Sunday Poster Session
Category: Infections and Microbiome
A Fatal Case of Suspected <i>Clostridioides difficile</i> in a Patient with Native Anatomy
P1338 - A Fatal Case of Suspected Clostridioides difficile in a Patient with Native Anatomy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Samantha Woller, MD, MS
Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Samantha Woller, MD, MS1, Clive Miranda, DO1, Eva Holland, 2, Fnu Monika, MBBS3, Wuttiporn Manatsathit, MD1
1Creighton University Medical Center, Omaha, NE; 2Creighton University School of Medicine, Omaha, NE; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Clostridioides difficile (C. diff) is a well-known cause of colitis but involvement of the small intestine, referred to as C. diff enteritis, is exceedingly rare. C. diff enteritis is usually reported in patients with prior colectomy due to loss of the ileocecal valve. We present a fatal case of suspected C. diff enteritis in a patient with intact colonic anatomy.
Case Description/
Methods: A 39-year-old female with a history of systemic lupus erythematosus (SLE) and chronic pancytopenia presented with several days of pain, nausea, vomiting, and diarrhea. Imaging revealed jejunal and mesenteric edema consistent with enteritis. Labs revealed chronic pancytopenia and mildly elevated inflammatory markers. Initial differentials included medication toxicity, SLE flare, and infection.
Esophagogastroduodenoscopy (EGD) was unrevealing. A gastrointestinal pathogen panel was positive for C. diff and oral vancomycin was started. Despite treatment, symptoms persisted. Repeat imaging showed progressive small bowel thickening and ascites, without colonic involvement. Given the isolated findings, lupus enteritis (LE), intestinal angioedema, or mastocytosis. High-dose intravenous steroids were initiated but soon de-escalated by rheumatology due to unremarkable lupus markers. The patient acutely decompensated with peritonitis and underwent emergent laparotomy with small bowel resection. Pathology showed pseudomembranous enteritis and acute serositis. No viral or vasculitis etiology was identified. Despite further intervention, the patient continued to decline and was transitioned to comfort care.
Discussion: This case represents a rare and fatal presentation of presumed C. diff enteritis in a patient without prior colectomy. While both stool pathogen testing and histology were consistent with C. diff infection, definitive causality could not be confirmed. Other autoimmune etiologies were thought to be less likely. C. diff enteritis has primarily been reported with patients post-colectomy; this patient’s intact colon raises questions about factors that may have predisposed her to isolated small bowel involvement. It also highlights the association of the hypervirulent BI/NAP1/027 strain with enteritis. Strain typing may have clarified the etiology, but was unavailable. This case highlights the need for clinical awareness of atypical C. diff presentations, especially in immunocompromised patients, and underscores the importance of further research into diagnostic criteria and risk factors for enteric involvement.
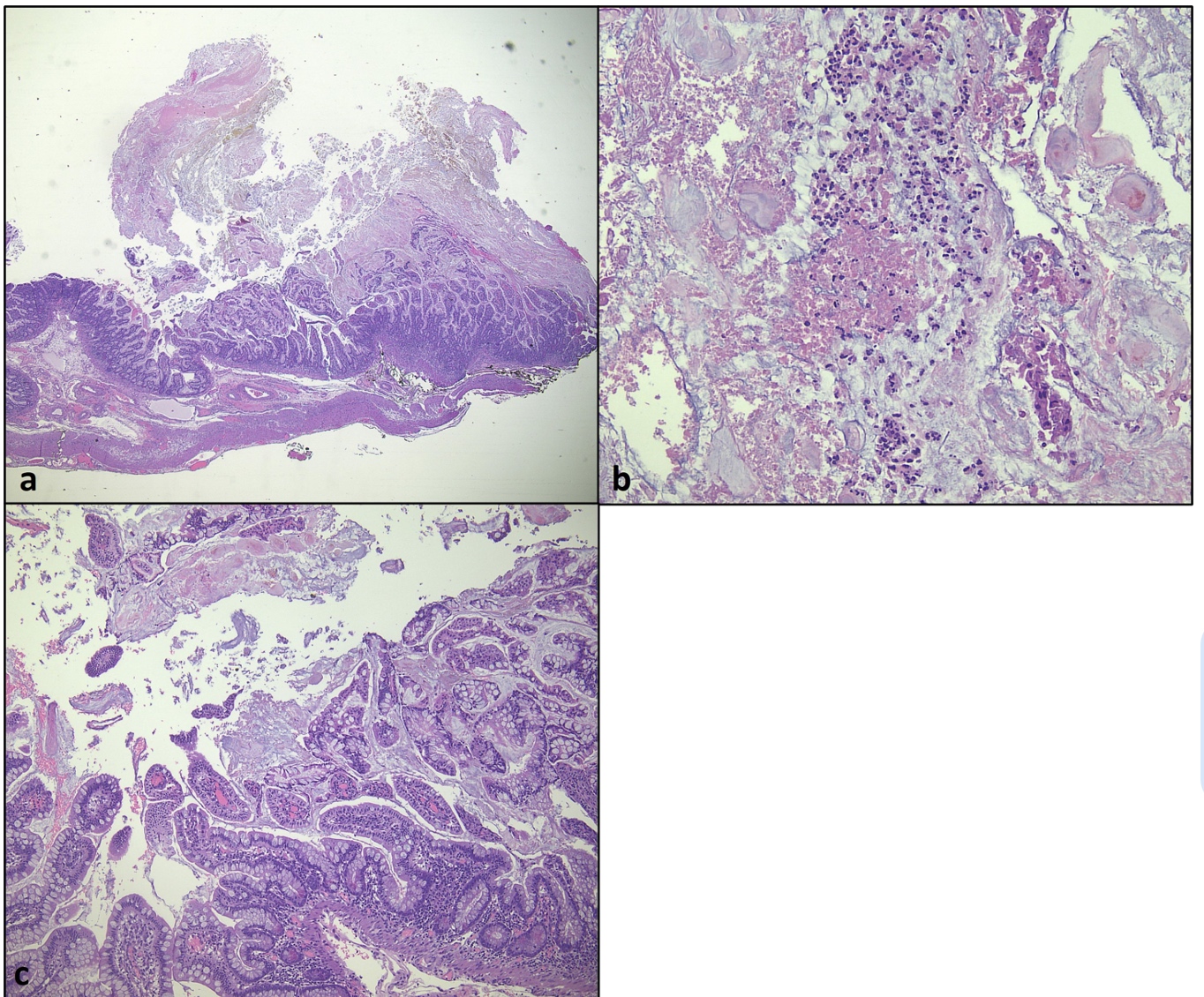
Figure: Figure 1. Pseudomembranous colitis. (a) At low power (2x), pseudomembrane can resembles volcanic eruption. (b) At high power (20 x) the pseudomembrane forms a cap of fibrinous debris, mucin and inflammatory cells. (c) Crypts and lamina propria are inflamed (10 x).
Disclosures:
Samantha Woller indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Eva Holland indicated no relevant financial relationships.
Fnu Monika indicated no relevant financial relationships.
Wuttiporn Manatsathit indicated no relevant financial relationships.
Samantha Woller, MD, MS1, Clive Miranda, DO1, Eva Holland, 2, Fnu Monika, MBBS3, Wuttiporn Manatsathit, MD1. P1338 - A Fatal Case of Suspected <i>Clostridioides difficile</i> in a Patient with Native Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University Medical Center, Omaha, NE; 2Creighton University School of Medicine, Omaha, NE; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Clostridioides difficile (C. diff) is a well-known cause of colitis but involvement of the small intestine, referred to as C. diff enteritis, is exceedingly rare. C. diff enteritis is usually reported in patients with prior colectomy due to loss of the ileocecal valve. We present a fatal case of suspected C. diff enteritis in a patient with intact colonic anatomy.
Case Description/
Methods: A 39-year-old female with a history of systemic lupus erythematosus (SLE) and chronic pancytopenia presented with several days of pain, nausea, vomiting, and diarrhea. Imaging revealed jejunal and mesenteric edema consistent with enteritis. Labs revealed chronic pancytopenia and mildly elevated inflammatory markers. Initial differentials included medication toxicity, SLE flare, and infection.
Esophagogastroduodenoscopy (EGD) was unrevealing. A gastrointestinal pathogen panel was positive for C. diff and oral vancomycin was started. Despite treatment, symptoms persisted. Repeat imaging showed progressive small bowel thickening and ascites, without colonic involvement. Given the isolated findings, lupus enteritis (LE), intestinal angioedema, or mastocytosis. High-dose intravenous steroids were initiated but soon de-escalated by rheumatology due to unremarkable lupus markers. The patient acutely decompensated with peritonitis and underwent emergent laparotomy with small bowel resection. Pathology showed pseudomembranous enteritis and acute serositis. No viral or vasculitis etiology was identified. Despite further intervention, the patient continued to decline and was transitioned to comfort care.
Discussion: This case represents a rare and fatal presentation of presumed C. diff enteritis in a patient without prior colectomy. While both stool pathogen testing and histology were consistent with C. diff infection, definitive causality could not be confirmed. Other autoimmune etiologies were thought to be less likely. C. diff enteritis has primarily been reported with patients post-colectomy; this patient’s intact colon raises questions about factors that may have predisposed her to isolated small bowel involvement. It also highlights the association of the hypervirulent BI/NAP1/027 strain with enteritis. Strain typing may have clarified the etiology, but was unavailable. This case highlights the need for clinical awareness of atypical C. diff presentations, especially in immunocompromised patients, and underscores the importance of further research into diagnostic criteria and risk factors for enteric involvement.
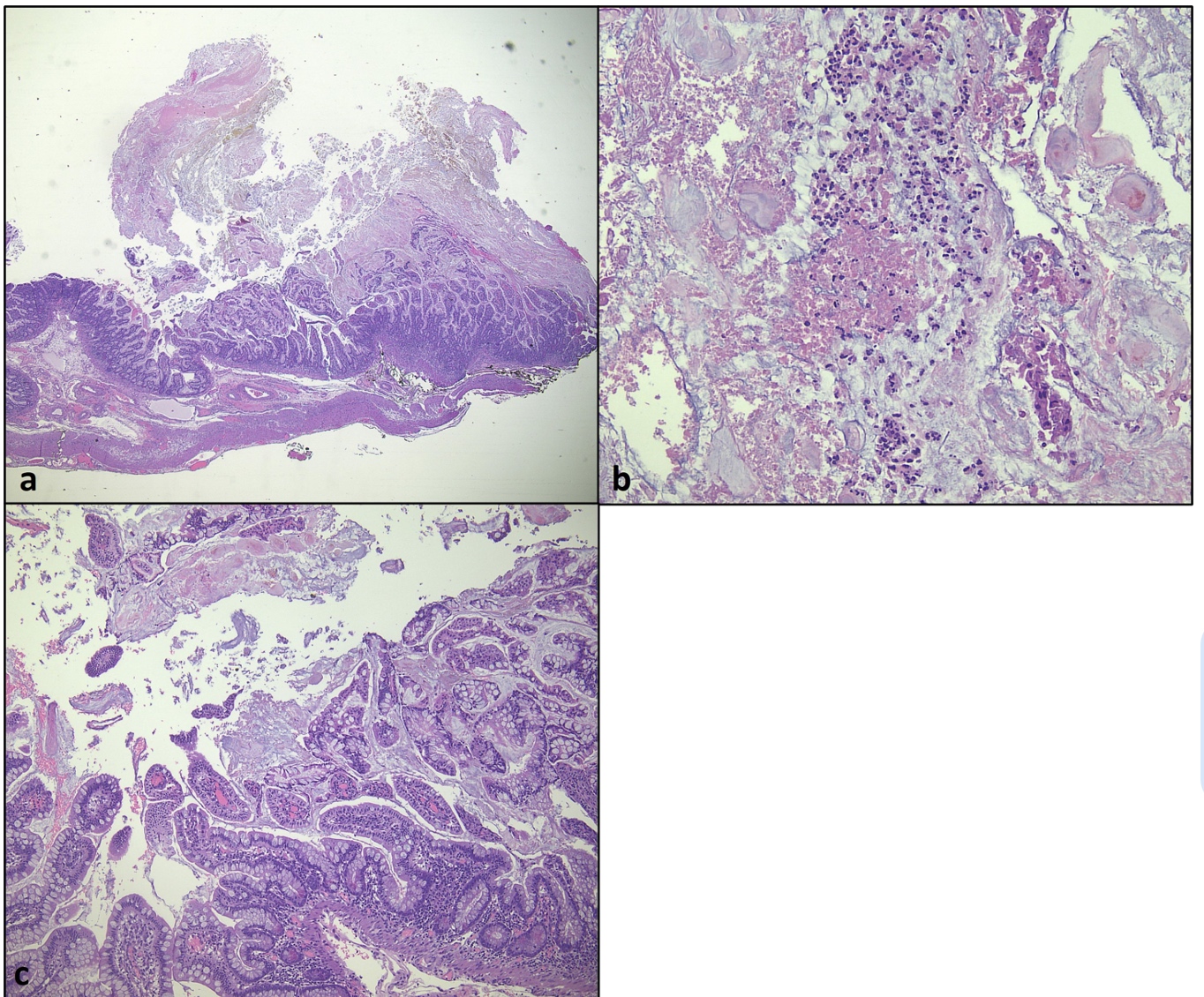
Figure: Figure 1. Pseudomembranous colitis. (a) At low power (2x), pseudomembrane can resembles volcanic eruption. (b) At high power (20 x) the pseudomembrane forms a cap of fibrinous debris, mucin and inflammatory cells. (c) Crypts and lamina propria are inflamed (10 x).
Disclosures:
Samantha Woller indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Eva Holland indicated no relevant financial relationships.
Fnu Monika indicated no relevant financial relationships.
Wuttiporn Manatsathit indicated no relevant financial relationships.
Samantha Woller, MD, MS1, Clive Miranda, DO1, Eva Holland, 2, Fnu Monika, MBBS3, Wuttiporn Manatsathit, MD1. P1338 - A Fatal Case of Suspected <i>Clostridioides difficile</i> in a Patient with Native Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
