Sunday Poster Session
Category: Infections and Microbiome
Utility of <i>C. difficile</i> Testing
P1333 - Utility of C. difficile Testing
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

David Glass, DO
Abington Jefferson Hospital
Abington, PA
Presenting Author(s)
David Glass, DO1, Dawood Tahir, MD2, Mark Bundschuh, MD1, Maliha Ahmed, MD1
1Abington Jefferson Hospital, Abington, PA; 2Jefferson Abington Hospital, Abington, PA
Introduction: C.difficile is a gram positive, spore forming, and obligate anaerobic bacillus. It causes a severe and contagious form of diarrhea world-wide. It is diagnosed with greater than 3 loose stools in 24 hours. PPI, immunosuppression, and anti-biotic use can lead to C.difficile. A variety of tests exist, including toxins A and B enzyme immunoassays (EIA) and ELISA. Treatments include oral Vancomycin and Fidaxomicin.
Case Description/
Methods: A 40 year old male with a past history of AAA and H. Pylori, who presented to the hospital due to abdominal pain and diarrhea. Symptoms began following completion of H.Pylori treatment. A week prior, he presented to the hospital with similar symptoms and CT abdomen/pelvis showed bowel wall edema. Following discharge, he traveled abroad and still had persistent abdominal pain. Upon return to the USA, he developed foul smelling diarrhea for 7 days, with 7 to 8 loose daily bowel movements. EIA Toxin Antigen Testing results were negative twice. Stool Cultures were negative. Infectious Disease was consulted due to the high clinical suspicion for C.difficile, despite negative testing. Patient was started on oral vancomycin with slow symptom improvement. Due symptom persistence he had a colonoscopy, which showed diffuse pseudomembranes, specifically acute inflammatory exudates with linear configuration of karyorrhectic debris and neutrophils. Biopsy confirmed C.difficile.
Discussion: C.difficile testing occurs through rapid EIAs, which is available at most hospitals. EIA sensitivity ranges from 44% to 99% compared to 100% for ELISA testing. As a standalone test, rapid EIAs are inadequate. ACG recommends utilizing a 2 step testing algorithm where GDH or Toxin B PCR is used as a screening test and the Toxin EIA confirms the diagnosis. IDSA recommends diagnosis with NAAT alone or 2- or 3-step testing (GDH immunoassay + toxin assay followed by NAAT only if either the GDH assay and toxin assay, but not both, are negative). If testing remains negative, studies have shown that flexible sigmoidoscopy can be superior to C.difficile cytotoxin test in patients with pseudomembranous colitis. This allows for direct visualization of the colon and biopsies can help rule out C.difficile, IBD, ischemic colitis, or other infectious causes. This case shows how rapid EIA testing delayed diagnosis. Other testing with EIA testing such as ELISA testing or flexible sigmoidoscopy can help confirm C.difficile. If there is high clinical suspicion of C.difficile, treatment should not be delayed.
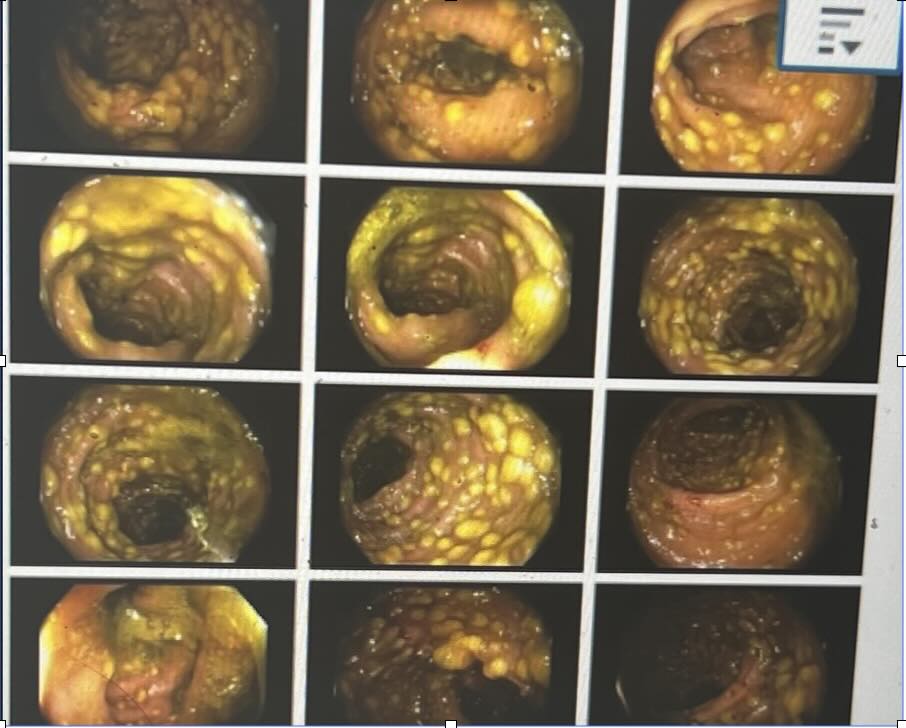
Figure: Patient with Pseudomebrane Colitis throughout entire colon.
Disclosures:
David Glass indicated no relevant financial relationships.
Dawood Tahir indicated no relevant financial relationships.
Mark Bundschuh indicated no relevant financial relationships.
Maliha Ahmed indicated no relevant financial relationships.
David Glass, DO1, Dawood Tahir, MD2, Mark Bundschuh, MD1, Maliha Ahmed, MD1. P1333 - Utility of <i>C. difficile</i> Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Abington Jefferson Hospital, Abington, PA; 2Jefferson Abington Hospital, Abington, PA
Introduction: C.difficile is a gram positive, spore forming, and obligate anaerobic bacillus. It causes a severe and contagious form of diarrhea world-wide. It is diagnosed with greater than 3 loose stools in 24 hours. PPI, immunosuppression, and anti-biotic use can lead to C.difficile. A variety of tests exist, including toxins A and B enzyme immunoassays (EIA) and ELISA. Treatments include oral Vancomycin and Fidaxomicin.
Case Description/
Methods: A 40 year old male with a past history of AAA and H. Pylori, who presented to the hospital due to abdominal pain and diarrhea. Symptoms began following completion of H.Pylori treatment. A week prior, he presented to the hospital with similar symptoms and CT abdomen/pelvis showed bowel wall edema. Following discharge, he traveled abroad and still had persistent abdominal pain. Upon return to the USA, he developed foul smelling diarrhea for 7 days, with 7 to 8 loose daily bowel movements. EIA Toxin Antigen Testing results were negative twice. Stool Cultures were negative. Infectious Disease was consulted due to the high clinical suspicion for C.difficile, despite negative testing. Patient was started on oral vancomycin with slow symptom improvement. Due symptom persistence he had a colonoscopy, which showed diffuse pseudomembranes, specifically acute inflammatory exudates with linear configuration of karyorrhectic debris and neutrophils. Biopsy confirmed C.difficile.
Discussion: C.difficile testing occurs through rapid EIAs, which is available at most hospitals. EIA sensitivity ranges from 44% to 99% compared to 100% for ELISA testing. As a standalone test, rapid EIAs are inadequate. ACG recommends utilizing a 2 step testing algorithm where GDH or Toxin B PCR is used as a screening test and the Toxin EIA confirms the diagnosis. IDSA recommends diagnosis with NAAT alone or 2- or 3-step testing (GDH immunoassay + toxin assay followed by NAAT only if either the GDH assay and toxin assay, but not both, are negative). If testing remains negative, studies have shown that flexible sigmoidoscopy can be superior to C.difficile cytotoxin test in patients with pseudomembranous colitis. This allows for direct visualization of the colon and biopsies can help rule out C.difficile, IBD, ischemic colitis, or other infectious causes. This case shows how rapid EIA testing delayed diagnosis. Other testing with EIA testing such as ELISA testing or flexible sigmoidoscopy can help confirm C.difficile. If there is high clinical suspicion of C.difficile, treatment should not be delayed.
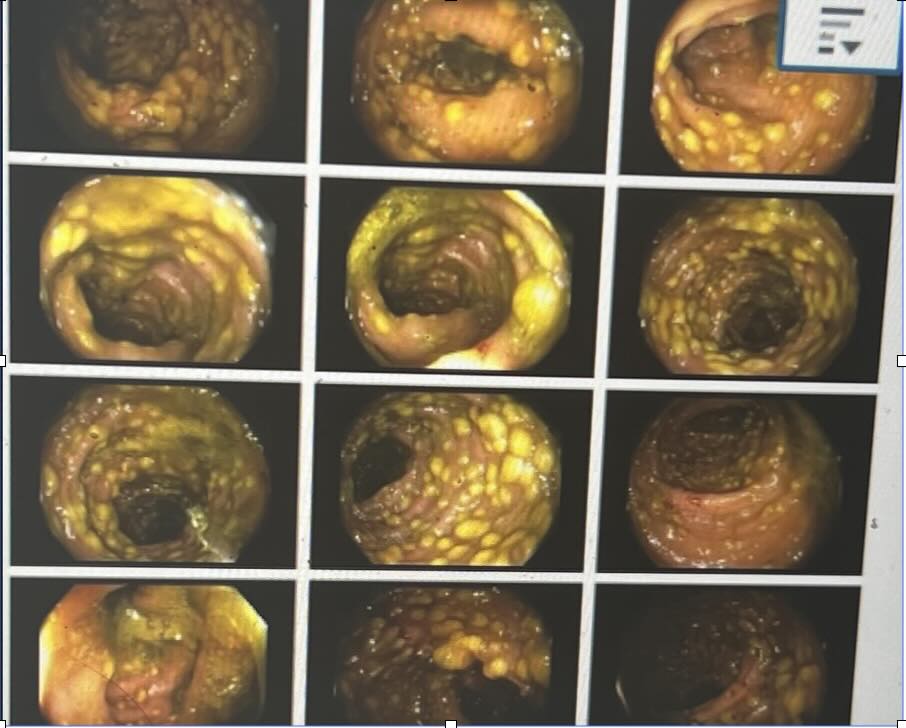
Figure: Patient with Pseudomebrane Colitis throughout entire colon.
Disclosures:
David Glass indicated no relevant financial relationships.
Dawood Tahir indicated no relevant financial relationships.
Mark Bundschuh indicated no relevant financial relationships.
Maliha Ahmed indicated no relevant financial relationships.
David Glass, DO1, Dawood Tahir, MD2, Mark Bundschuh, MD1, Maliha Ahmed, MD1. P1333 - Utility of <i>C. difficile</i> Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
