Sunday Poster Session
Category: IBD
P1202 - Determinants of Eating Disorders Among Hospitalized Patients With Inflammatory Bowel Disease: A Seven-Year Nationwide Review (2016–2022)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Abhin Sapkota, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Abhin Sapkota, MD1, Maria Grba, MD1, Kriti Katwal, 2, Daniel Guifarro Rivera, MD3, Gedion Amdetsion, MD1, Kajali Mishra, MD4
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Palpa, Lumbini, Nepal; 3Cook County Health and Hospital Systems, Chicago, IL; 4Cook County Health, Chicago, IL
Introduction: Eating disorders (ED) are increasingly recognized as comorbid psychiatric conditions in patients with inflammatory bowel disease (IBD), potentially influencing disease course, nutritional status, and healthcare utilization. However, contemporary national data examining trends and sociodemographic determinants of EDs in IBD patients is lacking.
Methods: A retrospective cohort study was done using data from the National Inpatient Sample database between 2016 and 2022 to identify hospitalizations with a principal or secondary diagnosis of IBD (Crohn’s disease or Ulcerative colitis) and common eating disorders using appropriate International Classification of Diseases, 10th revision codes. Baseline demographics, hospital characteristics, and socioeconomic and hospital-level factors were assessed. Logistic regression was use to identify independent determinants of ED. Statistical significance was defined as p< 0.05.
Results: Among 2,300,169 IBD patients, 3,179 (0.13%) had a concurrent diagnosis of ED. Patients with concomitant ED were significantly younger, with a mean age of 38.1 years compared to 53.2 years in those without ED (p< 0.001), and were predominantly female (81.0% vs. 55.9%; adjusted odds ratio [aOR] 3.57, p< 0.001). The ED cohort experienced a longer mean length of stay (10.04 vs. 5.49 days, p< 0.001) and higher mean charges ($78,195 vs. $63,075, p=0.008). Compared to those under 18 years, those aged 18–65 years (aOR 0.61, p=0.003) and over 65 years (aOR 0.34, p< 0.001) had lower odds of ED. Black (aOR 0.36, p< 0.001) and Hispanic (aOR 0.53, p=0.003) patients had lower odds compared to white. The highest income quartile was associated with increased odds (aOR 1.63, p< 0.001) compared to the lowest. Compared to Medicare or Medicaid, private insurance and self-pay (aOR 1.47, p< 0.001) had higher odds of ED. Regarding IBD subtype, Crohn’s disease had a similar prevalence and distribution of ED subtypes compared to Ulcerative colitis. The prevalence of ED showed modest but steady increase, rising from 0.13% in 2016 to 0.17% in 2022.
Discussion: Although ED remain relatively uncommon among IBD patients, their prevalence has shown a gradual rise over the years. ED disproportionately affect younger, white, female IBD patients with higher socioeconomic status and are associated with prolonged hospitalizations and increased resource use. These findings highlight the need for improved psychiatric screening and multidisciplinary management strategies, particularly in high-risk subgroups.
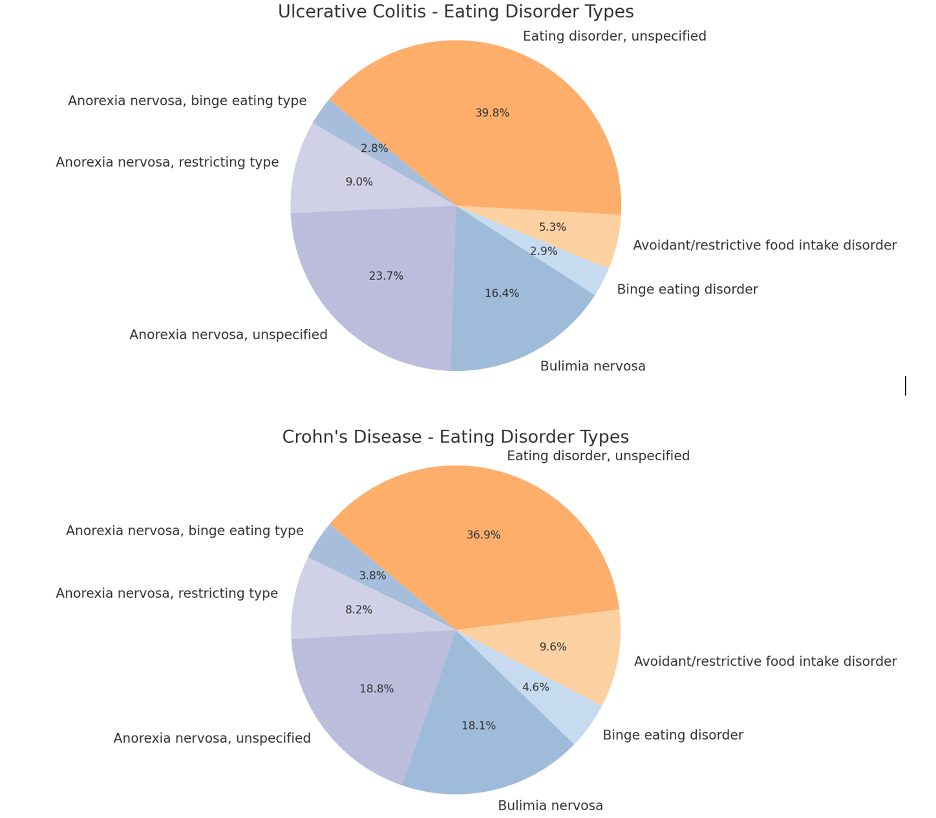
Figure: Table 1. Sociodemographic determinants of Eating Disorders in Inflammatory Bowel Disease.
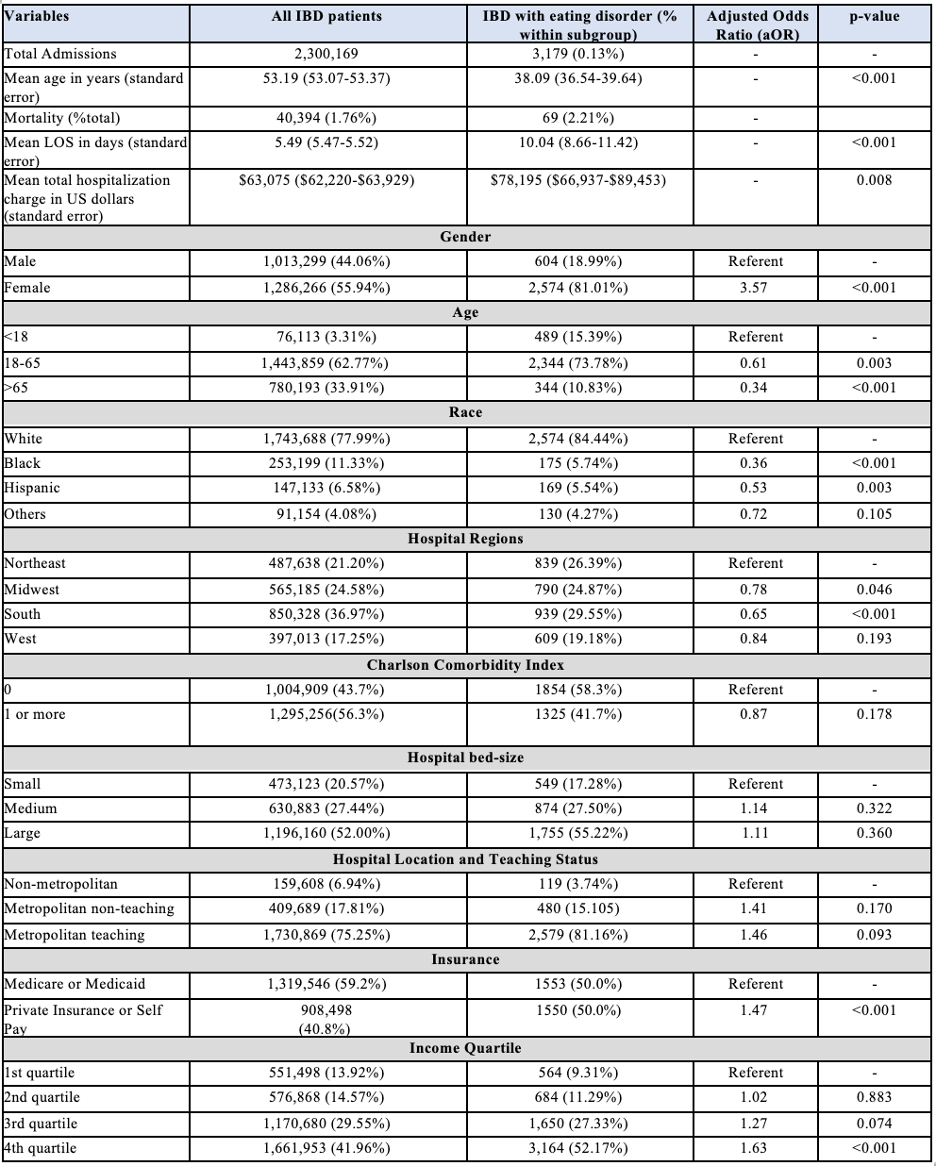
Figure: Figure 1. Distribution of Eating Disorder subtypes among Ulcerative Colitis and Crohn's Disease patients.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Gedion Amdetsion indicated no relevant financial relationships.
Kajali Mishra indicated no relevant financial relationships.
Abhin Sapkota, MD1, Maria Grba, MD1, Kriti Katwal, 2, Daniel Guifarro Rivera, MD3, Gedion Amdetsion, MD1, Kajali Mishra, MD4. P1202 - Determinants of Eating Disorders Among Hospitalized Patients With Inflammatory Bowel Disease: A Seven-Year Nationwide Review (2016–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Palpa, Lumbini, Nepal; 3Cook County Health and Hospital Systems, Chicago, IL; 4Cook County Health, Chicago, IL
Introduction: Eating disorders (ED) are increasingly recognized as comorbid psychiatric conditions in patients with inflammatory bowel disease (IBD), potentially influencing disease course, nutritional status, and healthcare utilization. However, contemporary national data examining trends and sociodemographic determinants of EDs in IBD patients is lacking.
Methods: A retrospective cohort study was done using data from the National Inpatient Sample database between 2016 and 2022 to identify hospitalizations with a principal or secondary diagnosis of IBD (Crohn’s disease or Ulcerative colitis) and common eating disorders using appropriate International Classification of Diseases, 10th revision codes. Baseline demographics, hospital characteristics, and socioeconomic and hospital-level factors were assessed. Logistic regression was use to identify independent determinants of ED. Statistical significance was defined as p< 0.05.
Results: Among 2,300,169 IBD patients, 3,179 (0.13%) had a concurrent diagnosis of ED. Patients with concomitant ED were significantly younger, with a mean age of 38.1 years compared to 53.2 years in those without ED (p< 0.001), and were predominantly female (81.0% vs. 55.9%; adjusted odds ratio [aOR] 3.57, p< 0.001). The ED cohort experienced a longer mean length of stay (10.04 vs. 5.49 days, p< 0.001) and higher mean charges ($78,195 vs. $63,075, p=0.008). Compared to those under 18 years, those aged 18–65 years (aOR 0.61, p=0.003) and over 65 years (aOR 0.34, p< 0.001) had lower odds of ED. Black (aOR 0.36, p< 0.001) and Hispanic (aOR 0.53, p=0.003) patients had lower odds compared to white. The highest income quartile was associated with increased odds (aOR 1.63, p< 0.001) compared to the lowest. Compared to Medicare or Medicaid, private insurance and self-pay (aOR 1.47, p< 0.001) had higher odds of ED. Regarding IBD subtype, Crohn’s disease had a similar prevalence and distribution of ED subtypes compared to Ulcerative colitis. The prevalence of ED showed modest but steady increase, rising from 0.13% in 2016 to 0.17% in 2022.
Discussion: Although ED remain relatively uncommon among IBD patients, their prevalence has shown a gradual rise over the years. ED disproportionately affect younger, white, female IBD patients with higher socioeconomic status and are associated with prolonged hospitalizations and increased resource use. These findings highlight the need for improved psychiatric screening and multidisciplinary management strategies, particularly in high-risk subgroups.
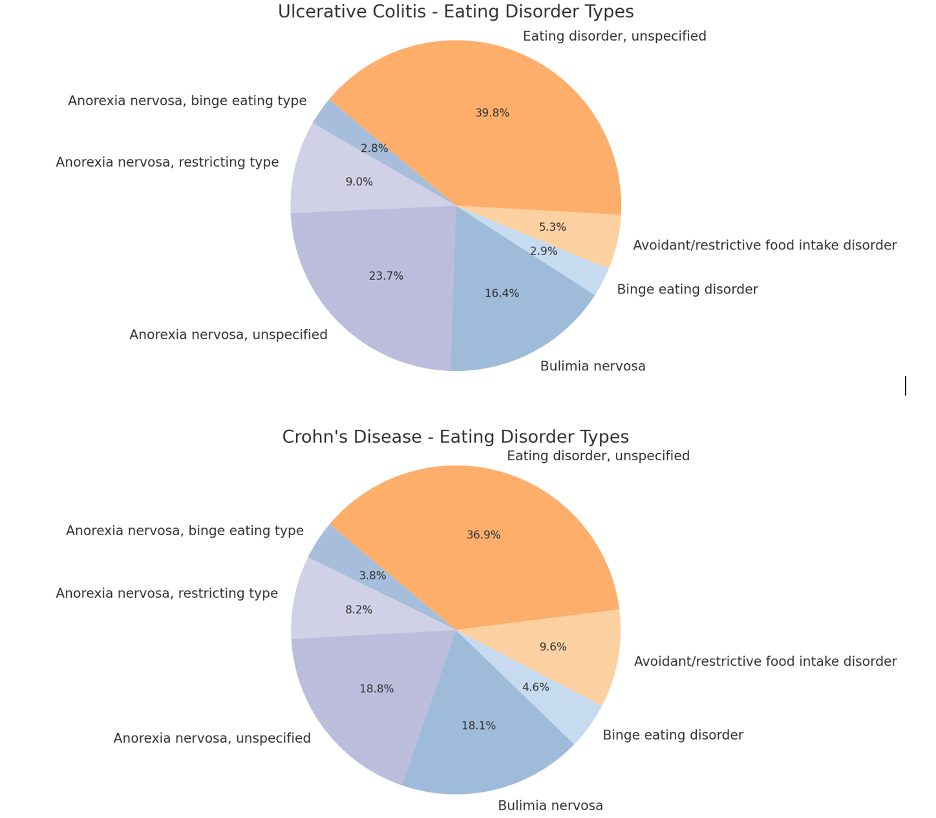
Figure: Table 1. Sociodemographic determinants of Eating Disorders in Inflammatory Bowel Disease.
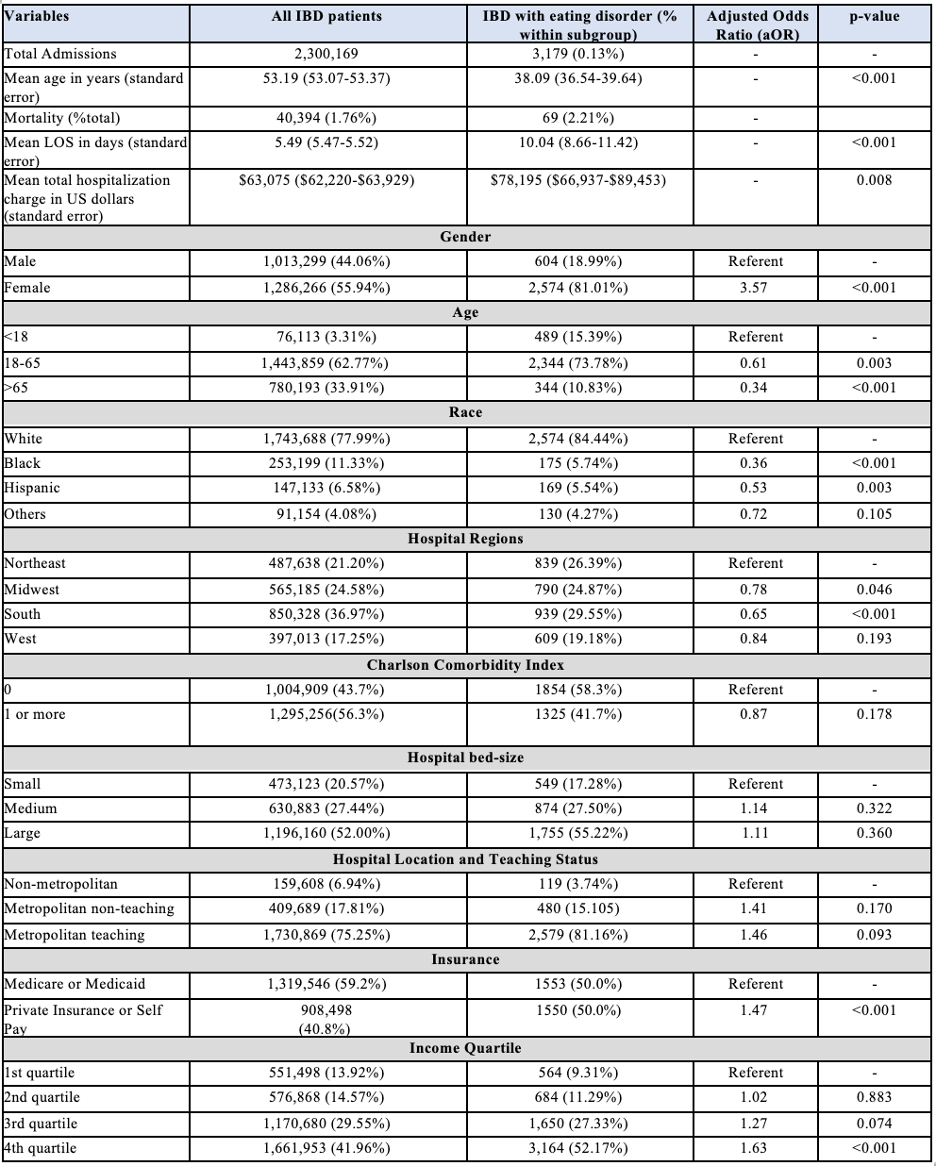
Figure: Figure 1. Distribution of Eating Disorder subtypes among Ulcerative Colitis and Crohn's Disease patients.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Maria Grba indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Gedion Amdetsion indicated no relevant financial relationships.
Kajali Mishra indicated no relevant financial relationships.
Abhin Sapkota, MD1, Maria Grba, MD1, Kriti Katwal, 2, Daniel Guifarro Rivera, MD3, Gedion Amdetsion, MD1, Kajali Mishra, MD4. P1202 - Determinants of Eating Disorders Among Hospitalized Patients With Inflammatory Bowel Disease: A Seven-Year Nationwide Review (2016–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
