Sunday Poster Session
Category: IBD
P1209 - Mineralocorticoid Receptor Antagonist Use Is Associated With Improved Clinical Outcomes in Crohn’s Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MS
Michael Saadeh, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Michael Saadeh, MD1, Apoorva K. Chandar, MBBS, MPH2, Jeffry A.. Katz, MD1, Miguel Regueiro, MD3
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Crohn’s disease (CD) is marked by intestinal inflammation and often complicated by intestinal fibrosis and stricturing disease. Mineralocorticoid receptor antagonists (MRA), such as spironolactone and eplerenone, have demonstrated anti-fibrotic properties in preclinical studies, but their role in clinical, real-world studies has yet to be evaluated. We investigated their clinical effects in the context of stricturing Crohn’s disease.
Methods: Using TriNetX, a large healthcare database comprising over 120 million patients in the United States, we identified cohorts of patients with CD on one or more CD medications using ICD-10 codes, and excluded those with cirrhosis or portal hypertension. We categorized these patients into 2 subgroups based on their exposure to MRA. Cases were CD patients on MRA, and controls were CD patients without exposure to MRA. The two cohorts were propensity matched for demographics, comorbidities including tobacco use, diabetes, and types of heart failure, inflammatory markers, and CD medications. The outcomes of interest were defined as CD-related surgery, steroid use, and intestinal strictures 3 months to 5 years after the index event of MRA use. We stratified our analysis by the inclusion or exclusion of prior intestinal strictures. Chi-square and t-tests were used for significance testing.
Results: There were 7,305 cases and 149,104 controls. After propensity matching, 6,843 who were evenly matched. When compared to patients with CD and no exposure to MRA, those with CD on MRA were less likely to have CD-related surgery (OR 0.59, 95% CI 0.49-0.71) and steroid use (OR 0.83, 95% CI 0.78-0.89). Excluding those with prior stricturing disease, patients with CD on MRA were less likely to have intestinal strictures (OR 0.70, 95% CI 0.60-0.81), and this benefit persisted when including those with prior stricturing disease (OR 0.85, 95% CI 0.77-0.95).
Discussion: In this retrospective cohort study, we found that MRA were associated with decreased CD-related surgery, steroid use, and stricturing disease in patients with CD. These findings support the existing preclinical literature regarding a potential protective role of MRA in fibrostenotic disease. Further research is needed to investigate the clinical use of MRA as anti-fibrotic therapy in this population.
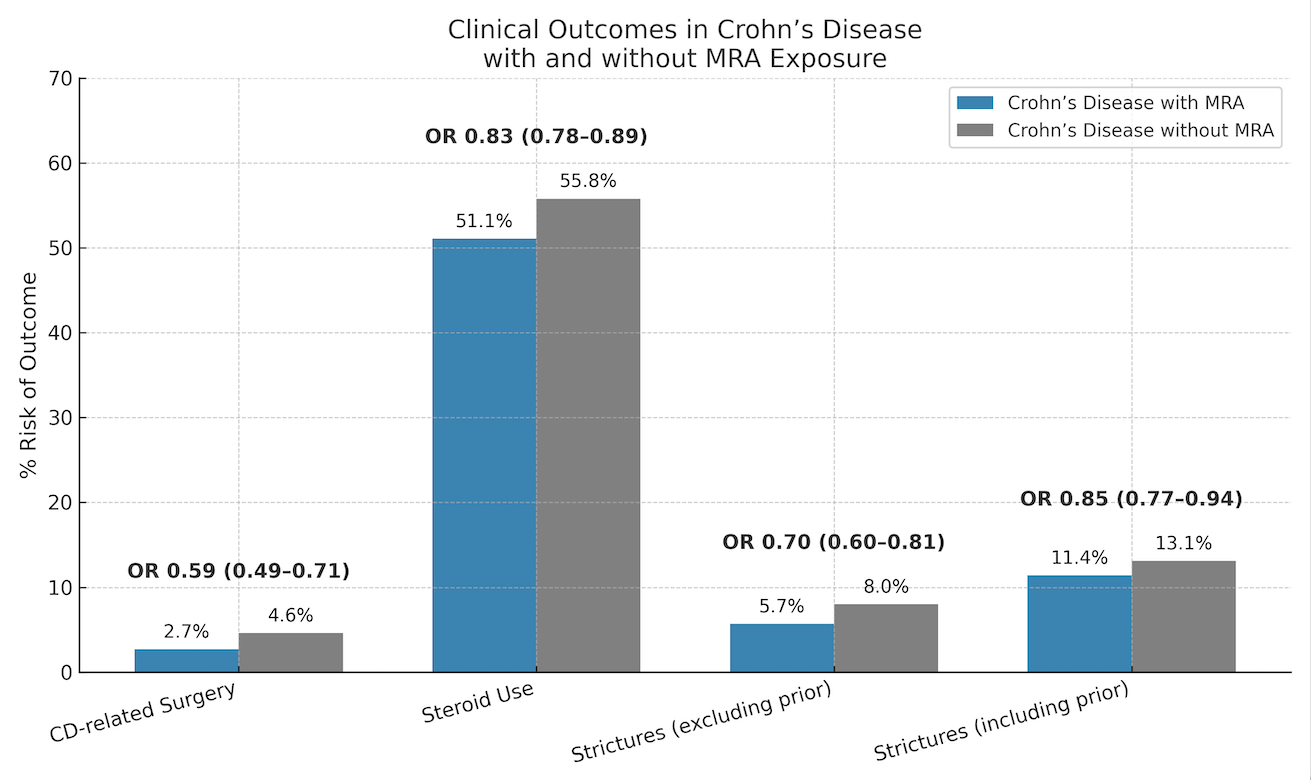
Figure: Graph 1: Clinical Outcomes in Patients With Crohn’s Disease With and Without MRA Therapy
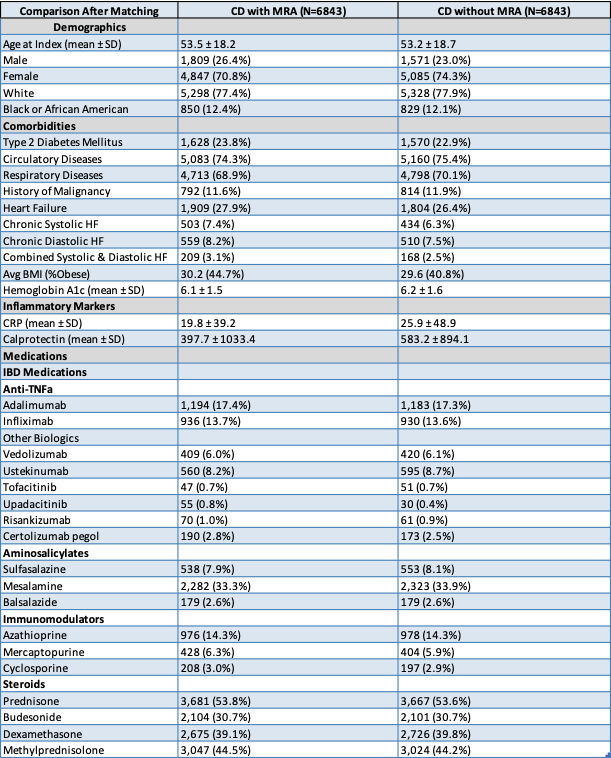
Figure: Table 1: Depicts the Demographics, Comorbidities, Inflammatory Markers, and Medications After Matching the Cases and Controls
Disclosures:
Michael Saadeh indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. BMS – Advisory Committee/Board Member, Consultant. Boehringer Ingelheim Pharmaceuticals Inc. – Advisory Committee/Board Member, Consultant. Celegene – Advisory Committee/Board Member, Consultant. Eli Lilly and Company – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Organon – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant.
Michael Saadeh, MD1, Apoorva K. Chandar, MBBS, MPH2, Jeffry A.. Katz, MD1, Miguel Regueiro, MD3. P1209 - Mineralocorticoid Receptor Antagonist Use Is Associated With Improved Clinical Outcomes in Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH
Introduction: Crohn’s disease (CD) is marked by intestinal inflammation and often complicated by intestinal fibrosis and stricturing disease. Mineralocorticoid receptor antagonists (MRA), such as spironolactone and eplerenone, have demonstrated anti-fibrotic properties in preclinical studies, but their role in clinical, real-world studies has yet to be evaluated. We investigated their clinical effects in the context of stricturing Crohn’s disease.
Methods: Using TriNetX, a large healthcare database comprising over 120 million patients in the United States, we identified cohorts of patients with CD on one or more CD medications using ICD-10 codes, and excluded those with cirrhosis or portal hypertension. We categorized these patients into 2 subgroups based on their exposure to MRA. Cases were CD patients on MRA, and controls were CD patients without exposure to MRA. The two cohorts were propensity matched for demographics, comorbidities including tobacco use, diabetes, and types of heart failure, inflammatory markers, and CD medications. The outcomes of interest were defined as CD-related surgery, steroid use, and intestinal strictures 3 months to 5 years after the index event of MRA use. We stratified our analysis by the inclusion or exclusion of prior intestinal strictures. Chi-square and t-tests were used for significance testing.
Results: There were 7,305 cases and 149,104 controls. After propensity matching, 6,843 who were evenly matched. When compared to patients with CD and no exposure to MRA, those with CD on MRA were less likely to have CD-related surgery (OR 0.59, 95% CI 0.49-0.71) and steroid use (OR 0.83, 95% CI 0.78-0.89). Excluding those with prior stricturing disease, patients with CD on MRA were less likely to have intestinal strictures (OR 0.70, 95% CI 0.60-0.81), and this benefit persisted when including those with prior stricturing disease (OR 0.85, 95% CI 0.77-0.95).
Discussion: In this retrospective cohort study, we found that MRA were associated with decreased CD-related surgery, steroid use, and stricturing disease in patients with CD. These findings support the existing preclinical literature regarding a potential protective role of MRA in fibrostenotic disease. Further research is needed to investigate the clinical use of MRA as anti-fibrotic therapy in this population.
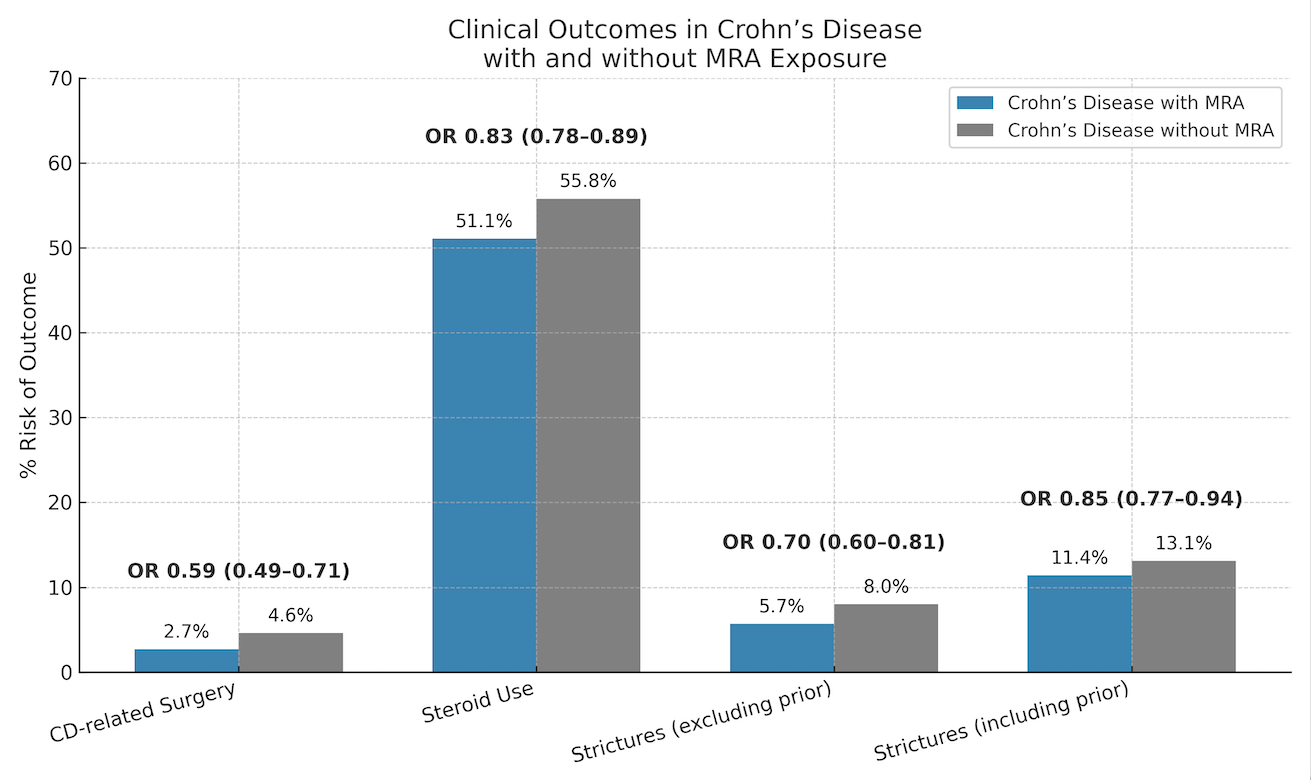
Figure: Graph 1: Clinical Outcomes in Patients With Crohn’s Disease With and Without MRA Therapy
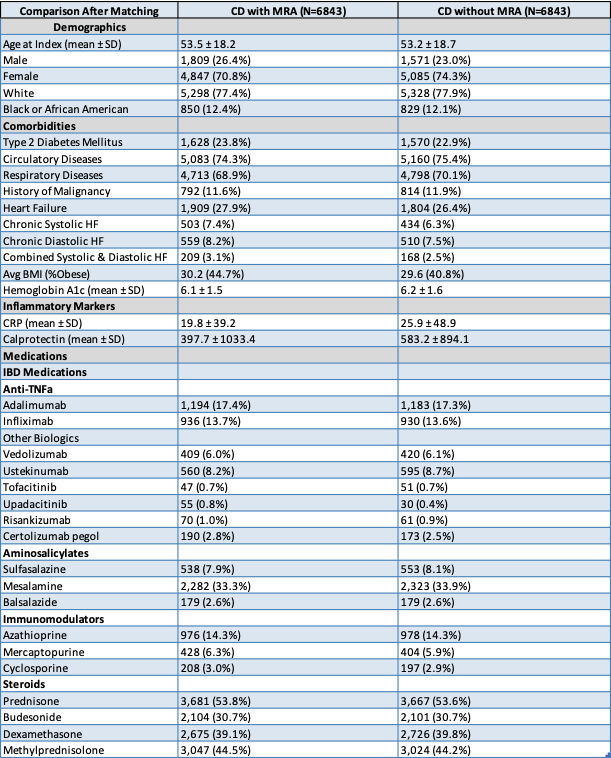
Figure: Table 1: Depicts the Demographics, Comorbidities, Inflammatory Markers, and Medications After Matching the Cases and Controls
Disclosures:
Michael Saadeh indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. BMS – Advisory Committee/Board Member, Consultant. Boehringer Ingelheim Pharmaceuticals Inc. – Advisory Committee/Board Member, Consultant. Celegene – Advisory Committee/Board Member, Consultant. Eli Lilly and Company – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Organon – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant.
Michael Saadeh, MD1, Apoorva K. Chandar, MBBS, MPH2, Jeffry A.. Katz, MD1, Miguel Regueiro, MD3. P1209 - Mineralocorticoid Receptor Antagonist Use Is Associated With Improved Clinical Outcomes in Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
