Sunday Poster Session
Category: Infections and Microbiome
P1336 - Beyond the Usual Suspects: Brucellosis in the Differential of Abdominal Pain
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Daniel Stenberg, DO
University of Washington Medical Center
Seattle, WA
Presenting Author(s)
Daniel Stenberg, DO1, Virginia Wang, MD1, Lauren Taylor, BS2, Isabel Hujoel, MD1, Nina Saxena, MD1
1University of Washington Medical Center, Seattle, WA; 2University of Washington School of Medicine, Seattle, WA
Introduction: Brucellosis is a rare zoonosis with fewer than 200 U.S. cases annually, most often linked to unpasteurized dairy. It typically causes vague symptoms including fever, malaise, and arthralgias. While osteoarticular involvement is the most common complication, spinal infection with epidural extension is unusual (< 0.1%). Neurologic signs, when present, often appear late. Without a high index of suspicion, diagnosis is often delayed. We present a case of a brucellar spinal epidural abscess manifesting initially only as postprandial abdominal pain that led to early GI consultation. The ultimate etiology, spinal brucellosis, was uncovered only after broader imaging and a detailed exposure history revealed recent ingestion of unpasteurized camel’s milk.
Case Description/
Methods: A 52-year-old Muslim female of West African origin presented during Ramadan with two weeks of worsening postprandial right upper quadrant pain associated with nausea and vomiting, radiating to her back. Her exam was significant for RUQ tenderness. CT abdomen raised concern for gastritis vs early PUD, and GI was consulted. Labs and cultures remained normal. A HIDA scan, CT angiogram, EGD, and colonoscopy were unrevealing. An MRCP with unremarkable biliary findings incidentally captured a thoracic lesion. MRI revealed discitis-osteomyelitis with paravertebral spread and an epidural abscess causing canal stenosis, remarkably without neurologic deficits (see figures). CT-guided biopsy was negative, but brucellosis was confirmed by PCR and agglutination testing. She was found to travel to Ethiopia yearly and indulges in unpasteurized camel’s milk. She was discharged on oral antibiotics with outpatient ID follow-up.
Discussion: Brucellosis can mimic GI pathology. In this case, postprandial pain out of proportion to exam prompted extensive evaluation before imaging incidentally revealed spinal disease. Brucellosis may resemble pyogenic or neoplastic processes. Blood cultures are often negative, making PCR essential when risk factors like unpasteurized dairy are present. Treatment includes doxycycline and rifampin for at least 6 weeks. With epidural spread, extended therapy or aminoglycosides may be added. Surgery is rarely needed unless neurologic compromise occurs. This case highlights the value of a broad differential in the workup of abdominal pain, and the importance of exposure history in identifying uncommon infections.
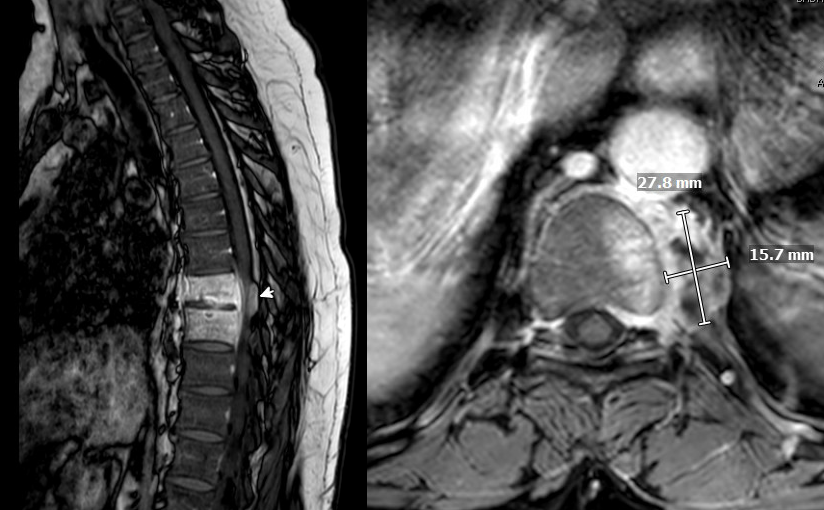
Figure: discitis-osteomyelitis with paravertebral spread and an epidural abscess causing canal stenosis
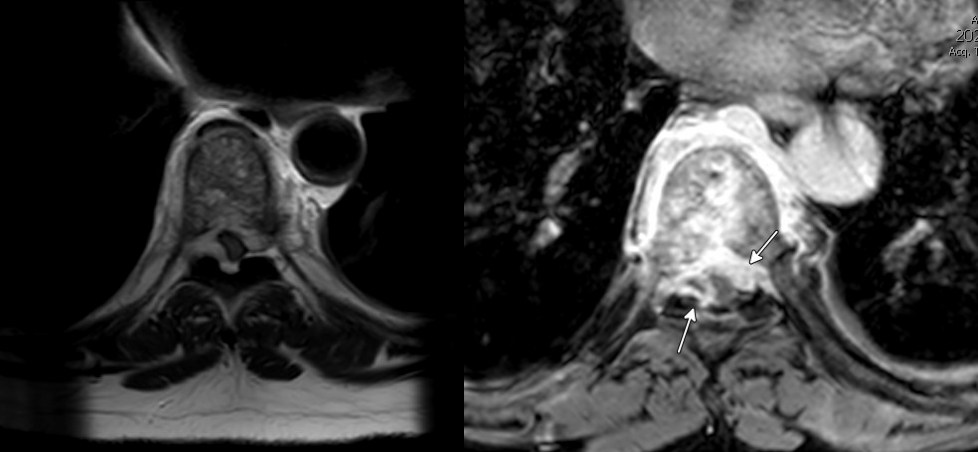
Figure: canal stenosis highlighted caused by discitis-osteomyelitis with paravertebral spread and an epidural abscess
Disclosures:
Daniel Stenberg indicated no relevant financial relationships.
Virginia Wang indicated no relevant financial relationships.
Lauren Taylor indicated no relevant financial relationships.
Isabel Hujoel indicated no relevant financial relationships.
Nina Saxena indicated no relevant financial relationships.
Daniel Stenberg, DO1, Virginia Wang, MD1, Lauren Taylor, BS2, Isabel Hujoel, MD1, Nina Saxena, MD1. P1336 - Beyond the Usual Suspects: Brucellosis in the Differential of Abdominal Pain, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Washington Medical Center, Seattle, WA; 2University of Washington School of Medicine, Seattle, WA
Introduction: Brucellosis is a rare zoonosis with fewer than 200 U.S. cases annually, most often linked to unpasteurized dairy. It typically causes vague symptoms including fever, malaise, and arthralgias. While osteoarticular involvement is the most common complication, spinal infection with epidural extension is unusual (< 0.1%). Neurologic signs, when present, often appear late. Without a high index of suspicion, diagnosis is often delayed. We present a case of a brucellar spinal epidural abscess manifesting initially only as postprandial abdominal pain that led to early GI consultation. The ultimate etiology, spinal brucellosis, was uncovered only after broader imaging and a detailed exposure history revealed recent ingestion of unpasteurized camel’s milk.
Case Description/
Methods: A 52-year-old Muslim female of West African origin presented during Ramadan with two weeks of worsening postprandial right upper quadrant pain associated with nausea and vomiting, radiating to her back. Her exam was significant for RUQ tenderness. CT abdomen raised concern for gastritis vs early PUD, and GI was consulted. Labs and cultures remained normal. A HIDA scan, CT angiogram, EGD, and colonoscopy were unrevealing. An MRCP with unremarkable biliary findings incidentally captured a thoracic lesion. MRI revealed discitis-osteomyelitis with paravertebral spread and an epidural abscess causing canal stenosis, remarkably without neurologic deficits (see figures). CT-guided biopsy was negative, but brucellosis was confirmed by PCR and agglutination testing. She was found to travel to Ethiopia yearly and indulges in unpasteurized camel’s milk. She was discharged on oral antibiotics with outpatient ID follow-up.
Discussion: Brucellosis can mimic GI pathology. In this case, postprandial pain out of proportion to exam prompted extensive evaluation before imaging incidentally revealed spinal disease. Brucellosis may resemble pyogenic or neoplastic processes. Blood cultures are often negative, making PCR essential when risk factors like unpasteurized dairy are present. Treatment includes doxycycline and rifampin for at least 6 weeks. With epidural spread, extended therapy or aminoglycosides may be added. Surgery is rarely needed unless neurologic compromise occurs. This case highlights the value of a broad differential in the workup of abdominal pain, and the importance of exposure history in identifying uncommon infections.
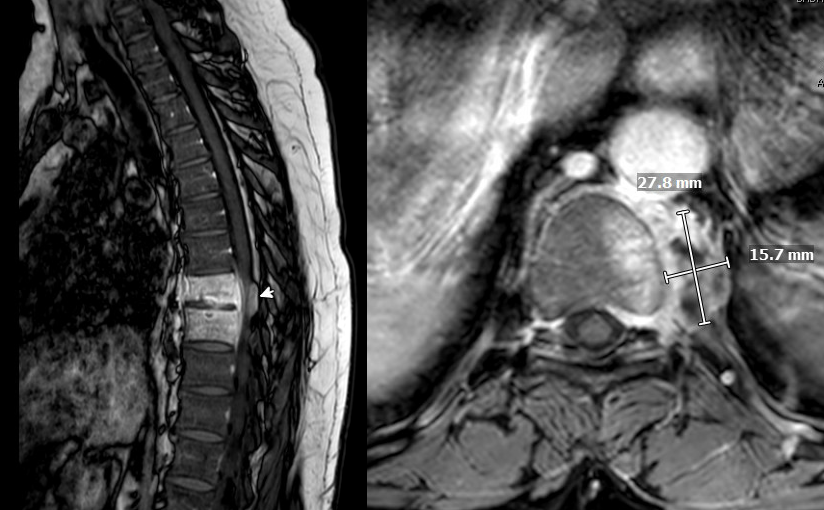
Figure: discitis-osteomyelitis with paravertebral spread and an epidural abscess causing canal stenosis
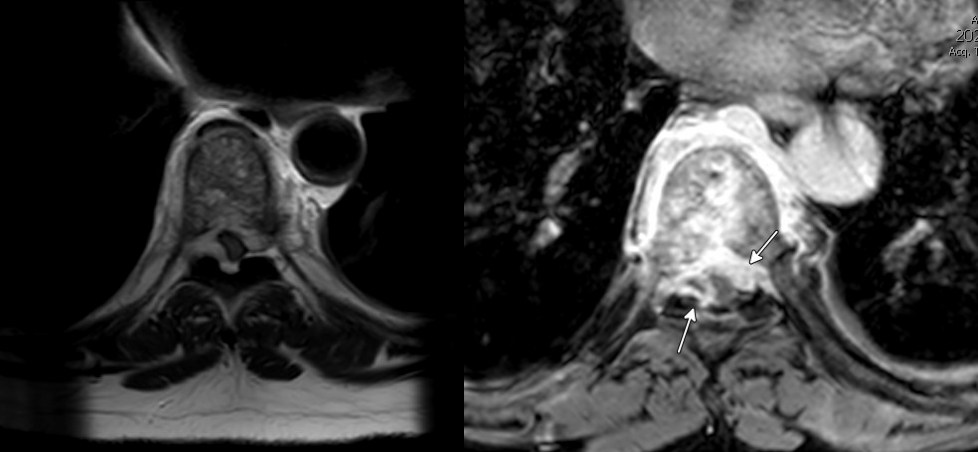
Figure: canal stenosis highlighted caused by discitis-osteomyelitis with paravertebral spread and an epidural abscess
Disclosures:
Daniel Stenberg indicated no relevant financial relationships.
Virginia Wang indicated no relevant financial relationships.
Lauren Taylor indicated no relevant financial relationships.
Isabel Hujoel indicated no relevant financial relationships.
Nina Saxena indicated no relevant financial relationships.
Daniel Stenberg, DO1, Virginia Wang, MD1, Lauren Taylor, BS2, Isabel Hujoel, MD1, Nina Saxena, MD1. P1336 - Beyond the Usual Suspects: Brucellosis in the Differential of Abdominal Pain, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
