Sunday Poster Session
Category: IBD
P1204 - Virtual EUA Boosts Clinical Confidence in Complex Perianal Crohn’s Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- TM
Trevor McCracken, MD (he/him/his)
University of California Irvine Health
Orange, CA
Presenting Author(s)
Trevor McCracken, MD1, Sophie Trujillo, DO1, Christopher Chang, MD1, Jeremy Huddy, BMBS, FRCS, PhD2, Valery Vilchez, MD3, Rony Kampalath, MD1, Robert Fearn, MD1, Gauraang Bhatnagar, MBBS, PhD4
1University of California Irvine Health, Orange, CA; 2Frimley Health NHS Trust, Frimley, England, United Kingdom; 3University of California Irvine Health, Irvine, CA; 4University College London Hospitals, Orange, CA
Introduction: Pelvic MRI is the gold standard for assessing perianal Crohn's disease, but interpretation can be challenging for non-radiologists. Virtual Examination under Anesthesia (vEUA) is a novel technology that generates a 3D model to enhance evaluation of fistula anatomy by demarcating the fistula tract in relation to the anal canal and pelvis. This multi-center observational study aims to assess the attitudes of gastroenterologists and surgeons toward this novel MRI technology.
Methods: A panel of gastroenterologists and surgeons reviewed two cases of perianal Crohn's disease and then completed a set of standardized questionnaires (Tables 1 and 2). The first case had a trans-sphincteric tract with two internal openings. The second case had a more complicated trans-sphincteric fistula with tracts extending above the puborectalis muscle (Figure 1).
For each case, participants were provided with a 3D vEUA model and a written report drafted by a radiologist. Participants first reviewed the narrative report and then completed a survey assessing confidence in understanding pathology, clinical decision-making, and ability to provide patient education based on the report. The survey was then repeated after viewing the vEUA model.
Results: Of 50 responses, 23 (46%) were gastroenterologists and 27 (54%) were surgeons. Amongst these, 17 (34%) were trainees.
All scores increased significantly after viewing the vEUA model, there was a 19% improvement for case 1 (MD 1.33 ± 1.71 points p< 0.001) and a 28% improvement for case 2 (MD 2.16 ± 1.88 points p< 0.001). The largest increases were seen in understanding anatomy (p< 0.001) and supporting operative planning (p< 0.05) for case 2.
Gastroenterologists demonstrated greater improvements over surgeons in understanding fistula anatomy (p< 0.01) and overall decision making (p=0.01) for case 1. Trainees demonstrated larger improvement in understanding fistula anatomy (< 0.001) and overall clinical decision making (< 0.005) (Table 3). Free text comments were received from 16 participants; 11 (69%) favored the vEUA model and 5 (31%) were neutral (Table 4).
Discussion: vEUA allows for improved evaluation of fistula anatomy by demarcating the fistula tract and its branches. Gastroenterologists and surgeons, especially trainees, found it helpful for understanding anatomy and guiding management, notably with greater benefit in the more complex case.
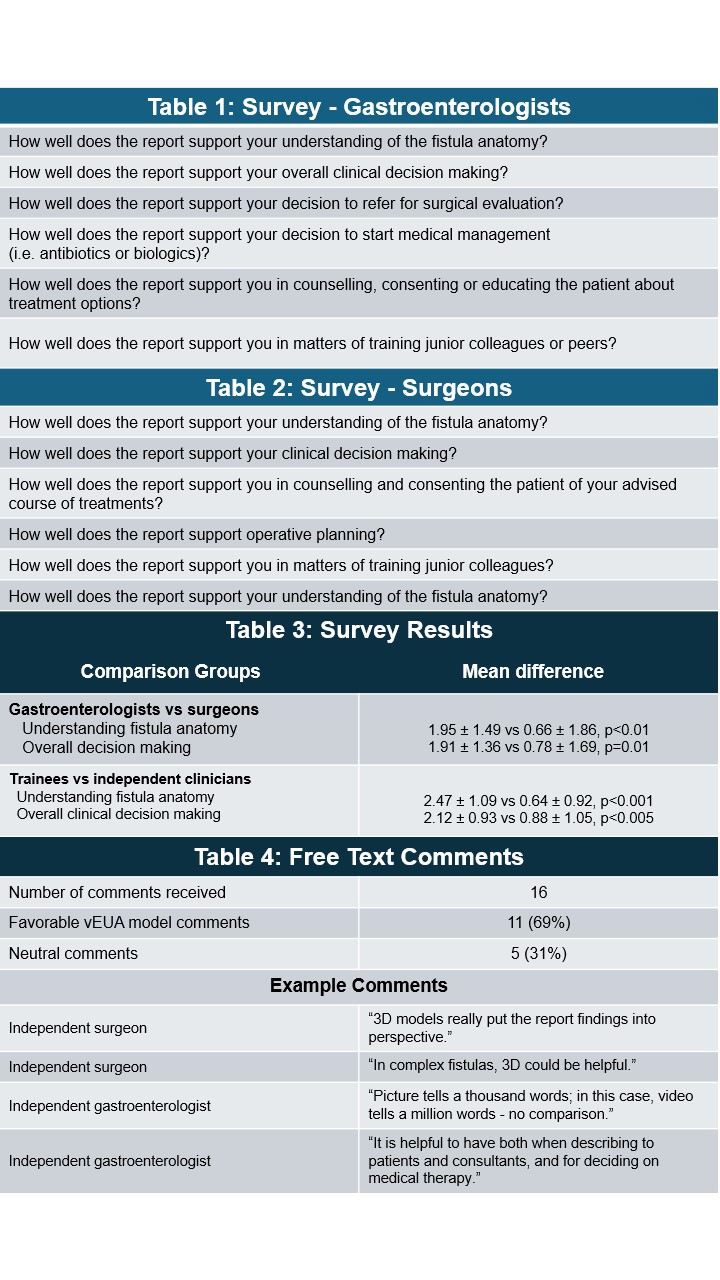
Figure: Figure 1: 3D model generated by virtual exam under anesthesia technology depicting a trans-sphincteric fistula with tracts extending above the puborectalis muscle (case two).

Figure: Table 1: Survey completed by gastroenterologists before and after interacting with virtual exam under anesthesia technology.
Table 2: Survey completed by surgeons before and after interacting with virtual exam under anesthesia technology.
Table 3: Results of survey comparing improvement scores between gastroenterologists and surgeons and improvement scores between trainees and independent clinicians.
Table 4: Free text comments from survey.
Disclosures:
Trevor McCracken indicated no relevant financial relationships.
Sophie Trujillo indicated no relevant financial relationships.
Christopher Chang indicated no relevant financial relationships.
Jeremy Huddy: CMR Surgical – Honorarium from CMR Surgical to partake in robotic human factors study. Motilent – Honorarium to host webinar.
Valery Vilchez indicated no relevant financial relationships.
Rony Kampalath indicated no relevant financial relationships.
Robert Fearn indicated no relevant financial relationships.
Gauraang Bhatnagar indicated no relevant financial relationships.
Trevor McCracken, MD1, Sophie Trujillo, DO1, Christopher Chang, MD1, Jeremy Huddy, BMBS, FRCS, PhD2, Valery Vilchez, MD3, Rony Kampalath, MD1, Robert Fearn, MD1, Gauraang Bhatnagar, MBBS, PhD4. P1204 - Virtual EUA Boosts Clinical Confidence in Complex Perianal Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Irvine Health, Orange, CA; 2Frimley Health NHS Trust, Frimley, England, United Kingdom; 3University of California Irvine Health, Irvine, CA; 4University College London Hospitals, Orange, CA
Introduction: Pelvic MRI is the gold standard for assessing perianal Crohn's disease, but interpretation can be challenging for non-radiologists. Virtual Examination under Anesthesia (vEUA) is a novel technology that generates a 3D model to enhance evaluation of fistula anatomy by demarcating the fistula tract in relation to the anal canal and pelvis. This multi-center observational study aims to assess the attitudes of gastroenterologists and surgeons toward this novel MRI technology.
Methods: A panel of gastroenterologists and surgeons reviewed two cases of perianal Crohn's disease and then completed a set of standardized questionnaires (Tables 1 and 2). The first case had a trans-sphincteric tract with two internal openings. The second case had a more complicated trans-sphincteric fistula with tracts extending above the puborectalis muscle (Figure 1).
For each case, participants were provided with a 3D vEUA model and a written report drafted by a radiologist. Participants first reviewed the narrative report and then completed a survey assessing confidence in understanding pathology, clinical decision-making, and ability to provide patient education based on the report. The survey was then repeated after viewing the vEUA model.
Results: Of 50 responses, 23 (46%) were gastroenterologists and 27 (54%) were surgeons. Amongst these, 17 (34%) were trainees.
All scores increased significantly after viewing the vEUA model, there was a 19% improvement for case 1 (MD 1.33 ± 1.71 points p< 0.001) and a 28% improvement for case 2 (MD 2.16 ± 1.88 points p< 0.001). The largest increases were seen in understanding anatomy (p< 0.001) and supporting operative planning (p< 0.05) for case 2.
Gastroenterologists demonstrated greater improvements over surgeons in understanding fistula anatomy (p< 0.01) and overall decision making (p=0.01) for case 1. Trainees demonstrated larger improvement in understanding fistula anatomy (< 0.001) and overall clinical decision making (< 0.005) (Table 3). Free text comments were received from 16 participants; 11 (69%) favored the vEUA model and 5 (31%) were neutral (Table 4).
Discussion: vEUA allows for improved evaluation of fistula anatomy by demarcating the fistula tract and its branches. Gastroenterologists and surgeons, especially trainees, found it helpful for understanding anatomy and guiding management, notably with greater benefit in the more complex case.
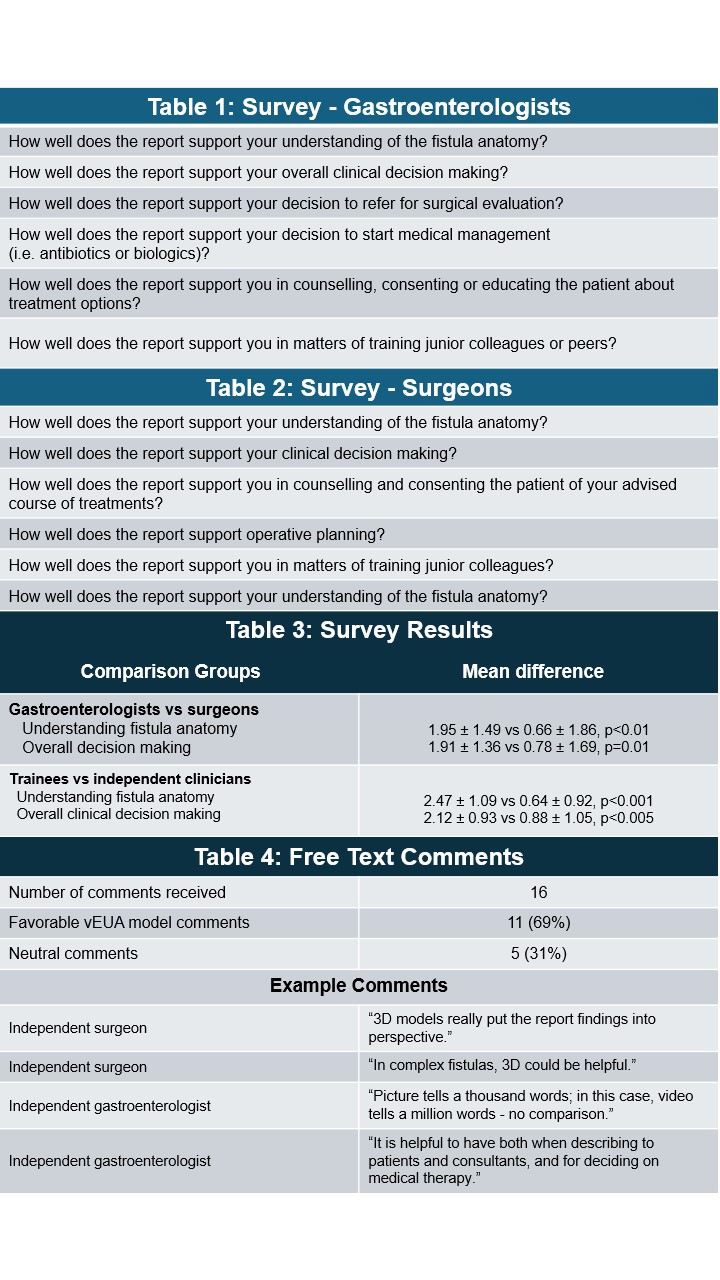
Figure: Figure 1: 3D model generated by virtual exam under anesthesia technology depicting a trans-sphincteric fistula with tracts extending above the puborectalis muscle (case two).

Figure: Table 1: Survey completed by gastroenterologists before and after interacting with virtual exam under anesthesia technology.
Table 2: Survey completed by surgeons before and after interacting with virtual exam under anesthesia technology.
Table 3: Results of survey comparing improvement scores between gastroenterologists and surgeons and improvement scores between trainees and independent clinicians.
Table 4: Free text comments from survey.
Disclosures:
Trevor McCracken indicated no relevant financial relationships.
Sophie Trujillo indicated no relevant financial relationships.
Christopher Chang indicated no relevant financial relationships.
Jeremy Huddy: CMR Surgical – Honorarium from CMR Surgical to partake in robotic human factors study. Motilent – Honorarium to host webinar.
Valery Vilchez indicated no relevant financial relationships.
Rony Kampalath indicated no relevant financial relationships.
Robert Fearn indicated no relevant financial relationships.
Gauraang Bhatnagar indicated no relevant financial relationships.
Trevor McCracken, MD1, Sophie Trujillo, DO1, Christopher Chang, MD1, Jeremy Huddy, BMBS, FRCS, PhD2, Valery Vilchez, MD3, Rony Kampalath, MD1, Robert Fearn, MD1, Gauraang Bhatnagar, MBBS, PhD4. P1204 - Virtual EUA Boosts Clinical Confidence in Complex Perianal Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
