Sunday Poster Session
Category: IBD
P1267 - Crohn's in Crisis: A Multi-Modal Approach to Abscess Management
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KM
Kranthi Mandava, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Kranthi Mandava, MD1, Charmi Patel, MD1, Ethan Shamsian, DO1, Michael Bebawy, DO1, Rohan Karkra, MBBS1, Anmol Mittal, MD1, Sima Vossough-Teehan, MD2
1Rutgers New Jersey Medical School, Newark, NJ; 2East Orange VA Hospital, East Orange, NJ
Introduction: Crohn’s disease (CD) is a chronic inflammatory disorder marked by transmural inflammation and skip lesions, often resulting in complications such as strictures, fistulas, and abscesses. Intra-abdominal or perianal abscesses complicate management, requiring a balance between infection control and inflammation control. ACG guidelines recommend prioritizing infection management and delaying biologics during active abscesses. However, limited guidance exists for managing non-drainable abscesses in patients with worsening symptoms. We report a case of CD complicated by a non-drainable intra-abdominal abscess in which biologic therapy was initiated due to disease progression.
Case Description/
Methods: A 27-year-old male with CD (diagnosed 2017) and prior small bowel perforations requiring ileostomy and reversal (2018) presented with 3 weeks of worsening abdominal pain, nausea, and vomiting. He was hospitalized one week prior for a 2.9 cm mesenteric abscess, which was managed conservatively due to its location. Upon re-presentation, he could not tolerate oral antibiotics, with worsening symptoms but no fever or GI bleeding. Labs showed leukocytosis, thrombocytosis, and elevated ESR/CRP. Repeat CT revealed interval growth of the abscess (now 4.1 cm), thickened ileal loops, and a new nonobstructive portal vein thrombus resulting from his pro-inflammatory state. IR again deferred drainage; surgery recommended non-operative management. He was started on IV piperacillin-tazobactam and therapeutic heparin. By day 6, CT showed a reduction in abscess size. Given a CDAI of 256.9, infliximab was initiated on day 7 without complications. He was discharged on IV antibiotics and started on mercaptopurine and apixaban. At follow-up, he reported mild abdominal pain without recurrence of his initial symptoms and continued to tolerate infliximab therapy.
Discussion: We present a case of a patient with moderate to severe CD who underwent biologic therapy induction in the setting of a non-drainable intra-abdominal abscess, with improvement in CD symptoms. Despite current guidelines advising resolution of abscesses prior to starting biologics, initiating anti-TNF therapy during ongoing symptoms was effective in mitigating disease burden. Existing literature evaluating the concurrent usage of anti-TNF and antibiotic therapy suggests that this may be a safe and effective strategy, and future studies are warranted to further investigate these findings so that guidelines may be adjusted accordingly.
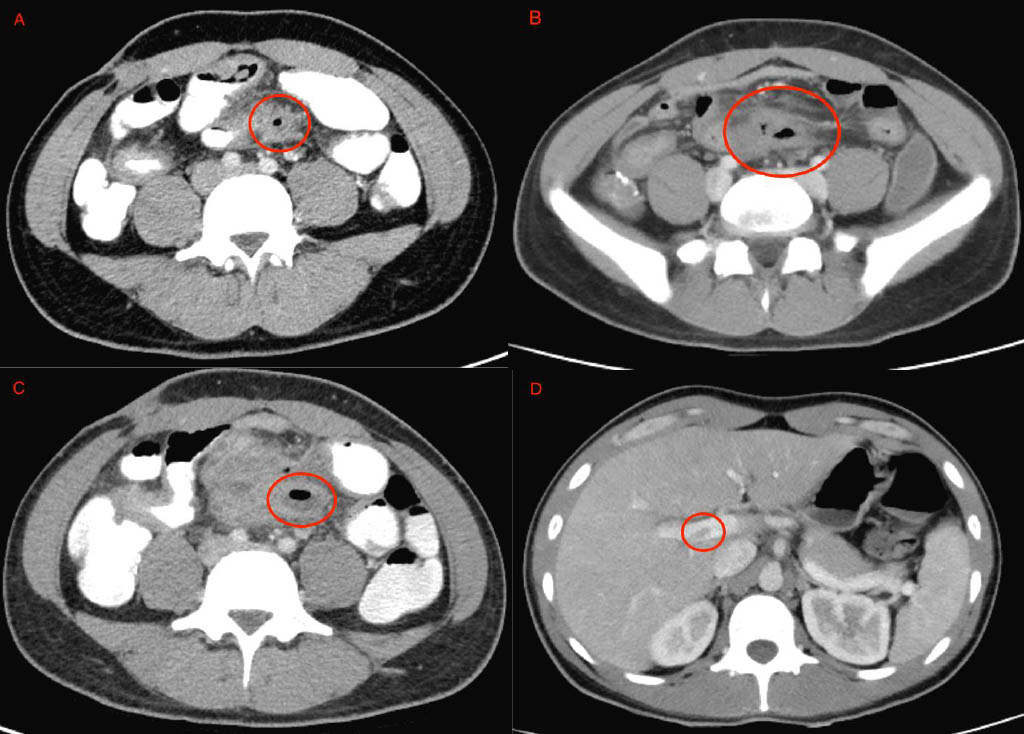
Figure: Evolution of patient's non-drainable intra-abdominal abscess. Figures A - C showcase patient's abscess on initial presentation, subsequent presentation and after IV antibiotics were initiated. Figure D shows new non-obstructive portal vein thrombus.
Disclosures:
Kranthi Mandava indicated no relevant financial relationships.
Charmi Patel indicated no relevant financial relationships.
Ethan Shamsian indicated no relevant financial relationships.
Michael Bebawy indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Anmol Mittal indicated no relevant financial relationships.
Sima Vossough-Teehan indicated no relevant financial relationships.
Kranthi Mandava, MD1, Charmi Patel, MD1, Ethan Shamsian, DO1, Michael Bebawy, DO1, Rohan Karkra, MBBS1, Anmol Mittal, MD1, Sima Vossough-Teehan, MD2. P1267 - Crohn's in Crisis: A Multi-Modal Approach to Abscess Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2East Orange VA Hospital, East Orange, NJ
Introduction: Crohn’s disease (CD) is a chronic inflammatory disorder marked by transmural inflammation and skip lesions, often resulting in complications such as strictures, fistulas, and abscesses. Intra-abdominal or perianal abscesses complicate management, requiring a balance between infection control and inflammation control. ACG guidelines recommend prioritizing infection management and delaying biologics during active abscesses. However, limited guidance exists for managing non-drainable abscesses in patients with worsening symptoms. We report a case of CD complicated by a non-drainable intra-abdominal abscess in which biologic therapy was initiated due to disease progression.
Case Description/
Methods: A 27-year-old male with CD (diagnosed 2017) and prior small bowel perforations requiring ileostomy and reversal (2018) presented with 3 weeks of worsening abdominal pain, nausea, and vomiting. He was hospitalized one week prior for a 2.9 cm mesenteric abscess, which was managed conservatively due to its location. Upon re-presentation, he could not tolerate oral antibiotics, with worsening symptoms but no fever or GI bleeding. Labs showed leukocytosis, thrombocytosis, and elevated ESR/CRP. Repeat CT revealed interval growth of the abscess (now 4.1 cm), thickened ileal loops, and a new nonobstructive portal vein thrombus resulting from his pro-inflammatory state. IR again deferred drainage; surgery recommended non-operative management. He was started on IV piperacillin-tazobactam and therapeutic heparin. By day 6, CT showed a reduction in abscess size. Given a CDAI of 256.9, infliximab was initiated on day 7 without complications. He was discharged on IV antibiotics and started on mercaptopurine and apixaban. At follow-up, he reported mild abdominal pain without recurrence of his initial symptoms and continued to tolerate infliximab therapy.
Discussion: We present a case of a patient with moderate to severe CD who underwent biologic therapy induction in the setting of a non-drainable intra-abdominal abscess, with improvement in CD symptoms. Despite current guidelines advising resolution of abscesses prior to starting biologics, initiating anti-TNF therapy during ongoing symptoms was effective in mitigating disease burden. Existing literature evaluating the concurrent usage of anti-TNF and antibiotic therapy suggests that this may be a safe and effective strategy, and future studies are warranted to further investigate these findings so that guidelines may be adjusted accordingly.
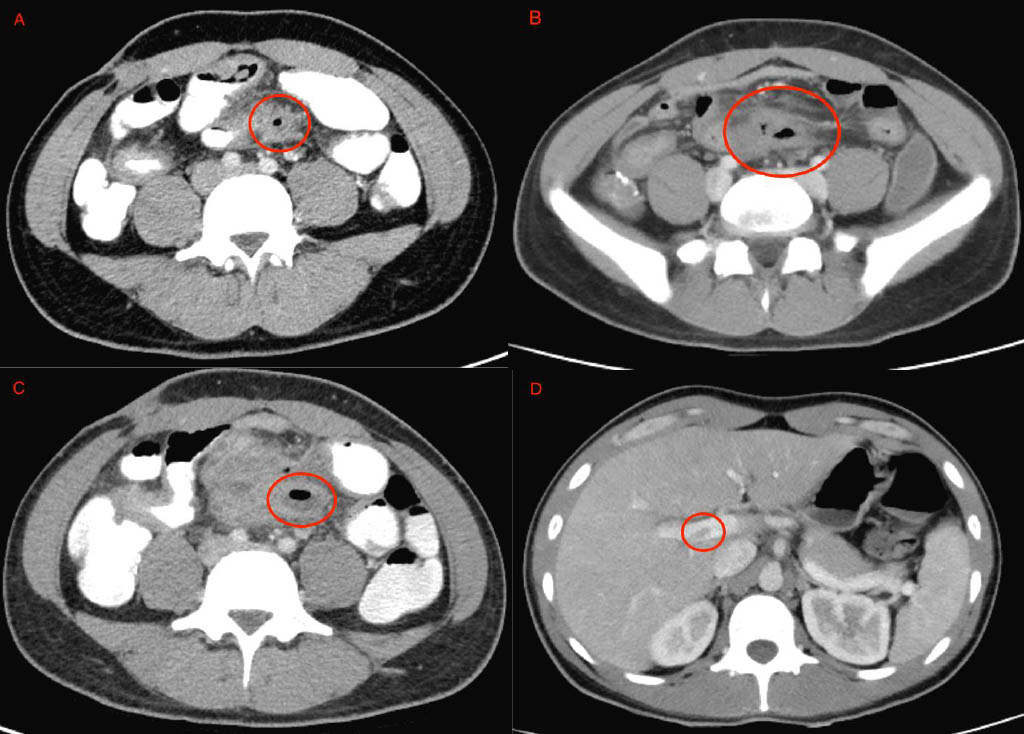
Figure: Evolution of patient's non-drainable intra-abdominal abscess. Figures A - C showcase patient's abscess on initial presentation, subsequent presentation and after IV antibiotics were initiated. Figure D shows new non-obstructive portal vein thrombus.
Disclosures:
Kranthi Mandava indicated no relevant financial relationships.
Charmi Patel indicated no relevant financial relationships.
Ethan Shamsian indicated no relevant financial relationships.
Michael Bebawy indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Anmol Mittal indicated no relevant financial relationships.
Sima Vossough-Teehan indicated no relevant financial relationships.
Kranthi Mandava, MD1, Charmi Patel, MD1, Ethan Shamsian, DO1, Michael Bebawy, DO1, Rohan Karkra, MBBS1, Anmol Mittal, MD1, Sima Vossough-Teehan, MD2. P1267 - Crohn's in Crisis: A Multi-Modal Approach to Abscess Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
