Sunday Poster Session
Category: Infections and Microbiome
P1307 - Impact of GI PCR versus Stool Culture on Clinical Outcomes in Hospitalized Patients: A Retrospective Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Bolaji O. Ayinde, MD
Northeast Georgia Medical Center
Gainesville, GA
Presenting Author(s)
Bolaji O. Ayinde, MD1, Mena Louis, DO2, Adeel Akhtar, MD1, Ana Tucker, PhD1, Jake Slaton, MS3, Phillip J. Gross, MD, MPH4
1Northeast Georgia Medical Center, Gainesville, GA; 2NGHS, Oakwood, GA; 3Northeast Georgia Medical Center, Duluth, GA; 4Northeast Georgia Health System, Gainesville, GA
Introduction: Gastrointestinal (GI) infections constitute a frequent cause of hospitalization, typically requiring immediate diagnosis to direct treatment. While standard stool culture is widely utilized, it is constrained by lengthy turnaround times. Multiplex gastrointestinal PCR (GI PCR) facilitates a wider and quicker identification of pathogens. This study evaluates the clinical implications of GI PCR compared to stool culture in patients hospitalized with suspected infectious gastroenteritis.
Methods: A retrospective cohort study conducted at a major regional health system examined adult inpatients with positive stool culture, GI PCR, or both from January 2019 to September 2024. The primary outcome was hospital length of stay (LOS). Secondary outcomes included appropriate antibiotic use, antibiotic duration, and inpatient colonoscopy rates. LOS and antibiotic duration were modeled using generalized additive models for location, scale, and shape (GAMLSS); logistic regression was used for antibiotic appropriateness.
Results: Of the 408 positive patients, 154 were positive just on stool culture, 153 on GI PCR, and 101 on both. GI PCR was associated with a 33.6% reduction in mean LOS compared to stool culture (IRR 0.664, 95% CI 0.526–0.840, P < 0.001). Appropriate antibiotic use occurred in 59.5% of PCR patients versus 21.4% of those with stool culture alone (OR 5.38, 95% CI 3.26–8.89, P < 0.001). Median antibiotic duration was similar across groups. Colonoscopy was rare (2.0%) and did not differ by test type.
Discussion: This study showed that utilizing GI PCR panels for hospitalized patients with suspected infectious gastroenteritis reduced hospital stays and dramatically improved antibiotic prescribing. Patients screened with PCR had more than 30% shorter stays and were five times more likely to receive adequate antibiotics than those tested with stool culture. PCR produced faster results, allowing for early, focused treatment. Patients who received both PCR and culture did not see the similar LOS reduction, emphasizing the need of early PCR-driven decisions. While antibiotic duration was comparable between groups, PCR resulted in more appropriate and individualized use, without increasing overall exposure. Colonoscopy rates were found to be low and did not differ according to the type of test performed. The study's limitations encompass its retrospective design, potential selection bias, a single-center context, and the unmeasured effects of costs.
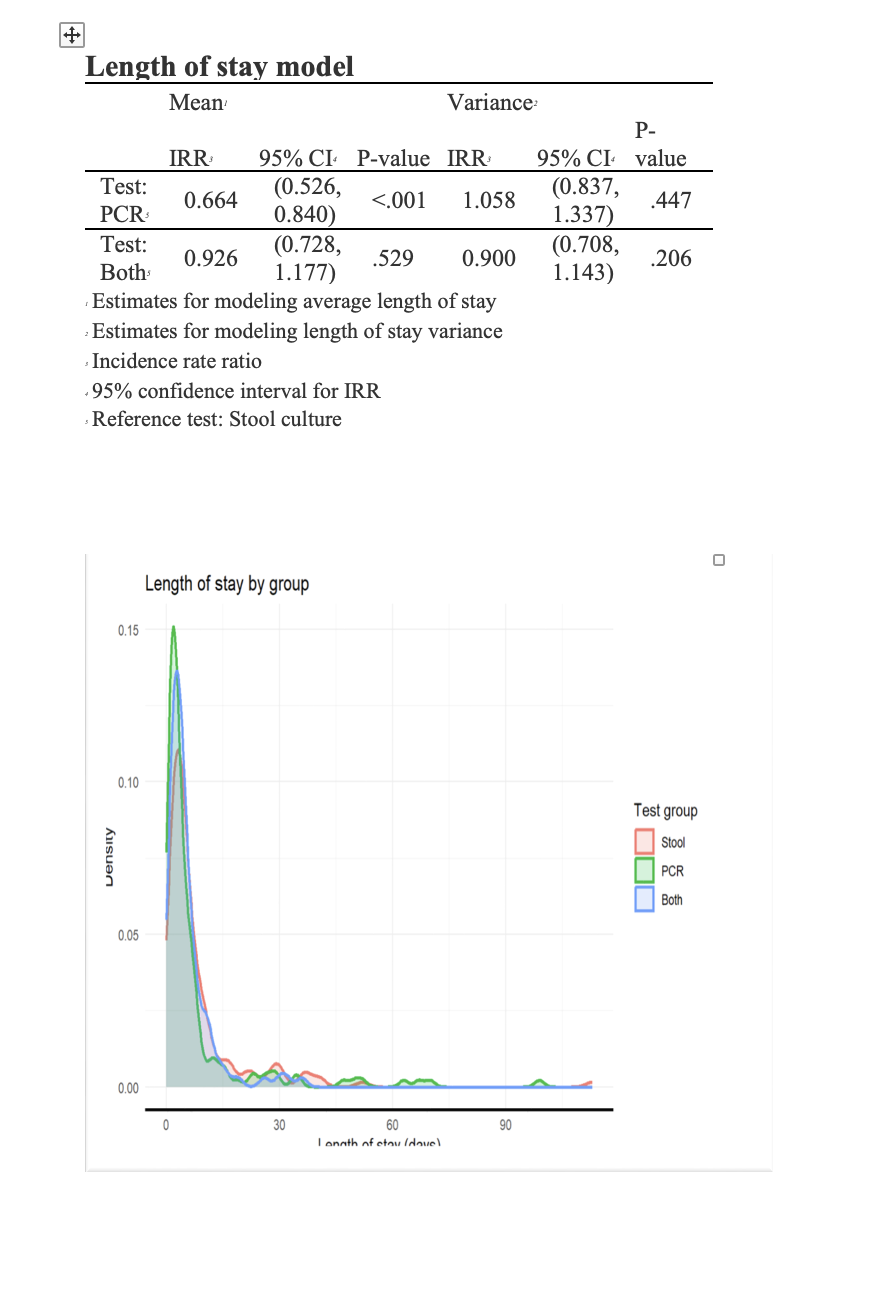
Figure: Length of Stay Model
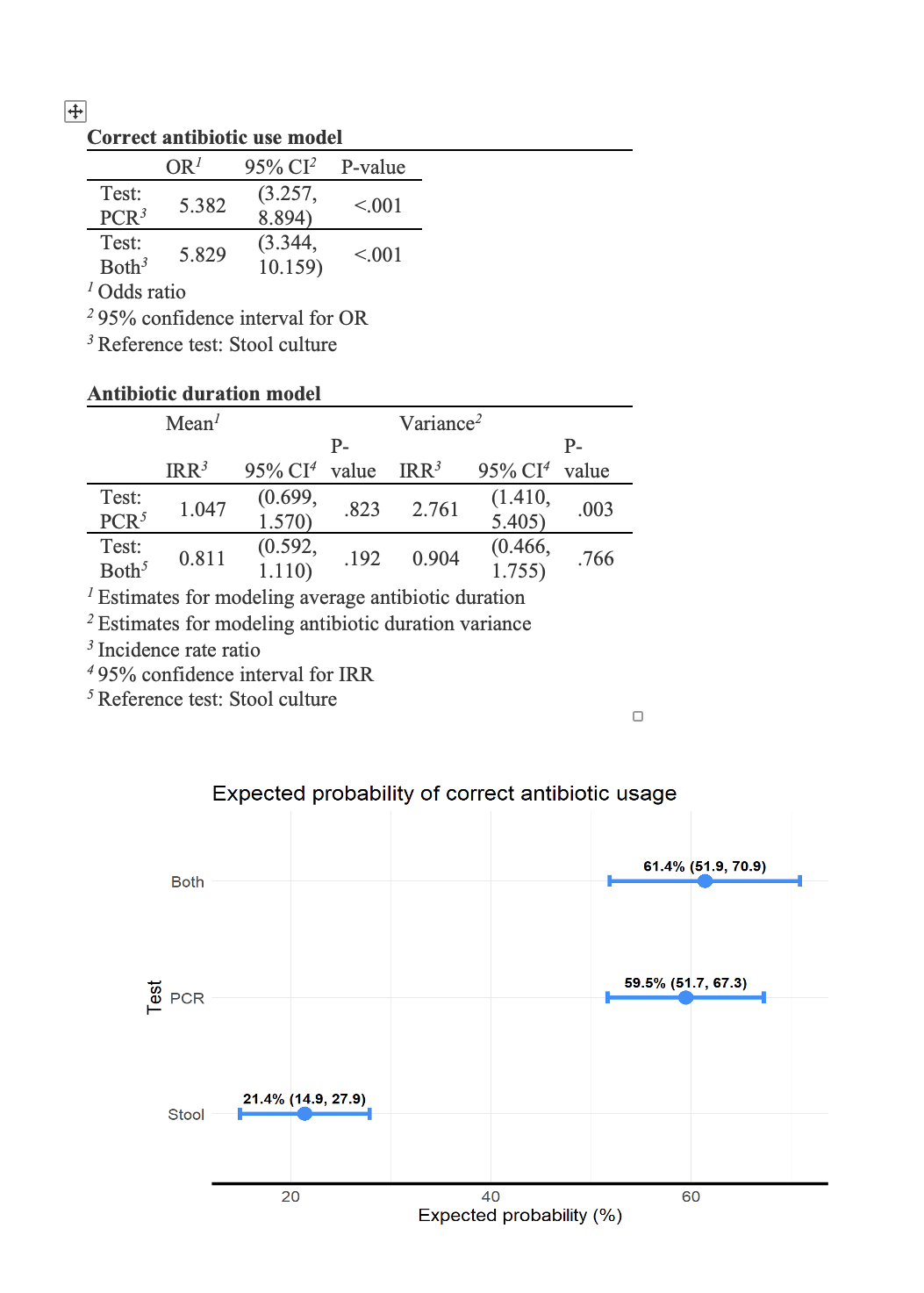
Figure: Antibiotics Use Model
Disclosures:
Bolaji Ayinde indicated no relevant financial relationships.
Mena Louis indicated no relevant financial relationships.
Adeel Akhtar indicated no relevant financial relationships.
Ana Tucker indicated no relevant financial relationships.
Jake Slaton indicated no relevant financial relationships.
Phillip Gross indicated no relevant financial relationships.
Bolaji O. Ayinde, MD1, Mena Louis, DO2, Adeel Akhtar, MD1, Ana Tucker, PhD1, Jake Slaton, MS3, Phillip J. Gross, MD, MPH4. P1307 - Impact of GI PCR versus Stool Culture on Clinical Outcomes in Hospitalized Patients: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northeast Georgia Medical Center, Gainesville, GA; 2NGHS, Oakwood, GA; 3Northeast Georgia Medical Center, Duluth, GA; 4Northeast Georgia Health System, Gainesville, GA
Introduction: Gastrointestinal (GI) infections constitute a frequent cause of hospitalization, typically requiring immediate diagnosis to direct treatment. While standard stool culture is widely utilized, it is constrained by lengthy turnaround times. Multiplex gastrointestinal PCR (GI PCR) facilitates a wider and quicker identification of pathogens. This study evaluates the clinical implications of GI PCR compared to stool culture in patients hospitalized with suspected infectious gastroenteritis.
Methods: A retrospective cohort study conducted at a major regional health system examined adult inpatients with positive stool culture, GI PCR, or both from January 2019 to September 2024. The primary outcome was hospital length of stay (LOS). Secondary outcomes included appropriate antibiotic use, antibiotic duration, and inpatient colonoscopy rates. LOS and antibiotic duration were modeled using generalized additive models for location, scale, and shape (GAMLSS); logistic regression was used for antibiotic appropriateness.
Results: Of the 408 positive patients, 154 were positive just on stool culture, 153 on GI PCR, and 101 on both. GI PCR was associated with a 33.6% reduction in mean LOS compared to stool culture (IRR 0.664, 95% CI 0.526–0.840, P < 0.001). Appropriate antibiotic use occurred in 59.5% of PCR patients versus 21.4% of those with stool culture alone (OR 5.38, 95% CI 3.26–8.89, P < 0.001). Median antibiotic duration was similar across groups. Colonoscopy was rare (2.0%) and did not differ by test type.
Discussion: This study showed that utilizing GI PCR panels for hospitalized patients with suspected infectious gastroenteritis reduced hospital stays and dramatically improved antibiotic prescribing. Patients screened with PCR had more than 30% shorter stays and were five times more likely to receive adequate antibiotics than those tested with stool culture. PCR produced faster results, allowing for early, focused treatment. Patients who received both PCR and culture did not see the similar LOS reduction, emphasizing the need of early PCR-driven decisions. While antibiotic duration was comparable between groups, PCR resulted in more appropriate and individualized use, without increasing overall exposure. Colonoscopy rates were found to be low and did not differ according to the type of test performed. The study's limitations encompass its retrospective design, potential selection bias, a single-center context, and the unmeasured effects of costs.
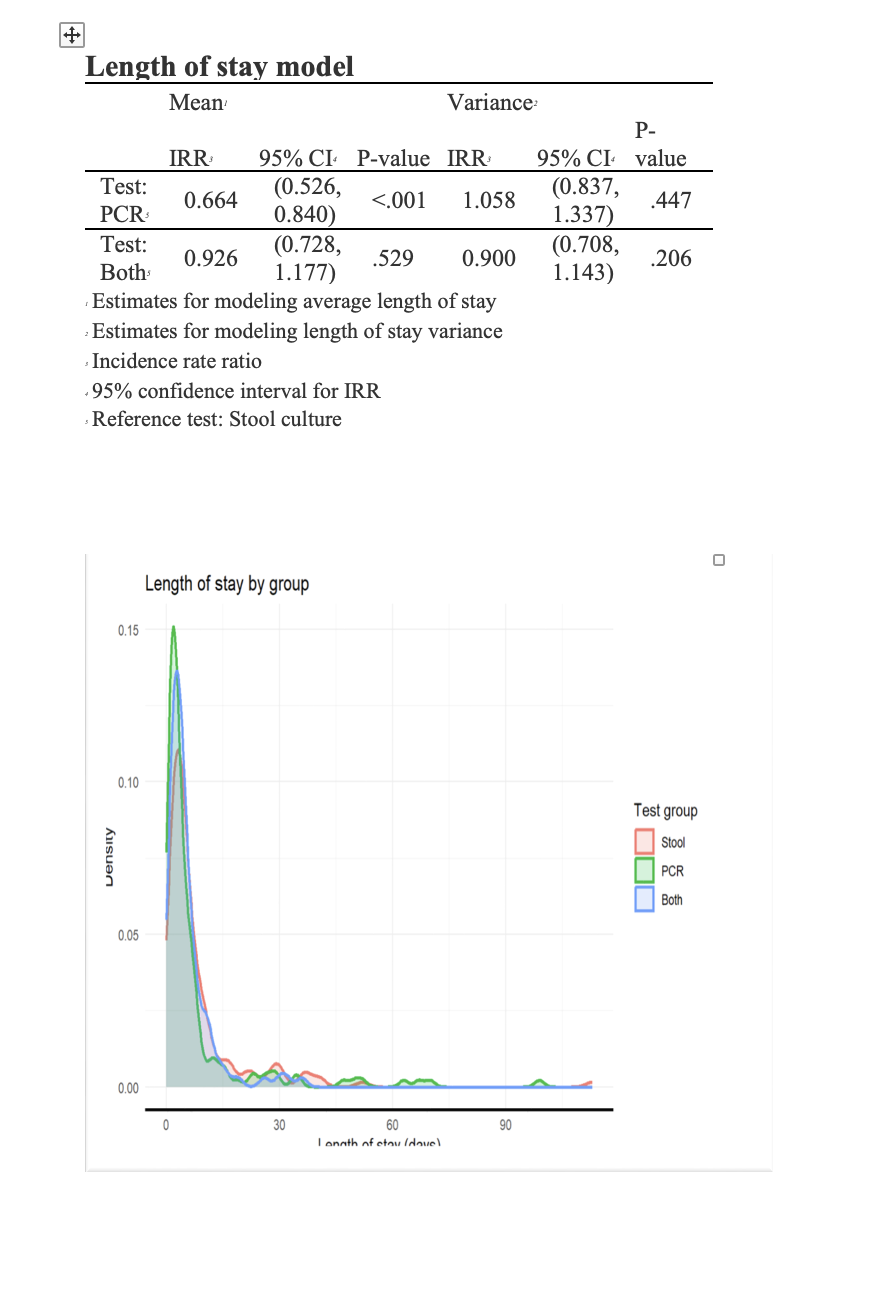
Figure: Length of Stay Model
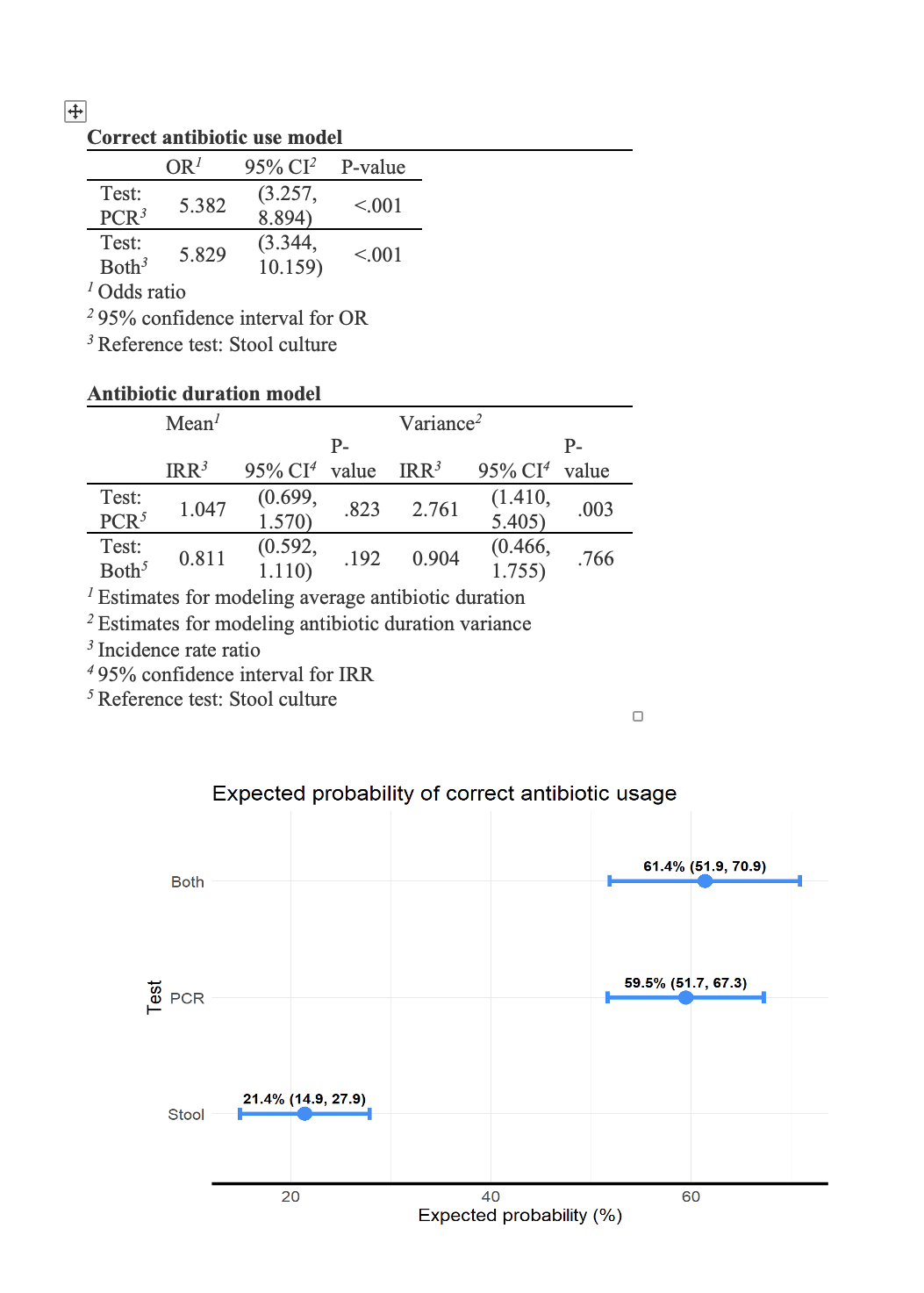
Figure: Antibiotics Use Model
Disclosures:
Bolaji Ayinde indicated no relevant financial relationships.
Mena Louis indicated no relevant financial relationships.
Adeel Akhtar indicated no relevant financial relationships.
Ana Tucker indicated no relevant financial relationships.
Jake Slaton indicated no relevant financial relationships.
Phillip Gross indicated no relevant financial relationships.
Bolaji O. Ayinde, MD1, Mena Louis, DO2, Adeel Akhtar, MD1, Ana Tucker, PhD1, Jake Slaton, MS3, Phillip J. Gross, MD, MPH4. P1307 - Impact of GI PCR versus Stool Culture on Clinical Outcomes in Hospitalized Patients: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
