Sunday Poster Session
Category: IBD
P1230 - The Unseen Culprit: Chronic Lymphocytic Leukemia as a Driver of Refractory Ulcerative Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- RS
Raj Shah, MD
Orlando VA Medical Center and UCF/HCA Greater Orlando
Kissimmee, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Raj Shah, MD1, Antonio Hernandez, MD2, Juan Oharriz, MD2
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 2Orlando VA Healthcare System, Orlando, FL
Introduction: Ulcerative colitis (UC) is an inflammatory bowel disease that primarily causes diffuse mucosal inflammation in the rectum and colon. Compared to those without UC, patients with UC have a higher incidence of hematologic malignancies, including leukemia. We present a rare case of refractory UC due to infiltration by Chronic Lymphocytic Leukemia (CLL).
Case Description/
Methods: A 60-year-old male with a history of UC and stage 0 CLL under observation presented with abdominal pain and worsening bloody diarrhea with more than 10 episodes per day. Previous UC treatments included prednisone, mesalamine, Infliximab, and Upadacitinib. Steroids were started for UC flare. Colonoscopy revealed pan-colitis with biopsy negative for Cytomegalovirus and CLL infiltration. He was started on Vedolizumab, and discharged home after improvement.
3 months later, he was readmitted for another flare-up. Colonoscopy showed severe pancolitis (Mayo Score 3), worse than the previous exam. (Fig. 1) Biopsy confirmed CLL infiltration with cells positive for CD20 but negative for CD10 or significant BCL6 to suggest Richter’s Transformation. (Fig. 2) Patient was again treated with steroids and changed to Ustekinumab, with partial improvement. Given refractory UC with CLL infiltration, oncology began treatment for CLL. At the 3-month follow-up, he exhibited significant improvement.
Discussion: CLL infiltration in the GI tract is rare and typically occurs after transforming to diffuse large B-cell lymphoma (Richter syndrome). However, in this case, infiltration was present at stage 0 without transformation. Non-responsiveness to several biologics raised suspicion of an underlying CLL infiltration. Despite the initial negative biopsy, biopsy was repeated to further investigate for CLL. At each instance we specially requested our pathologist to stain for CLL infiltration. Given the unusual combination of UC and CLL infiltration in the GI tract, there are currently no established guidelines for their management. Although the patient was initially under observation for CLL, the persistent nature of the symptoms prompted us to pursue concurrent treatment, which resulted in significant improvement. In conclusion, this case underlines the necessity of maintaining a high suspicion of CLL infiltration, even in patients with stage 0 as a potential cause of refractory UC. Close communication with pathologists and repeat biopsies may be crucial for confirmation.
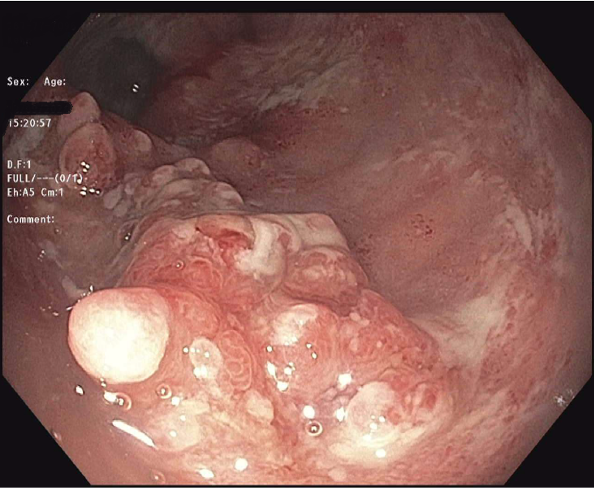
Figure: Colonoscopy showing severe inflammation in the rectum with nodular appearing mucosa.

Figure: Rectum Biopsy showing CD20+ B-CLL cells in the mucosa wall
Disclosures:
Raj Shah indicated no relevant financial relationships.
Antonio Hernandez indicated no relevant financial relationships.
Juan Oharriz indicated no relevant financial relationships.
Raj Shah, MD1, Antonio Hernandez, MD2, Juan Oharriz, MD2. P1230 - The Unseen Culprit: Chronic Lymphocytic Leukemia as a Driver of Refractory Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Raj Shah, MD1, Antonio Hernandez, MD2, Juan Oharriz, MD2
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 2Orlando VA Healthcare System, Orlando, FL
Introduction: Ulcerative colitis (UC) is an inflammatory bowel disease that primarily causes diffuse mucosal inflammation in the rectum and colon. Compared to those without UC, patients with UC have a higher incidence of hematologic malignancies, including leukemia. We present a rare case of refractory UC due to infiltration by Chronic Lymphocytic Leukemia (CLL).
Case Description/
Methods: A 60-year-old male with a history of UC and stage 0 CLL under observation presented with abdominal pain and worsening bloody diarrhea with more than 10 episodes per day. Previous UC treatments included prednisone, mesalamine, Infliximab, and Upadacitinib. Steroids were started for UC flare. Colonoscopy revealed pan-colitis with biopsy negative for Cytomegalovirus and CLL infiltration. He was started on Vedolizumab, and discharged home after improvement.
3 months later, he was readmitted for another flare-up. Colonoscopy showed severe pancolitis (Mayo Score 3), worse than the previous exam. (Fig. 1) Biopsy confirmed CLL infiltration with cells positive for CD20 but negative for CD10 or significant BCL6 to suggest Richter’s Transformation. (Fig. 2) Patient was again treated with steroids and changed to Ustekinumab, with partial improvement. Given refractory UC with CLL infiltration, oncology began treatment for CLL. At the 3-month follow-up, he exhibited significant improvement.
Discussion: CLL infiltration in the GI tract is rare and typically occurs after transforming to diffuse large B-cell lymphoma (Richter syndrome). However, in this case, infiltration was present at stage 0 without transformation. Non-responsiveness to several biologics raised suspicion of an underlying CLL infiltration. Despite the initial negative biopsy, biopsy was repeated to further investigate for CLL. At each instance we specially requested our pathologist to stain for CLL infiltration. Given the unusual combination of UC and CLL infiltration in the GI tract, there are currently no established guidelines for their management. Although the patient was initially under observation for CLL, the persistent nature of the symptoms prompted us to pursue concurrent treatment, which resulted in significant improvement. In conclusion, this case underlines the necessity of maintaining a high suspicion of CLL infiltration, even in patients with stage 0 as a potential cause of refractory UC. Close communication with pathologists and repeat biopsies may be crucial for confirmation.
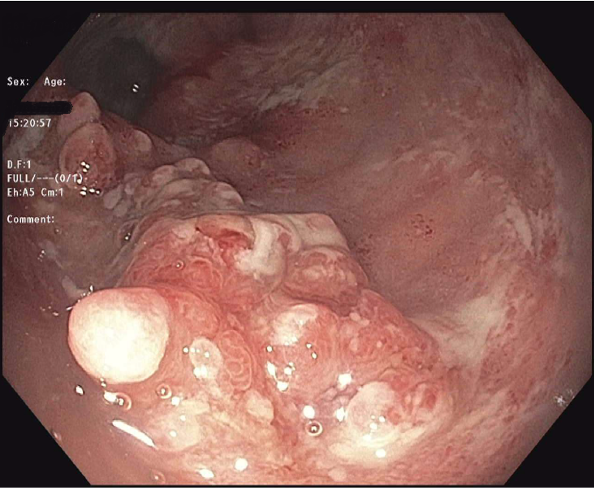
Figure: Colonoscopy showing severe inflammation in the rectum with nodular appearing mucosa.

Figure: Rectum Biopsy showing CD20+ B-CLL cells in the mucosa wall
Disclosures:
Raj Shah indicated no relevant financial relationships.
Antonio Hernandez indicated no relevant financial relationships.
Juan Oharriz indicated no relevant financial relationships.
Raj Shah, MD1, Antonio Hernandez, MD2, Juan Oharriz, MD2. P1230 - The Unseen Culprit: Chronic Lymphocytic Leukemia as a Driver of Refractory Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

