Sunday Poster Session
Category: IBD
P1212 - Evidence of a Hypercoagulable State in Inflammatory Bowel Disease Patients With Primary Sclerosing Cholangitis: A Propensity-Matched Real-World Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Prabhat Kumar, MD (he/him/his)
Virginia Commonwealth University
Richmond, VA
Presenting Author(s)
Prabhat Kumar, MD1, Mohamed Nadeem, MD2, Nayef Kiame, MS2, Anusha Agarwal, MD3, Archana Kharel, MD3, Stephen J. Bickston, MD, FACG4, Joseph Sleiman, MD2
1Virginia Commonwealth University, Richmond, VA; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Virginia Commonwealth University Health System, Richmond, VA
Introduction: Inflammatory bowel disease (IBD) confers a systemic hypercoagulable state, increasing the risk of thromboembolic complications. Primary sclerosing cholangitis (PSC), a chronic cholestatic liver disease that commonly coexists with IBD, may further amplify this prothrombotic risk. However, real-world data on thrombotic outcomes in patients with concurrent IBD and PSC remain sparse. We aimed to evaluate the impact of coexisting PSC on thromboembolic risk among patients with IBD using a large federated health research network.
Methods: We performed a retrospective cross-sectional analysis using the TriNetX Global Research Network, including adults (≥18 years) diagnosed between 2010–2024. Three mutually exclusive comparisons were made: (1) IBD-only vs. IBD+PSC, (2) PSC-only vs. IBD+PSC, and (3) IBD-only vs. PSC-only. Patients with prior thromboembolism or arterial occlusion were excluded. Propensity score matching (1:1) accounted for age, sex, race, diabetes, hypertension, hyperlipidemia, tobacco use, and cardiovascular disease. Primary outcomes were portal vein thrombosis (PVT), deep vein thrombosis (DVT), mesenteric ischemia, and arterial thrombosis over a 10-year period. Risk ratios (RR), odds ratios (OR), and p-values were calculated using Fisher’s exact test.
Results: Post-matching, three cohorts of 6542, 4504, and 6776 patients were analyzed. Compared to IBD-only, the IBD+PSC group had significantly higher odds of PVT (RR 7.29; OR 7.37; p< 0.01) and DVT (RR 1.52; OR 1.53; p=0.0047). Compared to PSC-only, the IBD+PSC group also had elevated odds of PVT (OR 10.9; p< 0.001) and DVT (OR 2.99; p< 0.001). No significant differences were noted in mesenteric ischemia or arterial thrombosis. Interestingly, PSC-only patients had lower odds of DVT and mesenteric ischemia compared to the IBD-only cohort.
Discussion: Patients with coexisting PSC and IBD have a significantly increased risk of venous thrombotic events—particularly PVT and DVT—versus those with either condition alone. These findings suggest an amplified hypercoagulable state in this dual-diagnosis group. Further studies are warranted to evaluate contributions of cirrhosis, IBD phenotype, colorectal cancer, hepatocellular carcinoma, and hospitalization burden in shaping thrombotic risk.
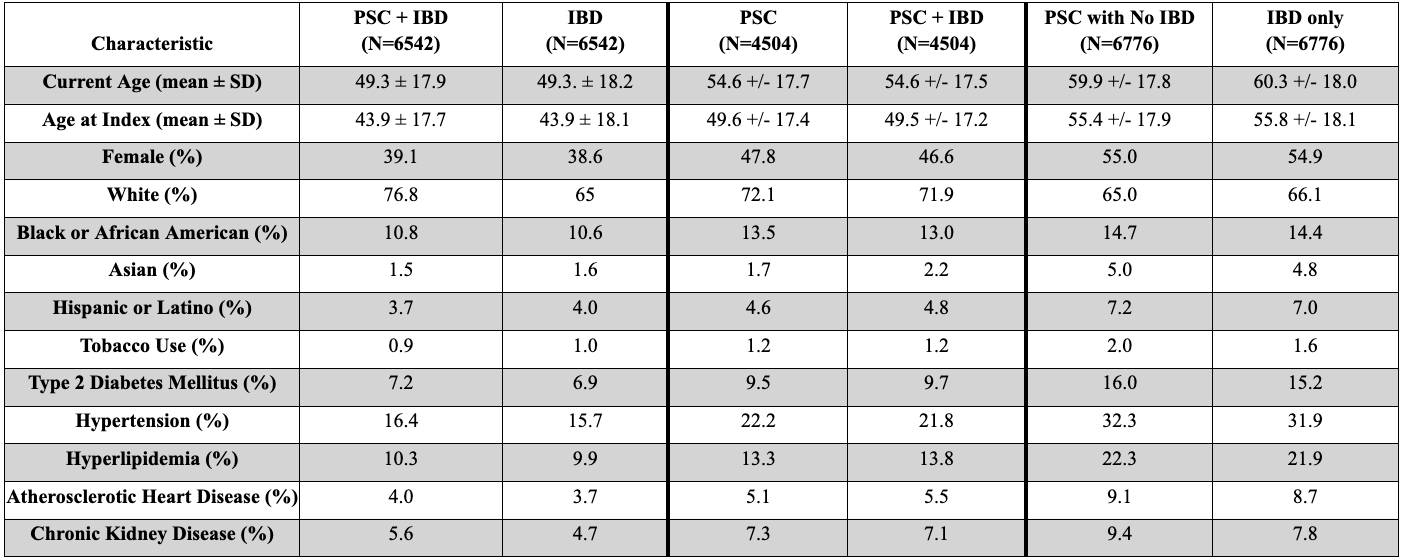
Figure: Table 1: Post-matching demographic and clinical characteristics of patients with inflammatory bowel disease (IBD) only, primary sclerosing cholangitis (PSC) only, and combined PSC with IBD. Values reflect mean ± standard deviation for continuous variables and percentages for categorical variables.
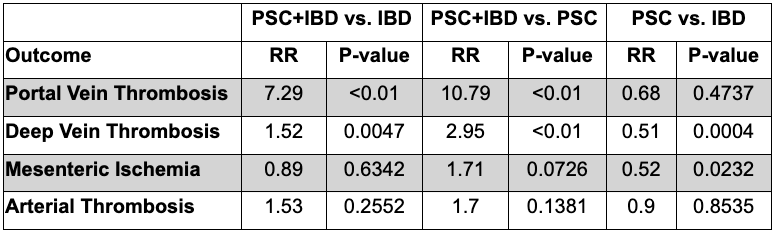
Figure: Table 2. Comparative risk ratios (RR) and p-values for thromboembolic outcomes across three patient groups: IBD-only, PSC-only, and PSC with IBD. Data derived from a TriNetX federated real-world analysis
Disclosures:
Prabhat Kumar indicated no relevant financial relationships.
Mohamed Nadeem indicated no relevant financial relationships.
Nayef Kiame indicated no relevant financial relationships.
Anusha Agarwal indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Joseph Sleiman indicated no relevant financial relationships.
Prabhat Kumar, MD1, Mohamed Nadeem, MD2, Nayef Kiame, MS2, Anusha Agarwal, MD3, Archana Kharel, MD3, Stephen J. Bickston, MD, FACG4, Joseph Sleiman, MD2. P1212 - Evidence of a Hypercoagulable State in Inflammatory Bowel Disease Patients With Primary Sclerosing Cholangitis: A Propensity-Matched Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Virginia Commonwealth University, Richmond, VA; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Virginia Commonwealth University Health System, Richmond, VA
Introduction: Inflammatory bowel disease (IBD) confers a systemic hypercoagulable state, increasing the risk of thromboembolic complications. Primary sclerosing cholangitis (PSC), a chronic cholestatic liver disease that commonly coexists with IBD, may further amplify this prothrombotic risk. However, real-world data on thrombotic outcomes in patients with concurrent IBD and PSC remain sparse. We aimed to evaluate the impact of coexisting PSC on thromboembolic risk among patients with IBD using a large federated health research network.
Methods: We performed a retrospective cross-sectional analysis using the TriNetX Global Research Network, including adults (≥18 years) diagnosed between 2010–2024. Three mutually exclusive comparisons were made: (1) IBD-only vs. IBD+PSC, (2) PSC-only vs. IBD+PSC, and (3) IBD-only vs. PSC-only. Patients with prior thromboembolism or arterial occlusion were excluded. Propensity score matching (1:1) accounted for age, sex, race, diabetes, hypertension, hyperlipidemia, tobacco use, and cardiovascular disease. Primary outcomes were portal vein thrombosis (PVT), deep vein thrombosis (DVT), mesenteric ischemia, and arterial thrombosis over a 10-year period. Risk ratios (RR), odds ratios (OR), and p-values were calculated using Fisher’s exact test.
Results: Post-matching, three cohorts of 6542, 4504, and 6776 patients were analyzed. Compared to IBD-only, the IBD+PSC group had significantly higher odds of PVT (RR 7.29; OR 7.37; p< 0.01) and DVT (RR 1.52; OR 1.53; p=0.0047). Compared to PSC-only, the IBD+PSC group also had elevated odds of PVT (OR 10.9; p< 0.001) and DVT (OR 2.99; p< 0.001). No significant differences were noted in mesenteric ischemia or arterial thrombosis. Interestingly, PSC-only patients had lower odds of DVT and mesenteric ischemia compared to the IBD-only cohort.
Discussion: Patients with coexisting PSC and IBD have a significantly increased risk of venous thrombotic events—particularly PVT and DVT—versus those with either condition alone. These findings suggest an amplified hypercoagulable state in this dual-diagnosis group. Further studies are warranted to evaluate contributions of cirrhosis, IBD phenotype, colorectal cancer, hepatocellular carcinoma, and hospitalization burden in shaping thrombotic risk.
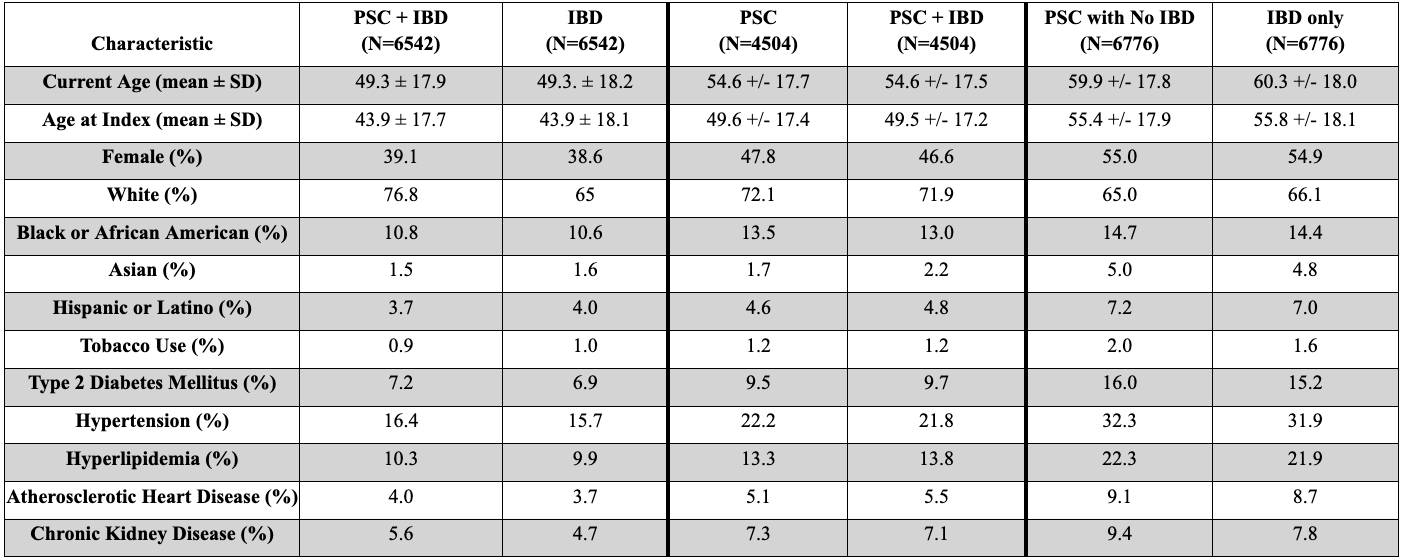
Figure: Table 1: Post-matching demographic and clinical characteristics of patients with inflammatory bowel disease (IBD) only, primary sclerosing cholangitis (PSC) only, and combined PSC with IBD. Values reflect mean ± standard deviation for continuous variables and percentages for categorical variables.
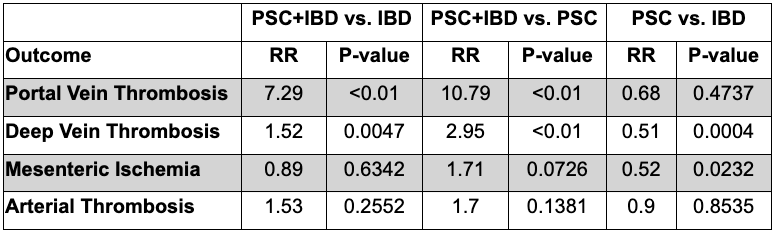
Figure: Table 2. Comparative risk ratios (RR) and p-values for thromboembolic outcomes across three patient groups: IBD-only, PSC-only, and PSC with IBD. Data derived from a TriNetX federated real-world analysis
Disclosures:
Prabhat Kumar indicated no relevant financial relationships.
Mohamed Nadeem indicated no relevant financial relationships.
Nayef Kiame indicated no relevant financial relationships.
Anusha Agarwal indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Joseph Sleiman indicated no relevant financial relationships.
Prabhat Kumar, MD1, Mohamed Nadeem, MD2, Nayef Kiame, MS2, Anusha Agarwal, MD3, Archana Kharel, MD3, Stephen J. Bickston, MD, FACG4, Joseph Sleiman, MD2. P1212 - Evidence of a Hypercoagulable State in Inflammatory Bowel Disease Patients With Primary Sclerosing Cholangitis: A Propensity-Matched Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
