Sunday Poster Session
Category: Infections and Microbiome
P1308 - A Multicenter Retrospective Study on the Clinical Yield of Ova and Parasite Testing in South Florida
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amanda Renee Eukovich, DO
Broward Health Medical Center
Pompano Beach, FL
Presenting Author(s)
Amanda Renee. Eukovich, DO1, Lorraine Chong Tai, MD2, Andrea Escalante, DO2, Edwin Makarevich, DO2, Ivana Rubenstein, DO2
1Broward Health Medical Center, Pompano Beach, FL; 2Broward Health Medical Center, Fort Lauderdale, FL
Introduction: Ova and parasite (O&P) testing is often routinely used in the work-up of diarrhea. The test involves the microscopic examination of stool, which is then permanently fixed onto a slide with iodine and trichrome staining. The total turn-around time is three-to-seven days. The US has over 179 million cases of diarrheal illnesses per year, and most cases resolve with symptomatic treatment alone. In the inpatient setting, the prevalence of parasitic disease is less than 5%. Despite this fact, O&P testing is commonly ordered in acute diarrheal illness. These tests are expensive and time-consuming. Collection methods and medications can alter test results. Indications for O&P testing are persistent diarrhea (more than 7 days), advanced HIV infection, and travel to regions where parasites are endemic. This study retrospectively reviewed all ova and parasite testing between January 1st, 2023 and December 31st, 2024 in individuals over the age of eighteen.
Methods: The hospital is a 1,579-bed multi-center facility located in South Florida with a large international population and cruise-ship transfers. The cost of each O&P test at this facility is $25. A total of 520 O&P tests were performed during this time frame. Inclusion criteria included diarrhea for more than seven days, immunocompromised status, or recent travel to parasite-prone regions. Immunocompromised patients included those with a history of malignancy, autoimmune conditions, HIV/AIDS, transplant, sickle cell disease, ESRD, chronic liver disease, and moderate or severe primary immunodeficiency. Endemic regions included Central America, South America, Africa, Egypt, and Asia.
Results: Of the 520 tests ordered, only 145 tests (27.9%) met the inclusion criteria. 375 tests (72.1%) were inappropriately ordered. Within the inclusion criteria (145 patients), only 7 were positive (4.8%). Thus, appropriate ordering of O&P testing could have saved $9,375. Interestingly, an additional 5 patients tested positive on a PCR panel but not on O&P testing.
Discussion: In conclusion, O&P studies are often inappropriately ordered and low-yield. Other testing methods, such as enzyme immunoassays (EIA), have been shown to be superior to O&P. EIAs can rapidly detect antibodies and only require one stool sample. If an O&P is selected, it has the highest utility if performed upon admission if diarrhea is present. O&P testing is not routinely recommended in immunocompetent patients, as most infections resolve without antimicrobials.
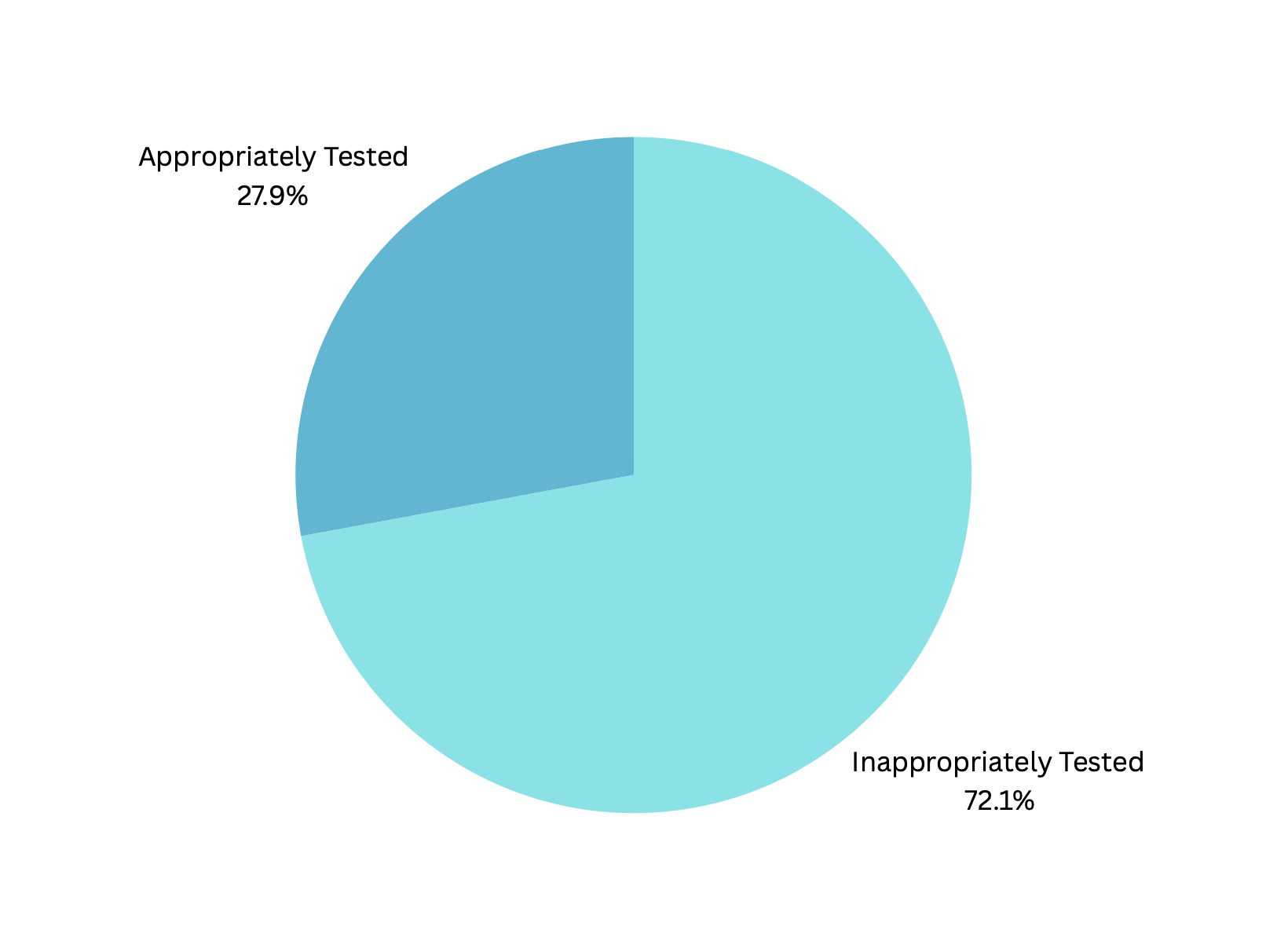
Figure: Figure 1. Appropriate O&P Testing; only 27.9% met inclusion criteria.
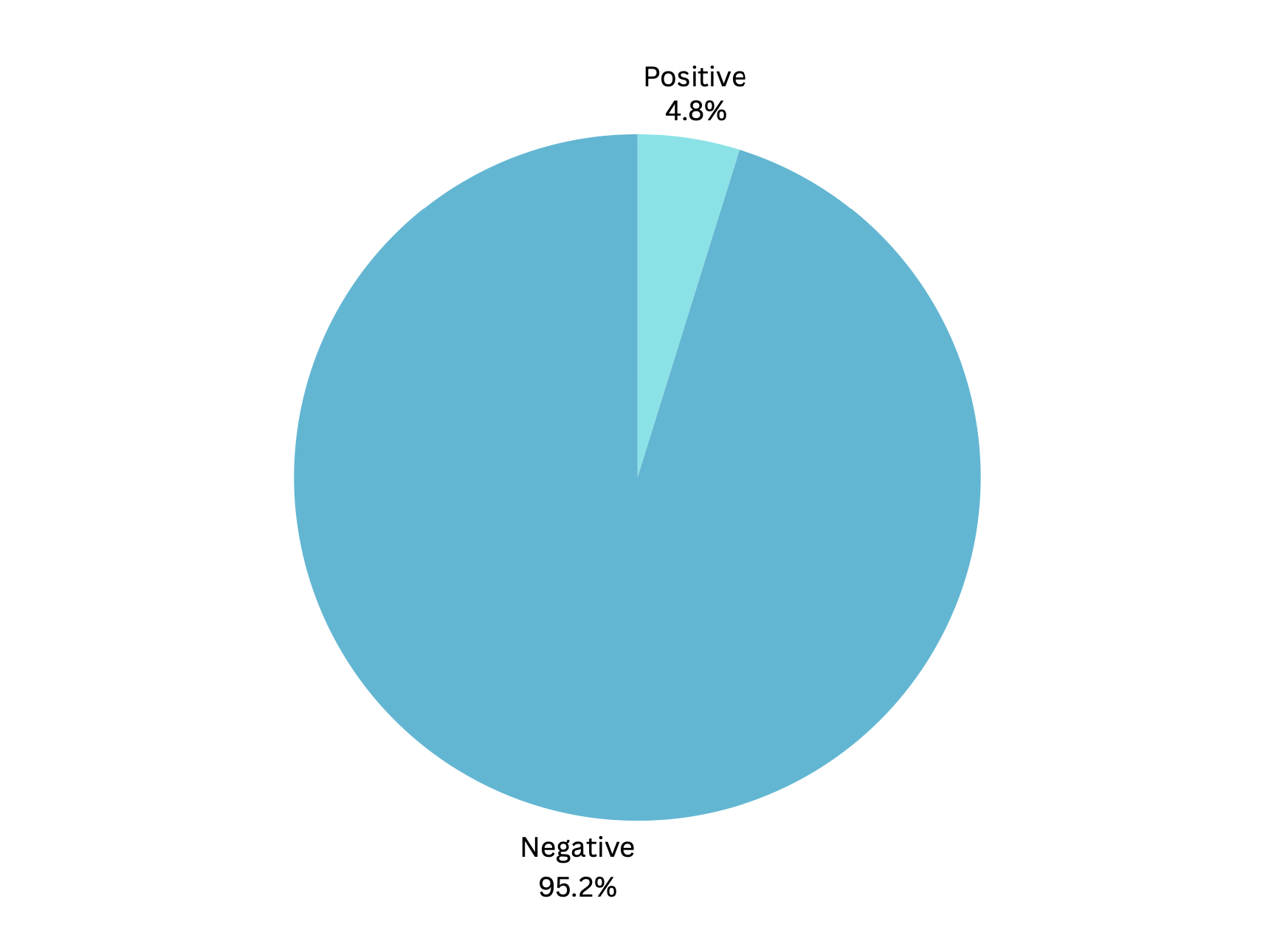
Figure: Figure 2. Positive O&P test; Only 4.8% of patients who met the inclusion criteria tested positive.
Disclosures:
Amanda Eukovich indicated no relevant financial relationships.
Lorraine Chong Tai indicated no relevant financial relationships.
Andrea Escalante indicated no relevant financial relationships.
Edwin Makarevich indicated no relevant financial relationships.
Ivana Rubenstein indicated no relevant financial relationships.
Amanda Renee. Eukovich, DO1, Lorraine Chong Tai, MD2, Andrea Escalante, DO2, Edwin Makarevich, DO2, Ivana Rubenstein, DO2. P1308 - A Multicenter Retrospective Study on the Clinical Yield of Ova and Parasite Testing in South Florida, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Broward Health Medical Center, Pompano Beach, FL; 2Broward Health Medical Center, Fort Lauderdale, FL
Introduction: Ova and parasite (O&P) testing is often routinely used in the work-up of diarrhea. The test involves the microscopic examination of stool, which is then permanently fixed onto a slide with iodine and trichrome staining. The total turn-around time is three-to-seven days. The US has over 179 million cases of diarrheal illnesses per year, and most cases resolve with symptomatic treatment alone. In the inpatient setting, the prevalence of parasitic disease is less than 5%. Despite this fact, O&P testing is commonly ordered in acute diarrheal illness. These tests are expensive and time-consuming. Collection methods and medications can alter test results. Indications for O&P testing are persistent diarrhea (more than 7 days), advanced HIV infection, and travel to regions where parasites are endemic. This study retrospectively reviewed all ova and parasite testing between January 1st, 2023 and December 31st, 2024 in individuals over the age of eighteen.
Methods: The hospital is a 1,579-bed multi-center facility located in South Florida with a large international population and cruise-ship transfers. The cost of each O&P test at this facility is $25. A total of 520 O&P tests were performed during this time frame. Inclusion criteria included diarrhea for more than seven days, immunocompromised status, or recent travel to parasite-prone regions. Immunocompromised patients included those with a history of malignancy, autoimmune conditions, HIV/AIDS, transplant, sickle cell disease, ESRD, chronic liver disease, and moderate or severe primary immunodeficiency. Endemic regions included Central America, South America, Africa, Egypt, and Asia.
Results: Of the 520 tests ordered, only 145 tests (27.9%) met the inclusion criteria. 375 tests (72.1%) were inappropriately ordered. Within the inclusion criteria (145 patients), only 7 were positive (4.8%). Thus, appropriate ordering of O&P testing could have saved $9,375. Interestingly, an additional 5 patients tested positive on a PCR panel but not on O&P testing.
Discussion: In conclusion, O&P studies are often inappropriately ordered and low-yield. Other testing methods, such as enzyme immunoassays (EIA), have been shown to be superior to O&P. EIAs can rapidly detect antibodies and only require one stool sample. If an O&P is selected, it has the highest utility if performed upon admission if diarrhea is present. O&P testing is not routinely recommended in immunocompetent patients, as most infections resolve without antimicrobials.
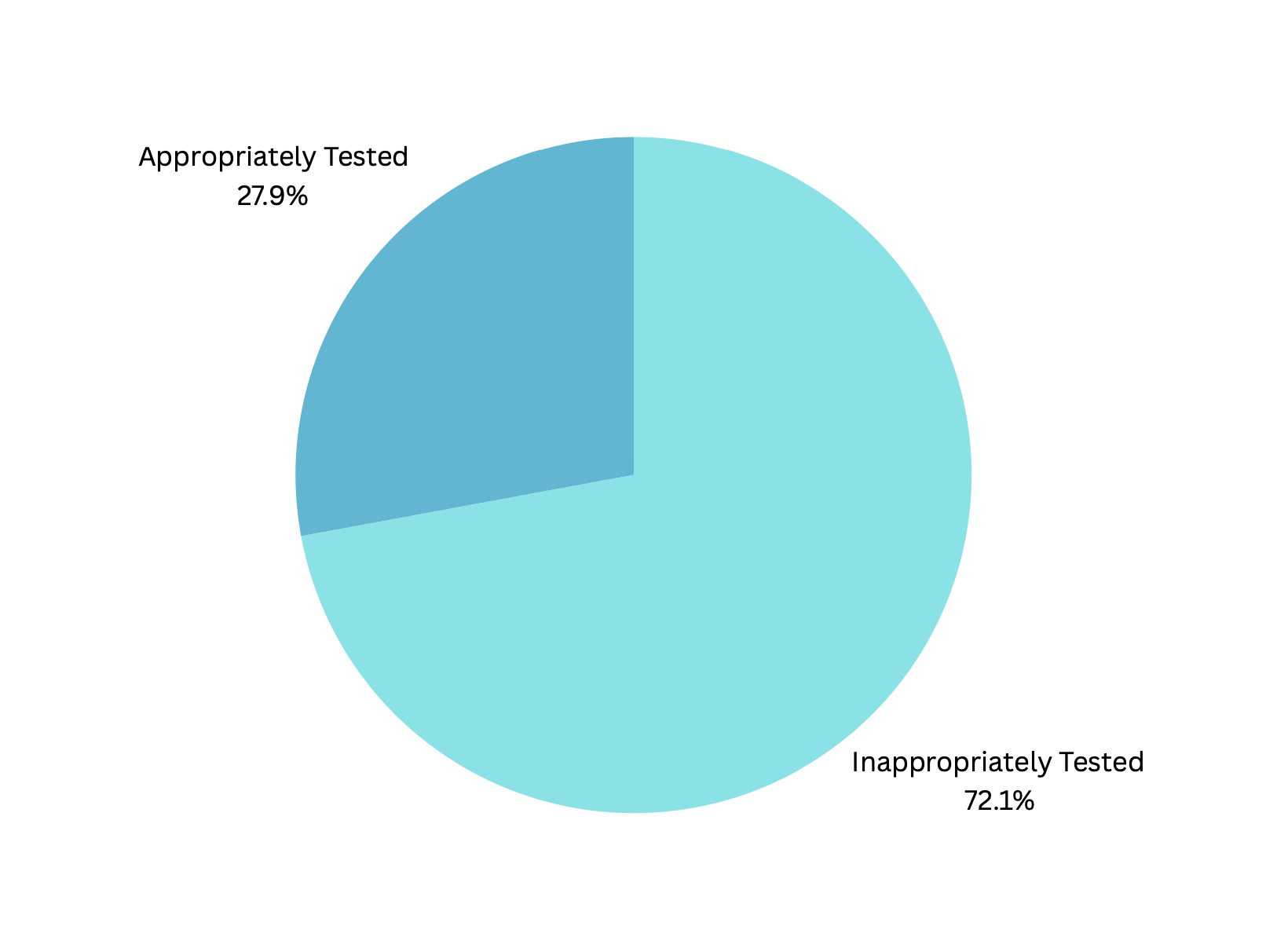
Figure: Figure 1. Appropriate O&P Testing; only 27.9% met inclusion criteria.
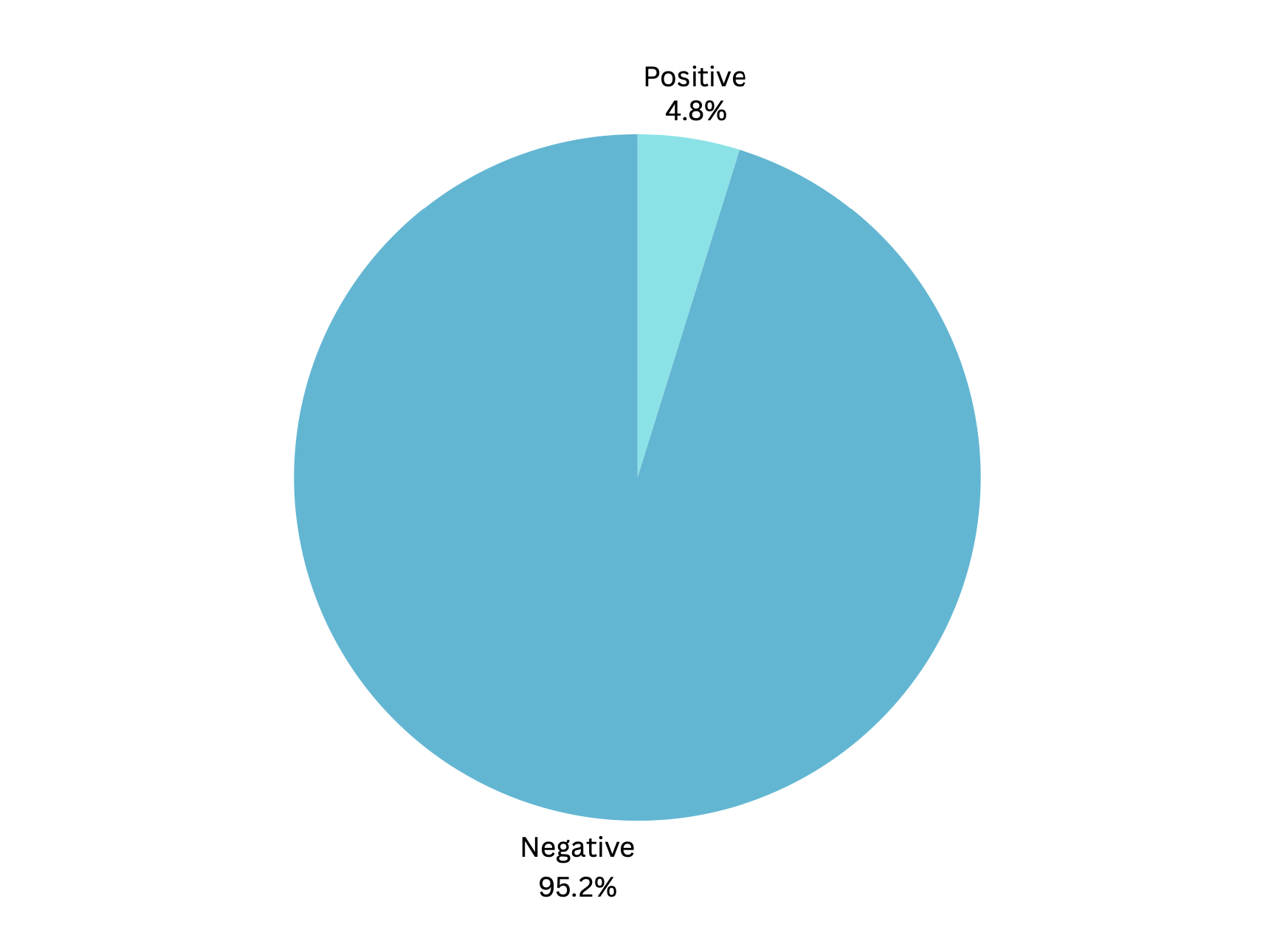
Figure: Figure 2. Positive O&P test; Only 4.8% of patients who met the inclusion criteria tested positive.
Disclosures:
Amanda Eukovich indicated no relevant financial relationships.
Lorraine Chong Tai indicated no relevant financial relationships.
Andrea Escalante indicated no relevant financial relationships.
Edwin Makarevich indicated no relevant financial relationships.
Ivana Rubenstein indicated no relevant financial relationships.
Amanda Renee. Eukovich, DO1, Lorraine Chong Tai, MD2, Andrea Escalante, DO2, Edwin Makarevich, DO2, Ivana Rubenstein, DO2. P1308 - A Multicenter Retrospective Study on the Clinical Yield of Ova and Parasite Testing in South Florida, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
