Sunday Poster Session
Category: IBD
P1213 - Two Decades of Inflammatory Bowel Disease-Related Cardiovascular Mortality in the United States: Temporal Trends and Demographic Disparities From a National Death Registry
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Ahmed Abuhasna, DO
Advocate Illinois Masonic Medical Center
Chicago, IL
Presenting Author(s)
Ahmed Abuhasna, DO1, Abdalhakim Shubietah, MD1, Islam Rajab, MD2, Mohammad Ghannam, MD3, Abdallah Hussein, MD4, Hamid U.. Rahman, MD1, Mohamed S. Elgendy, MBBCh5, Emmanuel Olumuyide, MD1, Ameer Awashra, MD6, Hosam I. Taha, MBBCh5, Qutaiba Qafisheh, MD7, Mohammad Alqadi, MD7, Mohammad O. Abdelhafez, MD8, Muath A. Baniowda, MD9
1Advocate Illinois Masonic Medical Center, Chicago, IL; 2St. Joseph's University Medical Center, Paterson, NJ; 3Brookdale University Hospital Medical Center, New York, NY; 4Virtua Our Lady of Lourdes Hospital, Camden, NJ; 5Tanta University, Tanta, Al Gharbiyah, Egypt; 6An-Najah National University, Nablus, Palestinian Territories; 7University of Toledo, Toledo, OH; 8Al-Quds University, Jerusalem, Palestinian Territories; 9University of Missouri Kansas City School of Medicine, Kansas City, MO
Introduction: Despite well-documented links between IBD and cardiovascular events, long-term, population-level mortality trends in this group remain unexplored. Therefore, we undertook the first comprehensive two-decade U.S. analysis of IBD-associated cardiovascular deaths to characterize temporal shifts and uncover demographic and geographic disparities in this high-risk population.
Methods: We retrospectively analyzed CDC WONDER data (1999–2020) for decedents with CVD (ICD‑10 I00–I99) and contributory IBD (K50/K51), calculating age‑adjusted mortality rates (AAMRs; direct method, 11 strata; 2000 standard) and crude mortality rates per 100,000. Rates were stratified by year, sex, race/Hispanic origin, age, state, place of death, and 2013 NCHS urbanization level; cells with < 20 deaths were suppressed per CDC guidelines.
Results: Between 1999 and 2020, 11,891 IBD-associated cardiovascular deaths occurred. Overall, mortality declined by –2.74% per year from 1999–2015 (95% CI –4.49 to –2.04; p = 0.0064) before a nonsignificant rebound of +3.85% from 2015–2020 (95% CI –0.24 to +13.86; p = 0.0656). Females saw a –2.99% decline (1999–2013; p = 0.0296) then plateaued (+1.76% through 2020; p = 0.3379), while males declined –3.07% (1999–2018; p = 0.0024) then rose +27.19% (2018–2020; p = 0.0100). White and Black individuals showed parallel trends: White APC –2.81% (1999–2014; p = 0.0004) then +3.12% (2014–2020; p = 0.0352); Black APC –2.82% (1999–2017; p = 0.0332) then +23.03% (2017–2020; p = 0.0416). AAMRs were highest in White (0.1672) and lowest in Asian/Pacific Islander (0.0280) populations; non‐Hispanics exceeded Hispanics (0.1657 vs 0.0385). State-level AAMRs ranged from 0.0684 in Louisiana to 0.2866 in Oregon, and urbanization-specific rates ranged from 0.1454 in large central metros to 0.1719 in small metro areas. Most deaths occurred at home (n = 3,727) or inpatient (n = 3,682), with crude mortality rising from 0.0037 (ages 15–24) to 2.72 (≥ 85 years).
Discussion: Analysis of U.S. mortality data demonstrated a marked reduction in IBD-associated cardiovascular deaths from 1999 to 2015, followed by stabilization and a modest rebound through 2020. The disproportionate resurgence among men and Black patients underscores persistent gaps in risk mitigation and management. These findings call for individualized, multidisciplinary preventive interventions and continuous cardiovascular surveillance throughout the IBD care continuum.
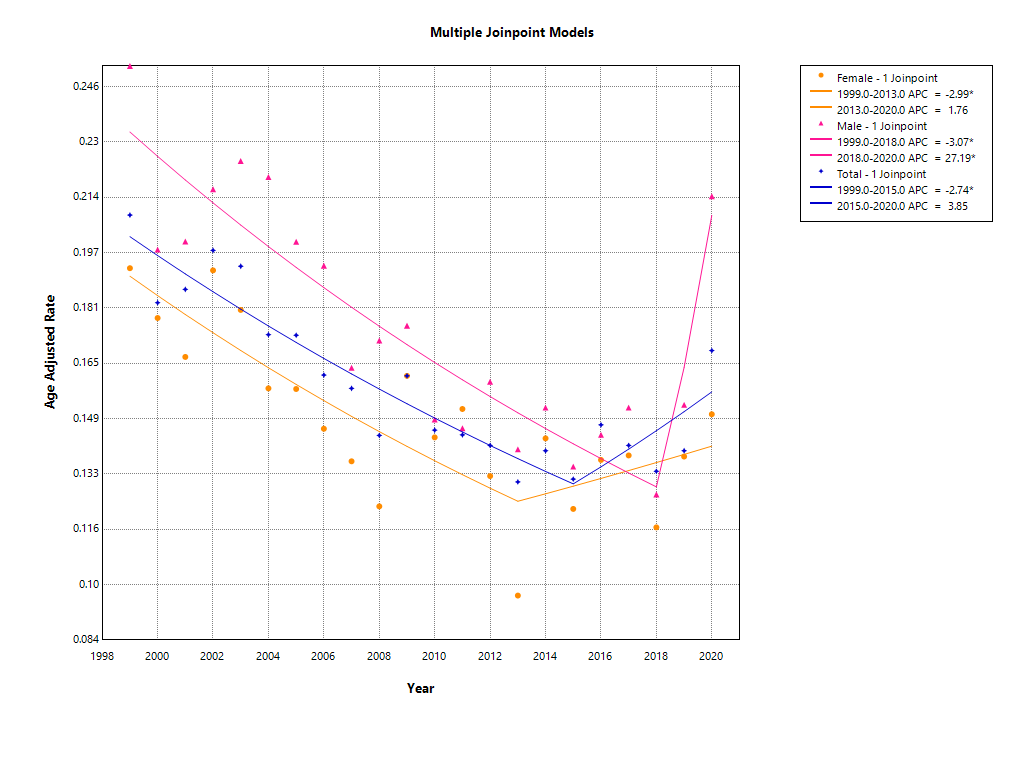
Figure: Figure 1. Age-adjusted cardiovascular mortality rates per 100,000 among U.S. decedents with IBD, 1999–2020, stratified by sex and overall cohort.
Disclosures:
Ahmed Abuhasna indicated no relevant financial relationships.
Abdalhakim Shubietah indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Mohammad Ghannam indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Hamid Rahman indicated no relevant financial relationships.
Mohamed S. Elgendy indicated no relevant financial relationships.
Emmanuel Olumuyide indicated no relevant financial relationships.
Ameer Awashra indicated no relevant financial relationships.
Hosam I. Taha indicated no relevant financial relationships.
Qutaiba Qafisheh indicated no relevant financial relationships.
Mohammad Alqadi indicated no relevant financial relationships.
Mohammad O. Abdelhafez indicated no relevant financial relationships.
Muath A. Baniowda indicated no relevant financial relationships.
Ahmed Abuhasna, DO1, Abdalhakim Shubietah, MD1, Islam Rajab, MD2, Mohammad Ghannam, MD3, Abdallah Hussein, MD4, Hamid U.. Rahman, MD1, Mohamed S. Elgendy, MBBCh5, Emmanuel Olumuyide, MD1, Ameer Awashra, MD6, Hosam I. Taha, MBBCh5, Qutaiba Qafisheh, MD7, Mohammad Alqadi, MD7, Mohammad O. Abdelhafez, MD8, Muath A. Baniowda, MD9. P1213 - Two Decades of Inflammatory Bowel Disease-Related Cardiovascular Mortality in the United States: Temporal Trends and Demographic Disparities From a National Death Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Advocate Illinois Masonic Medical Center, Chicago, IL; 2St. Joseph's University Medical Center, Paterson, NJ; 3Brookdale University Hospital Medical Center, New York, NY; 4Virtua Our Lady of Lourdes Hospital, Camden, NJ; 5Tanta University, Tanta, Al Gharbiyah, Egypt; 6An-Najah National University, Nablus, Palestinian Territories; 7University of Toledo, Toledo, OH; 8Al-Quds University, Jerusalem, Palestinian Territories; 9University of Missouri Kansas City School of Medicine, Kansas City, MO
Introduction: Despite well-documented links between IBD and cardiovascular events, long-term, population-level mortality trends in this group remain unexplored. Therefore, we undertook the first comprehensive two-decade U.S. analysis of IBD-associated cardiovascular deaths to characterize temporal shifts and uncover demographic and geographic disparities in this high-risk population.
Methods: We retrospectively analyzed CDC WONDER data (1999–2020) for decedents with CVD (ICD‑10 I00–I99) and contributory IBD (K50/K51), calculating age‑adjusted mortality rates (AAMRs; direct method, 11 strata; 2000 standard) and crude mortality rates per 100,000. Rates were stratified by year, sex, race/Hispanic origin, age, state, place of death, and 2013 NCHS urbanization level; cells with < 20 deaths were suppressed per CDC guidelines.
Results: Between 1999 and 2020, 11,891 IBD-associated cardiovascular deaths occurred. Overall, mortality declined by –2.74% per year from 1999–2015 (95% CI –4.49 to –2.04; p = 0.0064) before a nonsignificant rebound of +3.85% from 2015–2020 (95% CI –0.24 to +13.86; p = 0.0656). Females saw a –2.99% decline (1999–2013; p = 0.0296) then plateaued (+1.76% through 2020; p = 0.3379), while males declined –3.07% (1999–2018; p = 0.0024) then rose +27.19% (2018–2020; p = 0.0100). White and Black individuals showed parallel trends: White APC –2.81% (1999–2014; p = 0.0004) then +3.12% (2014–2020; p = 0.0352); Black APC –2.82% (1999–2017; p = 0.0332) then +23.03% (2017–2020; p = 0.0416). AAMRs were highest in White (0.1672) and lowest in Asian/Pacific Islander (0.0280) populations; non‐Hispanics exceeded Hispanics (0.1657 vs 0.0385). State-level AAMRs ranged from 0.0684 in Louisiana to 0.2866 in Oregon, and urbanization-specific rates ranged from 0.1454 in large central metros to 0.1719 in small metro areas. Most deaths occurred at home (n = 3,727) or inpatient (n = 3,682), with crude mortality rising from 0.0037 (ages 15–24) to 2.72 (≥ 85 years).
Discussion: Analysis of U.S. mortality data demonstrated a marked reduction in IBD-associated cardiovascular deaths from 1999 to 2015, followed by stabilization and a modest rebound through 2020. The disproportionate resurgence among men and Black patients underscores persistent gaps in risk mitigation and management. These findings call for individualized, multidisciplinary preventive interventions and continuous cardiovascular surveillance throughout the IBD care continuum.
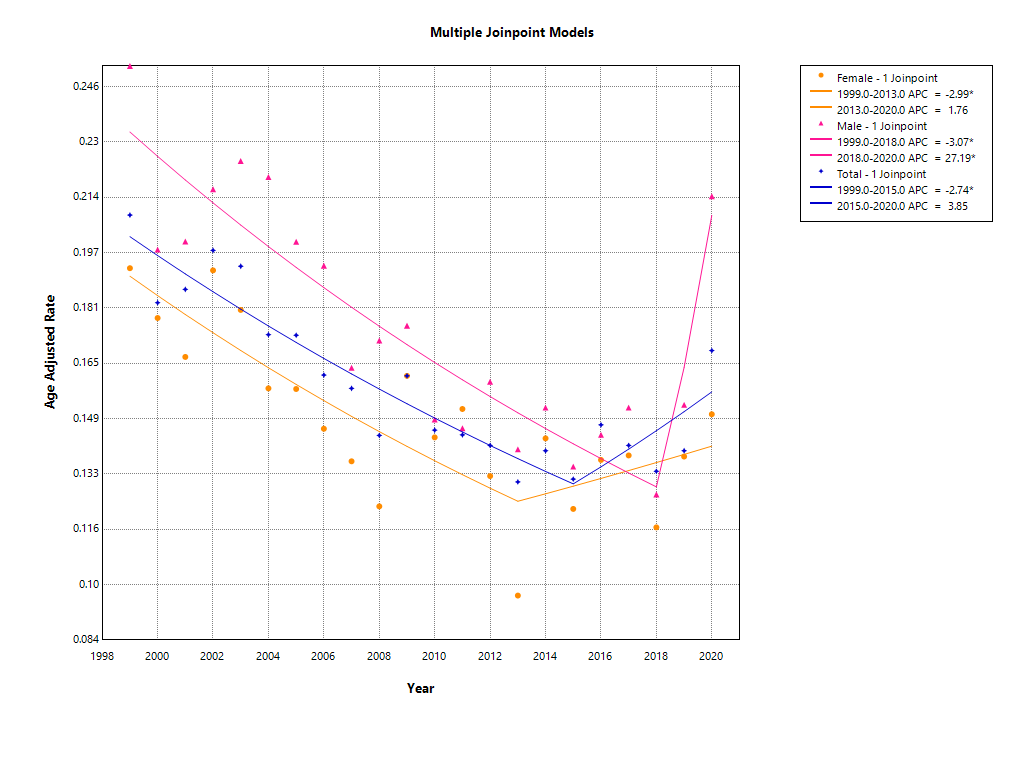
Figure: Figure 1. Age-adjusted cardiovascular mortality rates per 100,000 among U.S. decedents with IBD, 1999–2020, stratified by sex and overall cohort.
Disclosures:
Ahmed Abuhasna indicated no relevant financial relationships.
Abdalhakim Shubietah indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Mohammad Ghannam indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Hamid Rahman indicated no relevant financial relationships.
Mohamed S. Elgendy indicated no relevant financial relationships.
Emmanuel Olumuyide indicated no relevant financial relationships.
Ameer Awashra indicated no relevant financial relationships.
Hosam I. Taha indicated no relevant financial relationships.
Qutaiba Qafisheh indicated no relevant financial relationships.
Mohammad Alqadi indicated no relevant financial relationships.
Mohammad O. Abdelhafez indicated no relevant financial relationships.
Muath A. Baniowda indicated no relevant financial relationships.
Ahmed Abuhasna, DO1, Abdalhakim Shubietah, MD1, Islam Rajab, MD2, Mohammad Ghannam, MD3, Abdallah Hussein, MD4, Hamid U.. Rahman, MD1, Mohamed S. Elgendy, MBBCh5, Emmanuel Olumuyide, MD1, Ameer Awashra, MD6, Hosam I. Taha, MBBCh5, Qutaiba Qafisheh, MD7, Mohammad Alqadi, MD7, Mohammad O. Abdelhafez, MD8, Muath A. Baniowda, MD9. P1213 - Two Decades of Inflammatory Bowel Disease-Related Cardiovascular Mortality in the United States: Temporal Trends and Demographic Disparities From a National Death Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
