Sunday Poster Session
Category: IBD
P1203 - Beyond the Gut: A 7-Year Nationwide Review of Prevalence and Predictors of Food Allergies in Inflammatory Bowel Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abhin Sapkota, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Abhin Sapkota, MD1, Maria Grba, MD1, Kriti Katwal, 2, Gedion Amdetsion, MD1, Daniel Guifarro Rivera, MD3, Saksham Kohli, MBBS1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Palpa, Lumbini, Nepal; 3Cook County Health and Hospital Systems, Chicago, IL
Introduction: The interplay between food allergy (FA) and inflammatory bowel disease (IBD) remains under explored despite potential implications for disease activity and outcomes. We aimed to examine national trends and demographic factors associated with food allergy among hospitalized IBD patients in the United States.
Methods: A retrospective analysis of 2016–2022 National Inpatient Sample database was done to identify hospitalizations with a primary or secondary diagnosis of IBD (Crohn’s disease or Ulcerative colitis) and common FA (milk, egg, peanut, seafood) using appropriate International Classification of Diseases, 10th revision codes. Demographic and hospital-level factors were compared using multivariate logistic regression. Longitudinal trend analysis was done as well. Statistical significance was defined as p< 0.05.
Results: Among 2,300,169 admissions with IBD, 25,659 (1.1%) had a concomitant FA. Mean length of stay was slightly shorter in the food allergy group (5.08 vs. 5.49 days, p< 0.001), and mean hospitalization charges were comparable ($61,135 vs. $63,075). IBD patients with FA were younger (mean age 46.6 vs. 53.2 years, p< 0.001), more likely to be female (aOR 1.21, p< 0.001), and had a slightly lower in-hospital mortality (1.77% vs. 1.8%, p< 0.001). Black (aOR 1.93, p< 0.001), Hispanic (aOR 1.49, p< 0.001), and other non-White races (aOR 1.46, p< 0.001) were more likely to have FA compared to White patients. Higher comorbidity burden was associated with greater odds of FA, with peak association at CCI=1 (aOR 1.61, p< 0.001) compared to CCI 0. Medicaid (aOR 0.88, p=0.019) and private insurance (aOR 0.90, p=0.025) had slightly lower odds of FA compared to Medicare. The prevalence of FA increased from 0.9% in 2016 to 1.23% in 2022.
Discussion: The prevalence of FA among hospitalized IBD patients has increased over the past seven years, particularly in younger, female, and racial minority populations. These findings suggest important demographic disparities and support the need for focused dietary and allergy evaluation in IBD patients.
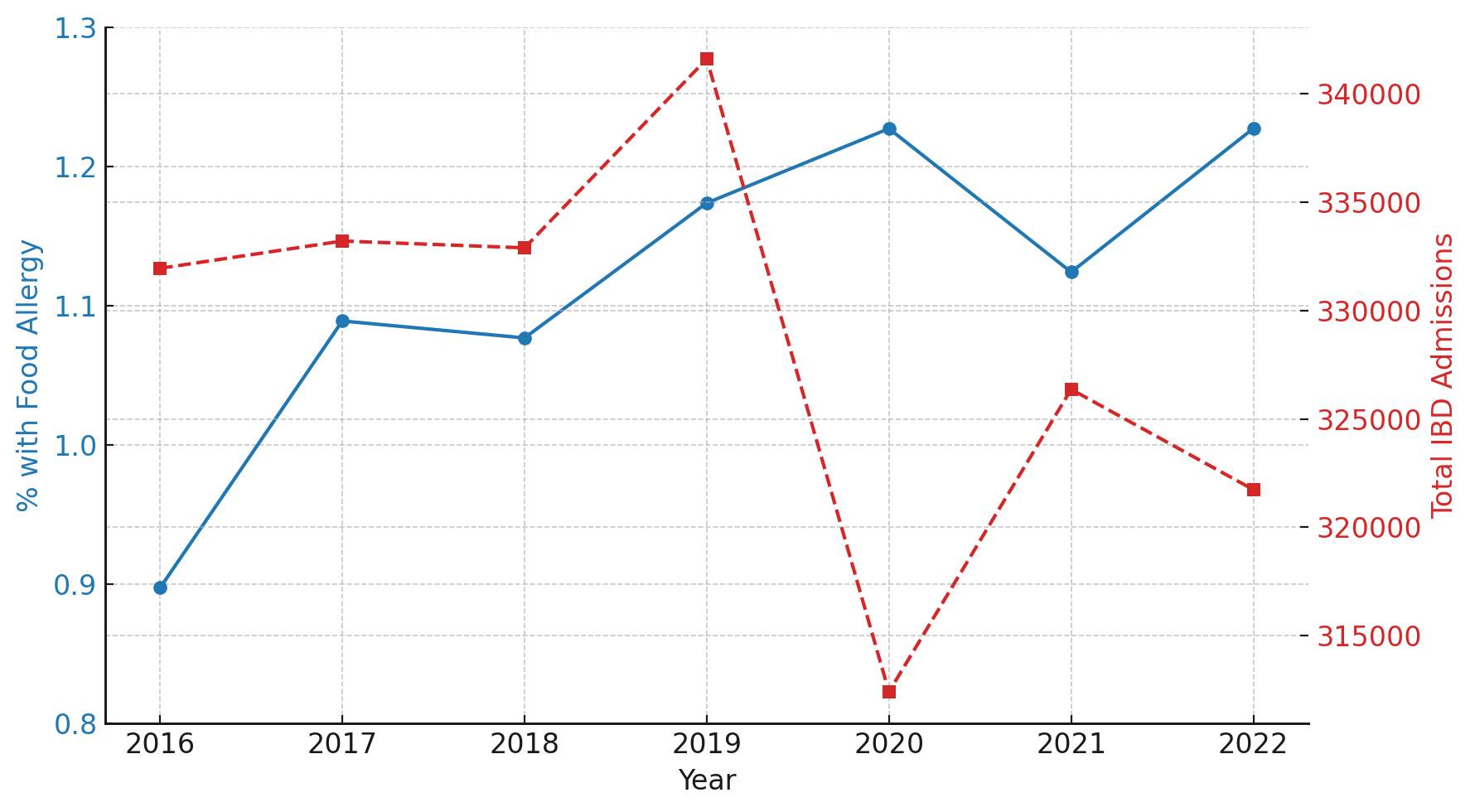
Figure: Table 1. Baseline characteristics and multivariable predictors of food allergy among hospitalized patients with inflammatory bowel disease.
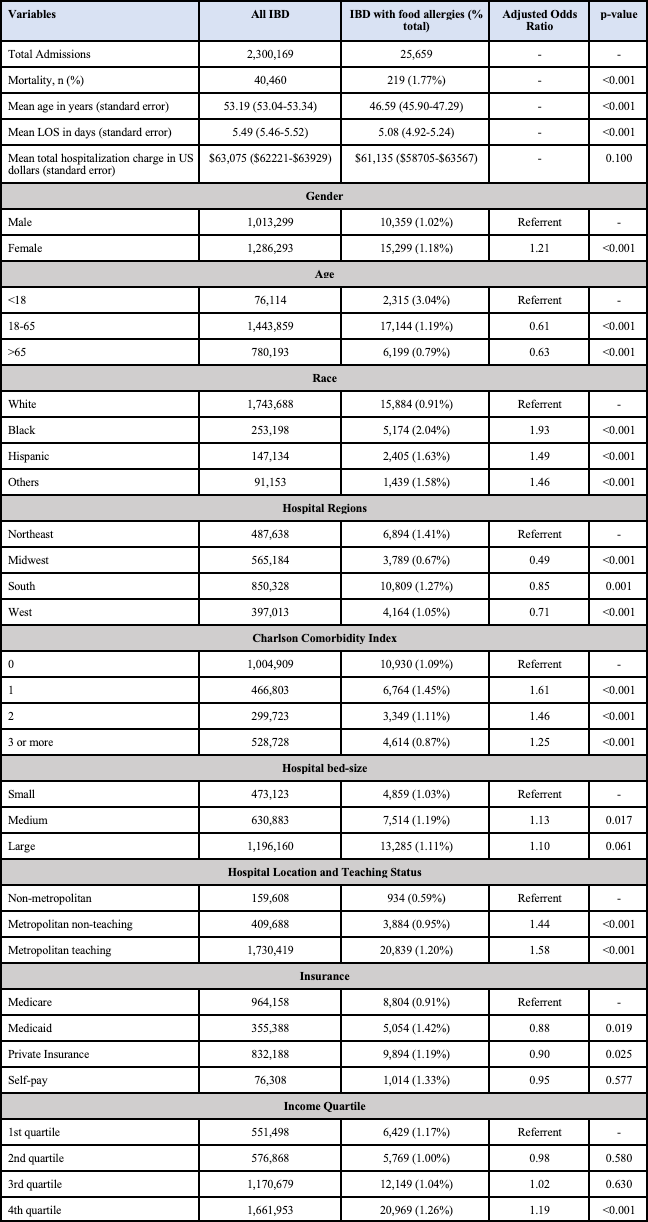
Figure: Figure 1. Temporal trends in the prevalence of food allergy among hospitalized IBD patients (blue line, left y-axis) and total IBD hospitalizations (red dashed line, right y-axis) in the United States from 2016 to 2022.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Gedion Amdetsion indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Abhin Sapkota, MD1, Maria Grba, MD1, Kriti Katwal, 2, Gedion Amdetsion, MD1, Daniel Guifarro Rivera, MD3, Saksham Kohli, MBBS1. P1203 - Beyond the Gut: A 7-Year Nationwide Review of Prevalence and Predictors of Food Allergies in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Palpa, Lumbini, Nepal; 3Cook County Health and Hospital Systems, Chicago, IL
Introduction: The interplay between food allergy (FA) and inflammatory bowel disease (IBD) remains under explored despite potential implications for disease activity and outcomes. We aimed to examine national trends and demographic factors associated with food allergy among hospitalized IBD patients in the United States.
Methods: A retrospective analysis of 2016–2022 National Inpatient Sample database was done to identify hospitalizations with a primary or secondary diagnosis of IBD (Crohn’s disease or Ulcerative colitis) and common FA (milk, egg, peanut, seafood) using appropriate International Classification of Diseases, 10th revision codes. Demographic and hospital-level factors were compared using multivariate logistic regression. Longitudinal trend analysis was done as well. Statistical significance was defined as p< 0.05.
Results: Among 2,300,169 admissions with IBD, 25,659 (1.1%) had a concomitant FA. Mean length of stay was slightly shorter in the food allergy group (5.08 vs. 5.49 days, p< 0.001), and mean hospitalization charges were comparable ($61,135 vs. $63,075). IBD patients with FA were younger (mean age 46.6 vs. 53.2 years, p< 0.001), more likely to be female (aOR 1.21, p< 0.001), and had a slightly lower in-hospital mortality (1.77% vs. 1.8%, p< 0.001). Black (aOR 1.93, p< 0.001), Hispanic (aOR 1.49, p< 0.001), and other non-White races (aOR 1.46, p< 0.001) were more likely to have FA compared to White patients. Higher comorbidity burden was associated with greater odds of FA, with peak association at CCI=1 (aOR 1.61, p< 0.001) compared to CCI 0. Medicaid (aOR 0.88, p=0.019) and private insurance (aOR 0.90, p=0.025) had slightly lower odds of FA compared to Medicare. The prevalence of FA increased from 0.9% in 2016 to 1.23% in 2022.
Discussion: The prevalence of FA among hospitalized IBD patients has increased over the past seven years, particularly in younger, female, and racial minority populations. These findings suggest important demographic disparities and support the need for focused dietary and allergy evaluation in IBD patients.
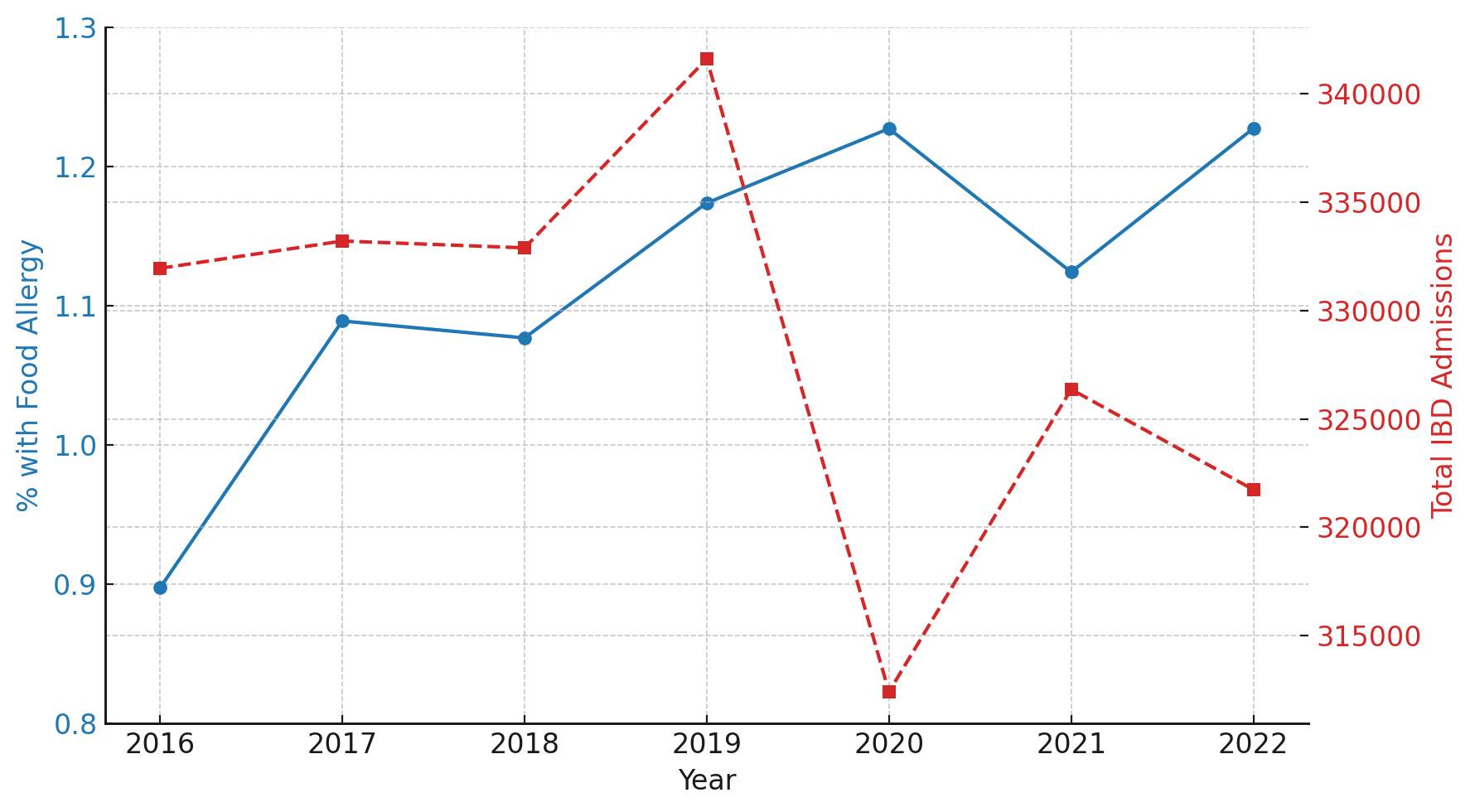
Figure: Table 1. Baseline characteristics and multivariable predictors of food allergy among hospitalized patients with inflammatory bowel disease.
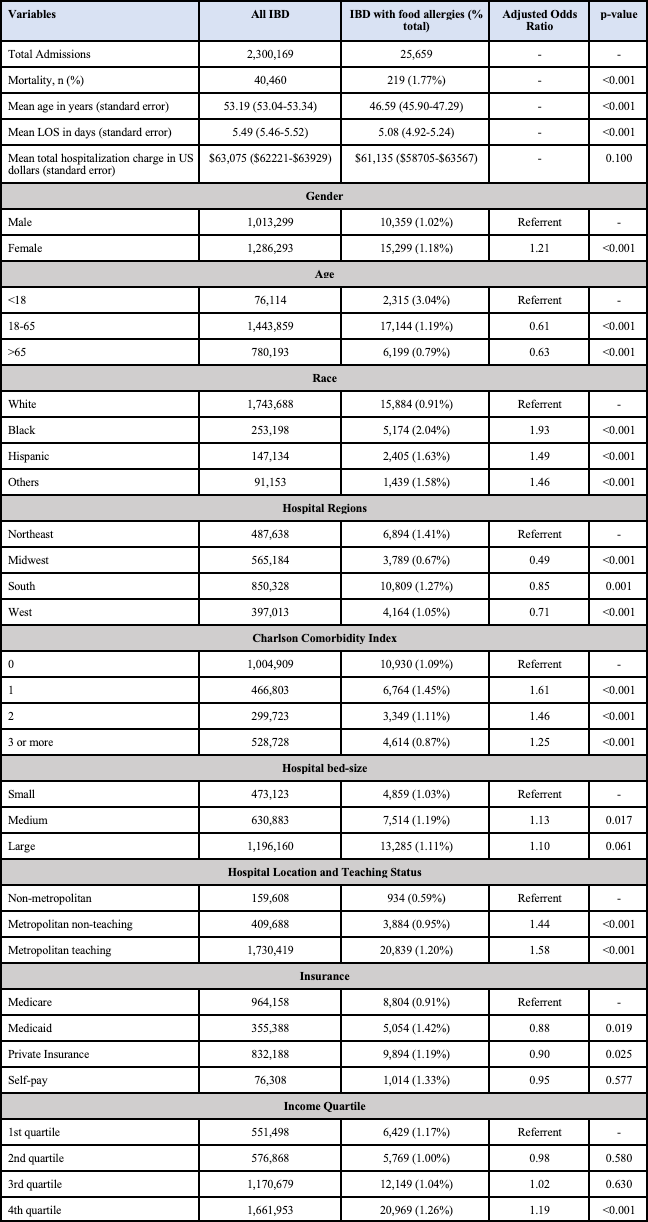
Figure: Figure 1. Temporal trends in the prevalence of food allergy among hospitalized IBD patients (blue line, left y-axis) and total IBD hospitalizations (red dashed line, right y-axis) in the United States from 2016 to 2022.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Gedion Amdetsion indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Abhin Sapkota, MD1, Maria Grba, MD1, Kriti Katwal, 2, Gedion Amdetsion, MD1, Daniel Guifarro Rivera, MD3, Saksham Kohli, MBBS1. P1203 - Beyond the Gut: A 7-Year Nationwide Review of Prevalence and Predictors of Food Allergies in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
