, with only one other similar case documented. The timing of symptoms and their resolution after treatment suggest a causal link. While the exact mechanisms remain unclear, H. pylori may induce eosinophilia through cytokine pathways, particularly interleukin-5. The findings of mild tissue eosinophilia and significant peripheral eosinophilia point to a systemic issue, rather than localized eosinophilic gastroenteritis. This case broadens the differential diagnosis for secondary hypereosinophilia and highlights the potential for atypical presentations of common pathogens.
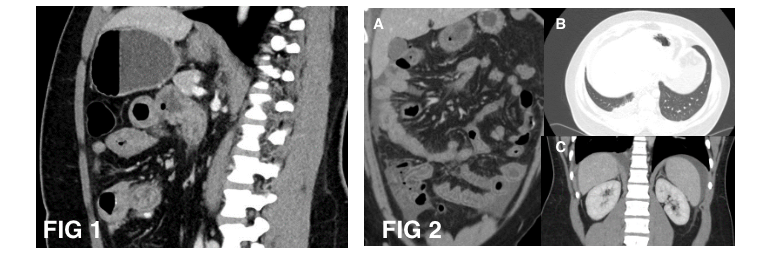
Figure: FIG 1: Long segment of small bowel wall edema and thickening with adjacent stranding and vascular engorgement on CT scan.
FIG 2: Diffuse small and large bowel inflammation with moderate volume ascites (A,C) and small right pleural effusion (B).
Disclosures:
Ashley Serjilus indicated no relevant financial relationships.
Rachel Dennis indicated no relevant financial relationships.
John Mattingly: fulgent genetics – Stock-publicly held company(excluding mutual/index funds). gilead sciences – Stock-publicly held company(excluding mutual/index funds). illumina inc – Stock-publicly held company(excluding mutual/index funds). natera incorporated – Stock-publicly held company(excluding mutual/index funds). neurocrine biosciences – Stock-publicly held company(excluding mutual/index funds).
Michael Burns indicated no relevant financial relationships.
Ashley Serjilus, MD, Rachel Dennis, DO, John Mattingly, MD, Michael Burns, DO. P1348 - When a Stomach Bug Stirs the Blood: A Case of <i>H. pylori</i> Induced Hypereosinophilic Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Naval Medical Center Portsmouth, Portsmouth, VA
Introduction: Hypereosinophilia is defined as an absolute eosinophil count (AEC) >1500 cells/μL. Hypereosinophilic syndromes (HES) are a group of disorders characterized by persistent eosinophilia, leading to eosinophil-related organ damage. Common causes include parasitic infections, drug hypersensitivity, allergic reactions, and hematologic malignancies. While Helicobacter pylori (H. pylori) is usually associated with gastritis and peptic ulcers, its connection to systemic inflammation is not widely acknowledged. We present a case of HES linked to H. pylori, resulting in extensive gastrointestinal (GI) symptoms and eosinophilia, which resolved after treatment.
Case Description/
Methods: A 25-year-old male presented with epigastric pain, nausea, vomiting, fever, diarrhea, and dyspnea. Labs revealed WBC 24.7 K/μL with AEC 14.5 K/μL, CRP 11.2 mg/dL, and ESR 45 mm/hr. Computed tomography (CT) imaging demonstrated diffuse GI tract inflammation, small bowel wall thickening, moderate ascites, and a small right pleural effusion. Infectious workup, including stool studies and serologies, was negative for parasites and viruses. Esophagogastroduodenoscopy (EGD) showed moderate chronic gastritis with biopsy-confirmed H. pylori. Duodenal biopsies had increased intraepithelial lymphocytes but minimal eosinophilic infiltration; colon biopsies revealed mild colitis with scattered eosinophils. Bone marrow biopsy and flow cytometry were unremarkable, and FIP1L1-PDGFRA testing was negative, ruling out myeloproliferative variants of HES. The patient was diagnosed with secondary hypereosinophilia related to H. pylori infection. He was started on quadruple therapy and oral prednisone. At the one-month follow-up, AEC decreased to 420 cells/μL, CRP levels 3.2 mg/dL, and ESR 12 mm/hr. Symptom resolution persisted over the next 10 months.
Discussion: This case highlights a rare instance of HES with significant GI involvement, likely triggered by an H. pylori infection, with only one other similar case documented. The timing of symptoms and their resolution after treatment suggest a causal link. While the exact mechanisms remain unclear, H. pylori may induce eosinophilia through cytokine pathways, particularly interleukin-5. The findings of mild tissue eosinophilia and significant peripheral eosinophilia point to a systemic issue, rather than localized eosinophilic gastroenteritis. This case broadens the differential diagnosis for secondary hypereosinophilia and highlights the potential for atypical presentations of common pathogens.
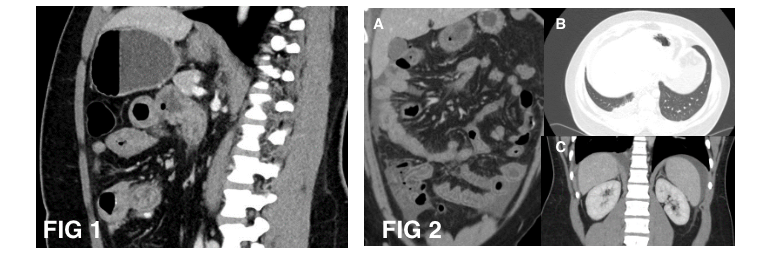
Figure: FIG 1: Long segment of small bowel wall edema and thickening with adjacent stranding and vascular engorgement on CT scan.
FIG 2: Diffuse small and large bowel inflammation with moderate volume ascites (A,C) and small right pleural effusion (B).
Disclosures:
Ashley Serjilus indicated no relevant financial relationships.
Rachel Dennis indicated no relevant financial relationships.
John Mattingly: fulgent genetics – Stock-publicly held company(excluding mutual/index funds). gilead sciences – Stock-publicly held company(excluding mutual/index funds). illumina inc – Stock-publicly held company(excluding mutual/index funds). natera incorporated – Stock-publicly held company(excluding mutual/index funds). neurocrine biosciences – Stock-publicly held company(excluding mutual/index funds).
Michael Burns indicated no relevant financial relationships.
Ashley Serjilus, MD, Rachel Dennis, DO, John Mattingly, MD, Michael Burns, DO. P1348 - When a Stomach Bug Stirs the Blood: A Case of <i>H. pylori</i> Induced Hypereosinophilic Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
