Sunday Poster Session
Category: IBD
P1233 - Mesalamine-Induced Pancreatitis: A Rare Complication in the Treatment of Ulcerative Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Sam Papasotiriou, DO
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Sam Papasotiriou, DO1, James S. Love, MD1, Mario Tavakoli, DO1, Itishree Trivedi, MD2
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL
Introduction: Mesalamines are a first-line therapy in management mild-to-moderate ulcerative colitis (UC). While generally well tolerated, rare and serious adverse events, including acute pancreatitis, have been reported. Diagnosing mesalamine-induced pancreatitis is challenging, particularly in a newly diagnosed UC patient, where disease-related symptoms and other causes of pancreatitis (such as autoimmune pancreatitis) may cloud the picture. Early recognition is critical to prevent recurrence and guide appropriate therapy.
Case Description/
Methods: A 35-year-old man with no medical history presented with abdominal pain and hematochezia. Colonoscopy revealed pancolitis consistent with mild-to-moderate UC (Mayo score: 2), confirmed on biopsy. He was started on oral mesalamine (4.8 g/day) and mesalamine enemas. Two weeks later, he returned with persistent bloody diarrhea and abdominal pain, with an additional complaint of epigastric pain radiating to the back. Labs showed elevated CRP (8.9 mg/L) and lipase 171 U/L . Liver enzymes were normal. Imaging demonstrated peripancreatic fat stranding, consistent with acute pancreatitis, and diffuse colonic wall thickening. Abdominal ultrasound showed no gallstones or biliary pathology.
He was managed supportively with IV fluids and bowel rest. Due to ongoing hematochezia and elevated inflammatory markers, IV methylprednisolone was started for management of UC. Flexible sigmoidoscopy confirmed active colitis. Within 48 hours, he improved with resolution of bleeding and decreased stool frequency. CRP trended down to 8.6 mg/L. He was discharged on a prednisone taper and transitioned to azathioprine and adalimumab for maintenance. On follow-up visit in 6 weeks, patient was in clinical remission from a UC perspective.
Discussion: Mesalamine is linked to both paradoxical UC worsening (up to 6.2%) and drug-induced pancreatitis (up to 1.8%), typically within the first weeks of treatment. The pathogenesis remains unclear but is hypothesized to involve either a hypersensitivity reaction or direct toxic injury to pancreatic acinar cells. Mesalamine-induced pancreatitis is often mild and self-limited upon discontinuation, however, re-challenge typically results in rapid recurrence. Severe or fulminant pancreatitis has been described in isolated reports with mortality occurring in cases of delayed recognition. This case highlights the need for vigilance regarding mesalamine-related adverse effects in patients presenting with new or worsening symptoms after therapy initiation.
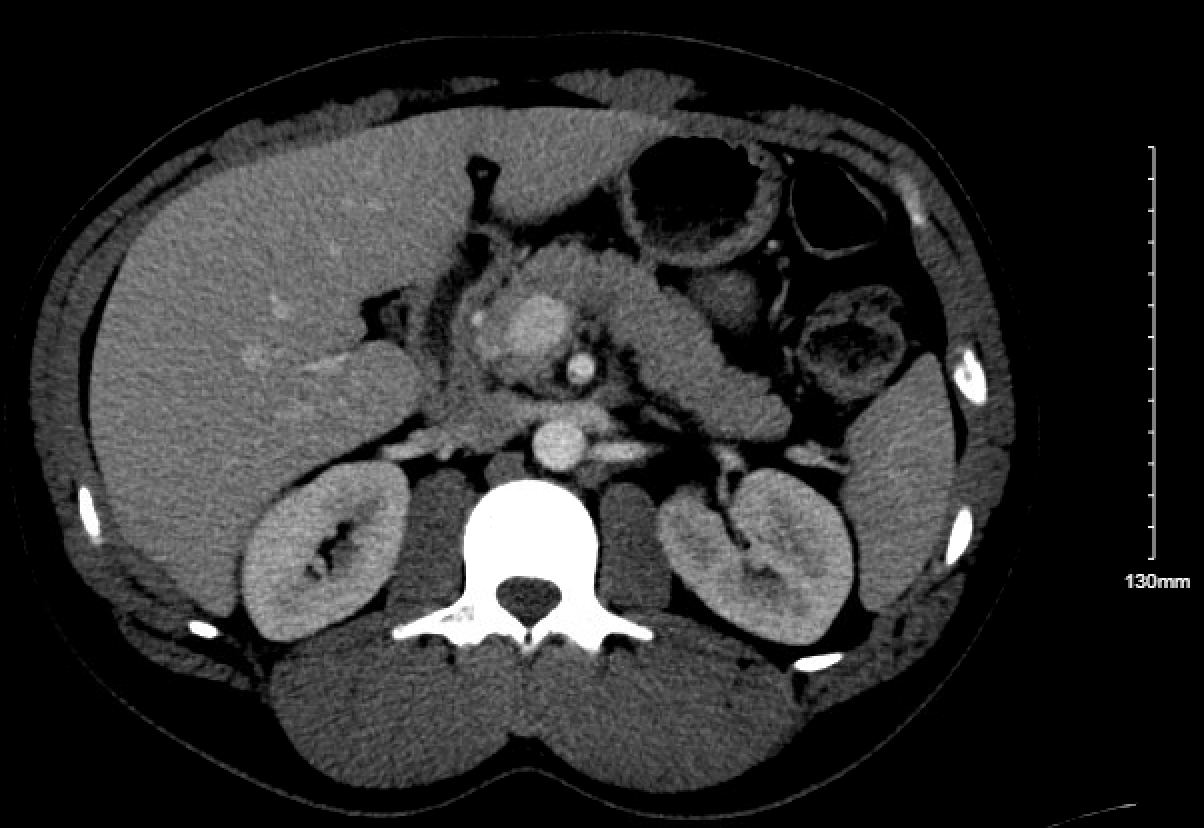
Figure: CT A/P

Figure: Inflammation of Sigmoid Colon
Disclosures:
Sam Papasotiriou indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Mario Tavakoli indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Sam Papasotiriou, DO1, James S. Love, MD1, Mario Tavakoli, DO1, Itishree Trivedi, MD2. P1233 - Mesalamine-Induced Pancreatitis: A Rare Complication in the Treatment of Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL
Introduction: Mesalamines are a first-line therapy in management mild-to-moderate ulcerative colitis (UC). While generally well tolerated, rare and serious adverse events, including acute pancreatitis, have been reported. Diagnosing mesalamine-induced pancreatitis is challenging, particularly in a newly diagnosed UC patient, where disease-related symptoms and other causes of pancreatitis (such as autoimmune pancreatitis) may cloud the picture. Early recognition is critical to prevent recurrence and guide appropriate therapy.
Case Description/
Methods: A 35-year-old man with no medical history presented with abdominal pain and hematochezia. Colonoscopy revealed pancolitis consistent with mild-to-moderate UC (Mayo score: 2), confirmed on biopsy. He was started on oral mesalamine (4.8 g/day) and mesalamine enemas. Two weeks later, he returned with persistent bloody diarrhea and abdominal pain, with an additional complaint of epigastric pain radiating to the back. Labs showed elevated CRP (8.9 mg/L) and lipase 171 U/L . Liver enzymes were normal. Imaging demonstrated peripancreatic fat stranding, consistent with acute pancreatitis, and diffuse colonic wall thickening. Abdominal ultrasound showed no gallstones or biliary pathology.
He was managed supportively with IV fluids and bowel rest. Due to ongoing hematochezia and elevated inflammatory markers, IV methylprednisolone was started for management of UC. Flexible sigmoidoscopy confirmed active colitis. Within 48 hours, he improved with resolution of bleeding and decreased stool frequency. CRP trended down to 8.6 mg/L. He was discharged on a prednisone taper and transitioned to azathioprine and adalimumab for maintenance. On follow-up visit in 6 weeks, patient was in clinical remission from a UC perspective.
Discussion: Mesalamine is linked to both paradoxical UC worsening (up to 6.2%) and drug-induced pancreatitis (up to 1.8%), typically within the first weeks of treatment. The pathogenesis remains unclear but is hypothesized to involve either a hypersensitivity reaction or direct toxic injury to pancreatic acinar cells. Mesalamine-induced pancreatitis is often mild and self-limited upon discontinuation, however, re-challenge typically results in rapid recurrence. Severe or fulminant pancreatitis has been described in isolated reports with mortality occurring in cases of delayed recognition. This case highlights the need for vigilance regarding mesalamine-related adverse effects in patients presenting with new or worsening symptoms after therapy initiation.
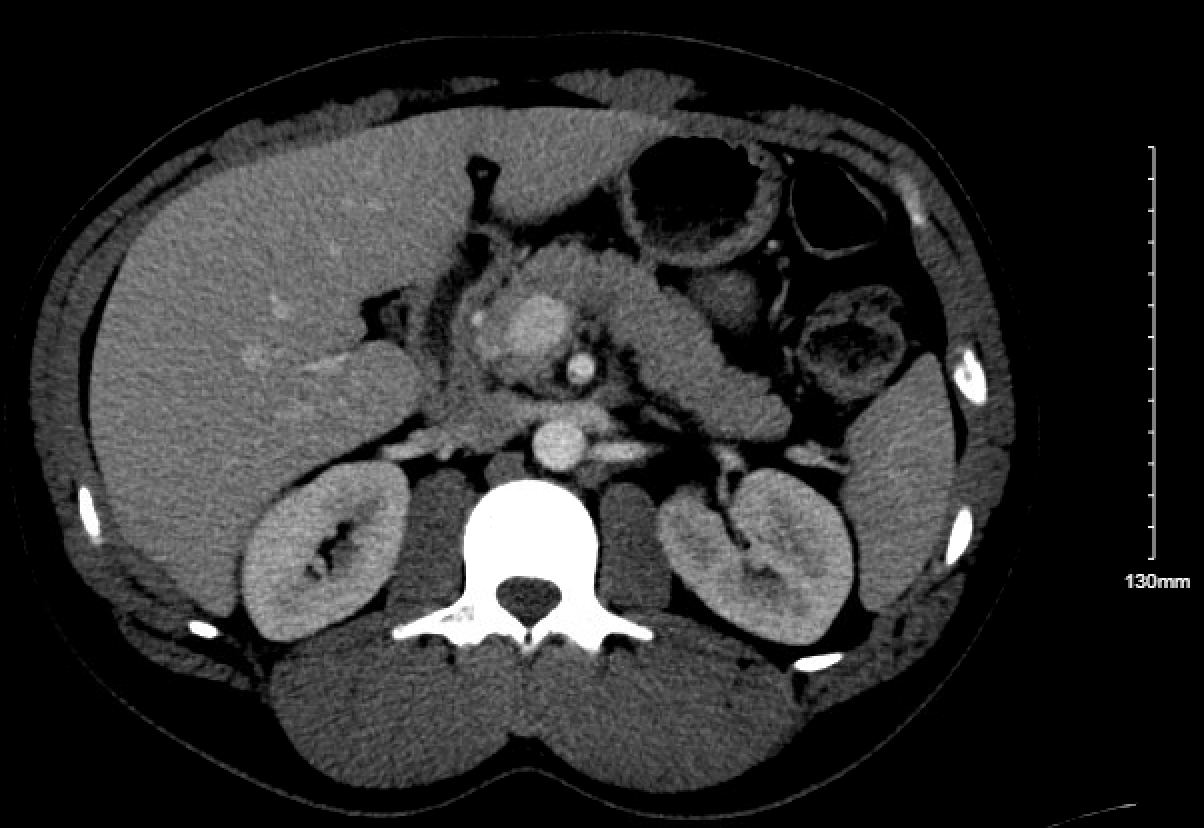
Figure: CT A/P

Figure: Inflammation of Sigmoid Colon
Disclosures:
Sam Papasotiriou indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Mario Tavakoli indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Sam Papasotiriou, DO1, James S. Love, MD1, Mario Tavakoli, DO1, Itishree Trivedi, MD2. P1233 - Mesalamine-Induced Pancreatitis: A Rare Complication in the Treatment of Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

