Sunday Poster Session
Category: Infections and Microbiome
P1332 - The Fungal Specter: A Sinister Liver Abscess by Candida glabrata
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Sabrina Ho, MD
Banner - University of Arizona Tucson
Tucson, AZ
Presenting Author(s)
Sabrina Ho, MD1, Samuel Cheong, DO2, Mohamad Omar Diab, MD3, Franklin Liu, MD2, Brandon Witten, MD1
1Banner - University of Arizona Tucson, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ; 3Canyon Vista Medical Center, Sierra Vista, AZ
Introduction: Candida glabrata was once considered a non-pathogenic organism. Now, it’s recognized as a high-priority pathogen due to its increasing resistance to antifungal agents. The reported incidence ranges from 0.67 to 2.66 cases per 100,000 individuals per year. We present a rare case of a liver abscess caused by Candida glabrata.
Case Description/
Methods: A 57-year-old male with a history of heart failure, atrial fibrillation status post-ablation, end-stage renal disease (ESRD), and decompensated alcoholic cirrhosis complicated by spontaneous bacterial peritonitis (SBP) and hepatic encephalopathy presented with worsening anasarca, dyspnea on exertion, and leakage from a recently placed cholecystostomy tube for acute cholecystitis. A multidisciplinary discussion involving surgery, gastroenterology, and interventional radiology (IR) was conducted regarding management of the cholecystostomy tube. Ultimately, IR performed a percutaneous cholecystoduodenostomy with placement of a lumen-apposing stent, and the existing drain was exchanged.
During his prolonged hospitalization, the patient required multiple ICU transfers for hypotension due to suspected septic shock. He was empirically treated with vancomycin and meropenem. He underwent multiple paracenteses for recurrent ascites and abdominal pain. One of the ascitic fluid samples cultured pan-sensitive Candida glabrata. Micafungin was initiated, and infectious disease was consulted. Imaging revealed worsening pneumoperitoneum and an abscess (9.7 × 4.5 × 0.5 cm). IR drained the abscess, yielding 40 cc of purulent material. Cultures confirmed pan-sensitive Candida glabrata. The patient was transitioned to oral fluconazole, and the drain was subsequently removed.
Unfortunately, follow-up imaging revealed recurrence of a liver abscess; however, cultures were negative for Candida glabrata.
Discussion: Candida liver abscesses are uncommon and typically occur in the context of disseminated candidemia, with an incidence of less than 15%. Known risk factors include immunosuppression, prolonged parenteral nutrition, diabetes mellitus, and prior exposure to broad-spectrum antibiotics. In this case, repeated instrumentation also likely contributed. Fortunately, the strain isolated was pan-sensitive, allowing transition to fluconazole on discharge. The CDC recommends repeat imaging at 3- to 6-month intervals and a minimum of 6 months of follow-up to confirm resolution. The optimal duration of antifungal therapy, however, remains unclear.
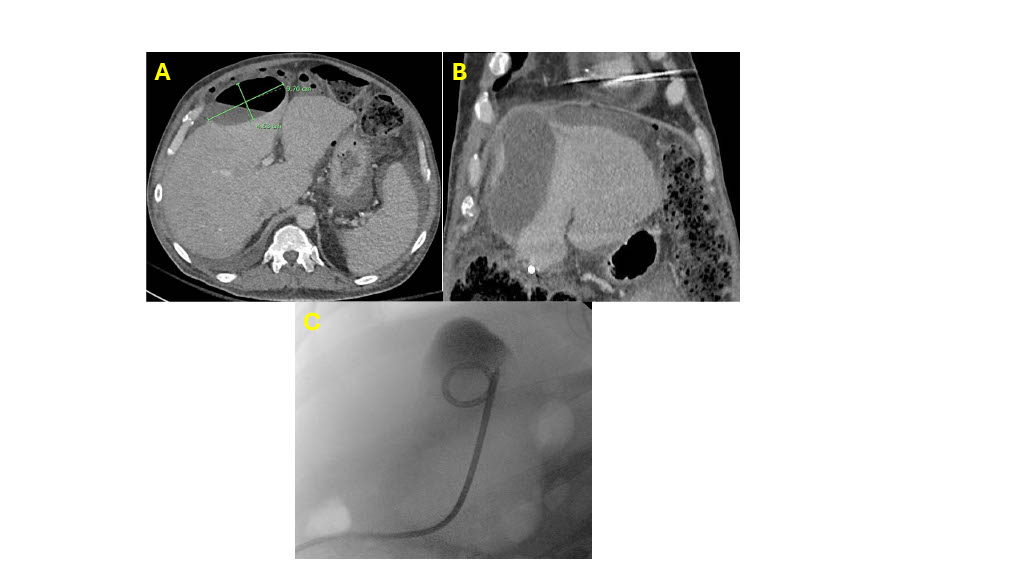
Figure: A. CT scan with liver abscess measuring 9.7cm x 4.53 cm.
B. Coronal view of the liver abscess.
C. IR drainage of liver abscess
Disclosures:
Sabrina Ho indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Franklin Liu indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Sabrina Ho, MD1, Samuel Cheong, DO2, Mohamad Omar Diab, MD3, Franklin Liu, MD2, Brandon Witten, MD1. P1332 - The Fungal Specter: A Sinister Liver Abscess by Candida glabrata, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Banner - University of Arizona Tucson, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ; 3Canyon Vista Medical Center, Sierra Vista, AZ
Introduction: Candida glabrata was once considered a non-pathogenic organism. Now, it’s recognized as a high-priority pathogen due to its increasing resistance to antifungal agents. The reported incidence ranges from 0.67 to 2.66 cases per 100,000 individuals per year. We present a rare case of a liver abscess caused by Candida glabrata.
Case Description/
Methods: A 57-year-old male with a history of heart failure, atrial fibrillation status post-ablation, end-stage renal disease (ESRD), and decompensated alcoholic cirrhosis complicated by spontaneous bacterial peritonitis (SBP) and hepatic encephalopathy presented with worsening anasarca, dyspnea on exertion, and leakage from a recently placed cholecystostomy tube for acute cholecystitis. A multidisciplinary discussion involving surgery, gastroenterology, and interventional radiology (IR) was conducted regarding management of the cholecystostomy tube. Ultimately, IR performed a percutaneous cholecystoduodenostomy with placement of a lumen-apposing stent, and the existing drain was exchanged.
During his prolonged hospitalization, the patient required multiple ICU transfers for hypotension due to suspected septic shock. He was empirically treated with vancomycin and meropenem. He underwent multiple paracenteses for recurrent ascites and abdominal pain. One of the ascitic fluid samples cultured pan-sensitive Candida glabrata. Micafungin was initiated, and infectious disease was consulted. Imaging revealed worsening pneumoperitoneum and an abscess (9.7 × 4.5 × 0.5 cm). IR drained the abscess, yielding 40 cc of purulent material. Cultures confirmed pan-sensitive Candida glabrata. The patient was transitioned to oral fluconazole, and the drain was subsequently removed.
Unfortunately, follow-up imaging revealed recurrence of a liver abscess; however, cultures were negative for Candida glabrata.
Discussion: Candida liver abscesses are uncommon and typically occur in the context of disseminated candidemia, with an incidence of less than 15%. Known risk factors include immunosuppression, prolonged parenteral nutrition, diabetes mellitus, and prior exposure to broad-spectrum antibiotics. In this case, repeated instrumentation also likely contributed. Fortunately, the strain isolated was pan-sensitive, allowing transition to fluconazole on discharge. The CDC recommends repeat imaging at 3- to 6-month intervals and a minimum of 6 months of follow-up to confirm resolution. The optimal duration of antifungal therapy, however, remains unclear.
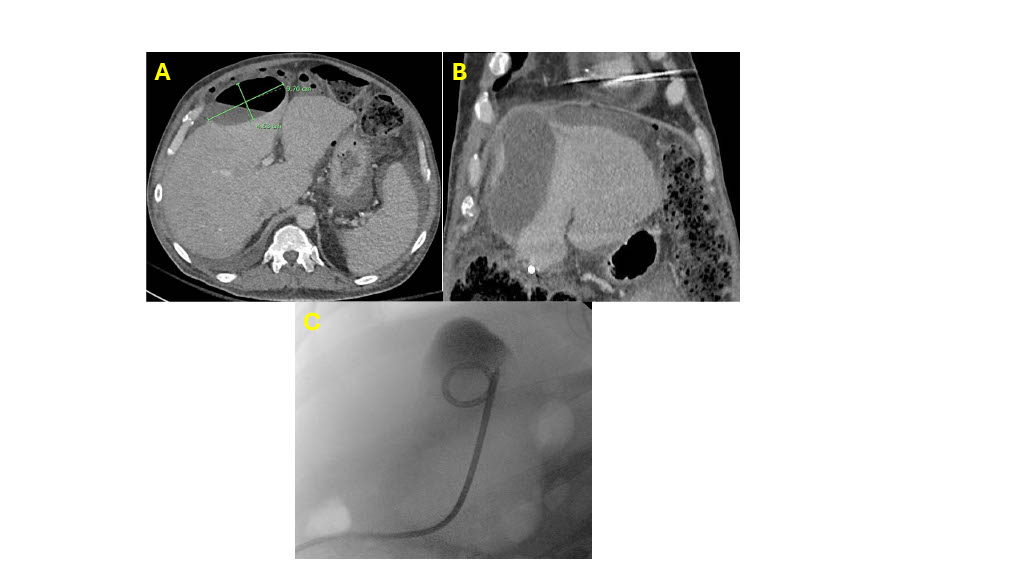
Figure: A. CT scan with liver abscess measuring 9.7cm x 4.53 cm.
B. Coronal view of the liver abscess.
C. IR drainage of liver abscess
Disclosures:
Sabrina Ho indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Mohamad Omar Diab indicated no relevant financial relationships.
Franklin Liu indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Sabrina Ho, MD1, Samuel Cheong, DO2, Mohamad Omar Diab, MD3, Franklin Liu, MD2, Brandon Witten, MD1. P1332 - The Fungal Specter: A Sinister Liver Abscess by Candida glabrata, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
