Sunday Poster Session
Category: IBD
P1193 - GLP-1 Receptor Agonists Are Associated With Reduced IBD Exacerbations, Hospitalizations, and ER Visits: A Multicenter Observational Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JD
Josue A. Davila, MD (he/him/his)
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Josue A. Davila, MD1, Henry Herrera, BS2, Sherif Saleh, MD1, Nisheet Waghray, MD1
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Case Western Reserve University School of Medicine, Cleveland, OH
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are commonly prescribed for type 2 diabetes and obesity. These agents have demonstrated systemic anti-inflammatory effects and gut-modulating properties. Increasing evidence suggests that GLP-1 RAs may influence IBD activity through weight loss–mediated immune modulation, enhanced intestinal barrier function, and modified gut-brain signaling. However, their clinical impact on IBD exacerbations has not been well studied.
Methods: Using the TriNetX research network, we conducted a retrospective cohort study of adults with Crohn’s disease or ulcerative colitis. Patients who initiated GLP-1 RA therapy after IBD diagnosis were matched 1:1 with non-GLP-1 users based on age, sex, BMI, IBD subtype, diabetes status, immunosuppressant use, and comorbidities (n=16,717 per group). Outcomes assessed over 12 months included (1) IV corticosteroid use, (2) inpatient hospitalization, and (3) emergency department (ED) visits. Risk differences (RD), risk ratios (RR), and odds ratios (OR) were calculated with 95% confidence intervals (CI).
Results: GLP-1 RA use was associated with significantly reduced risk across all measured outcomes. For IV corticosteroids, methylprednisolone was used in 16.5% of GLP-1 users versus 21.3% of non-users (RD −4.8%, RR 0.776, OR 0.731, p< 0.0001); hydrocortisone in 7.5% vs. 10.7% (RD −3.2%, RR 0.702, OR 0.678, p< 0.0001); and dexamethasone in 15.0% vs. 21.8% (RD −6.8%, RR 0.689, OR 0.634, p< 0.0001). Hospitalizations occurred in 15.5% of GLP-1 users versus 36.9% of controls (RD −21.5%, RR 0.419, OR 0.313, p< 0.0001). ED visits were also lower among GLP-1 users (23.5% vs. 31.5%, RD −8.0%, RR 0.746, OR 0.667, p< 0.0001).
Discussion: In this large observational cohort, GLP-1 RA therapy was associated with significantly fewer IBD exacerbation markers, including steroid use, hospitalizations, and ED visits. These findings support a potential protective role of GLP-1 RAs in modifying IBD activity through metabolic and anti-inflammatory pathways. While limited by its retrospective design and potential unmeasured confounding, this study highlights a promising therapeutic intersection between obesity management and chronic gastrointestinal inflammation in a real-life clinical setting, warranting prospective evaluation.
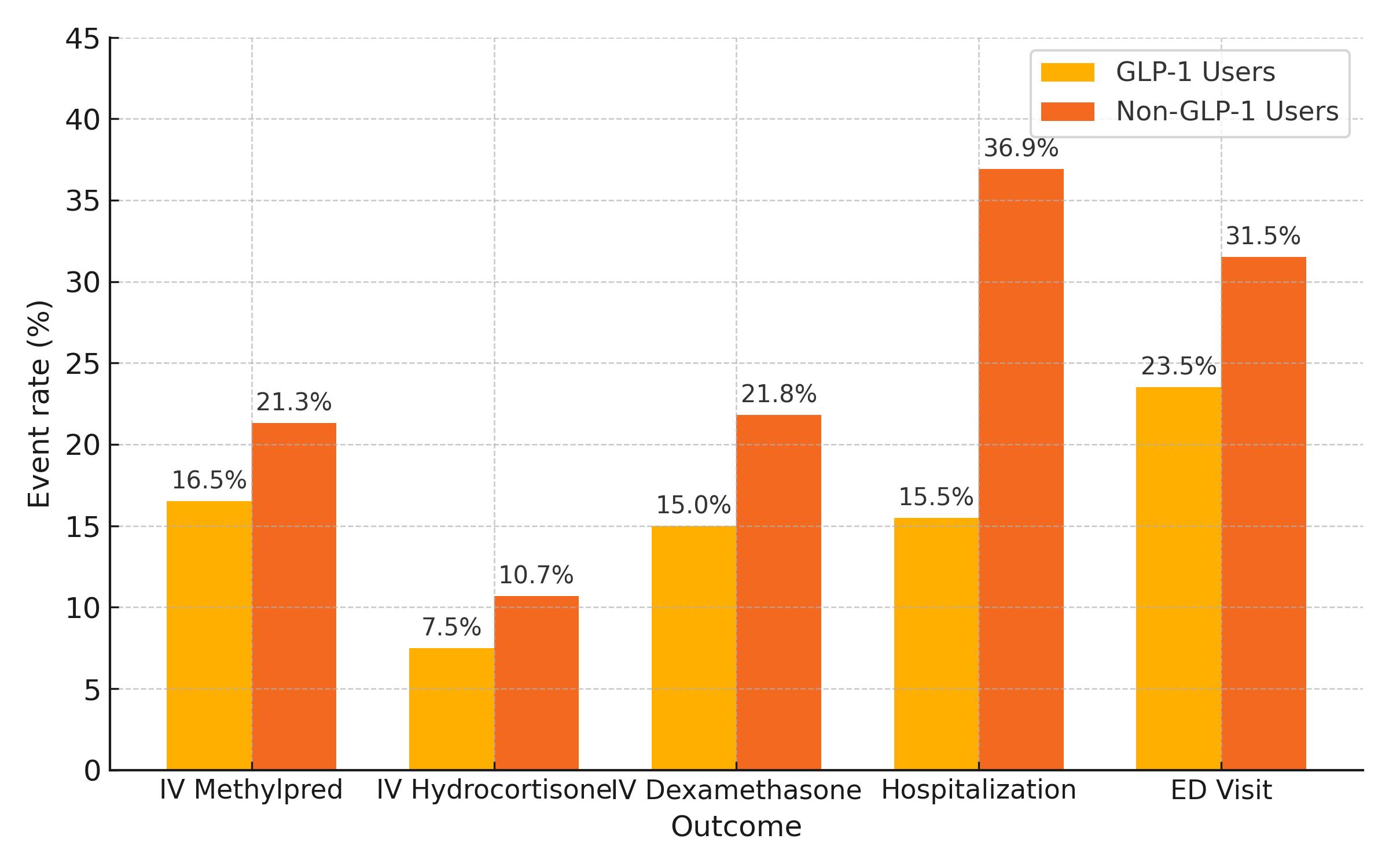
Figure: Comparison of event rates between GLP-1 users and non-users in patients with inflammatory bowel disease, including IV corticosteroid use, hospitalizations, and emergency department visits over 12-month follow-up. All outcomes were significantly lower among GLP-1 users (p < 0.0001 for all comparisons).
Disclosures:
Josue Davila indicated no relevant financial relationships.
Henry Herrera indicated no relevant financial relationships.
Sherif Saleh indicated no relevant financial relationships.
Nisheet Waghray indicated no relevant financial relationships.
Josue A. Davila, MD1, Henry Herrera, BS2, Sherif Saleh, MD1, Nisheet Waghray, MD1. P1193 - GLP-1 Receptor Agonists Are Associated With Reduced IBD Exacerbations, Hospitalizations, and ER Visits: A Multicenter Observational Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Case Western Reserve University School of Medicine, Cleveland, OH
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are commonly prescribed for type 2 diabetes and obesity. These agents have demonstrated systemic anti-inflammatory effects and gut-modulating properties. Increasing evidence suggests that GLP-1 RAs may influence IBD activity through weight loss–mediated immune modulation, enhanced intestinal barrier function, and modified gut-brain signaling. However, their clinical impact on IBD exacerbations has not been well studied.
Methods: Using the TriNetX research network, we conducted a retrospective cohort study of adults with Crohn’s disease or ulcerative colitis. Patients who initiated GLP-1 RA therapy after IBD diagnosis were matched 1:1 with non-GLP-1 users based on age, sex, BMI, IBD subtype, diabetes status, immunosuppressant use, and comorbidities (n=16,717 per group). Outcomes assessed over 12 months included (1) IV corticosteroid use, (2) inpatient hospitalization, and (3) emergency department (ED) visits. Risk differences (RD), risk ratios (RR), and odds ratios (OR) were calculated with 95% confidence intervals (CI).
Results: GLP-1 RA use was associated with significantly reduced risk across all measured outcomes. For IV corticosteroids, methylprednisolone was used in 16.5% of GLP-1 users versus 21.3% of non-users (RD −4.8%, RR 0.776, OR 0.731, p< 0.0001); hydrocortisone in 7.5% vs. 10.7% (RD −3.2%, RR 0.702, OR 0.678, p< 0.0001); and dexamethasone in 15.0% vs. 21.8% (RD −6.8%, RR 0.689, OR 0.634, p< 0.0001). Hospitalizations occurred in 15.5% of GLP-1 users versus 36.9% of controls (RD −21.5%, RR 0.419, OR 0.313, p< 0.0001). ED visits were also lower among GLP-1 users (23.5% vs. 31.5%, RD −8.0%, RR 0.746, OR 0.667, p< 0.0001).
Discussion: In this large observational cohort, GLP-1 RA therapy was associated with significantly fewer IBD exacerbation markers, including steroid use, hospitalizations, and ED visits. These findings support a potential protective role of GLP-1 RAs in modifying IBD activity through metabolic and anti-inflammatory pathways. While limited by its retrospective design and potential unmeasured confounding, this study highlights a promising therapeutic intersection between obesity management and chronic gastrointestinal inflammation in a real-life clinical setting, warranting prospective evaluation.
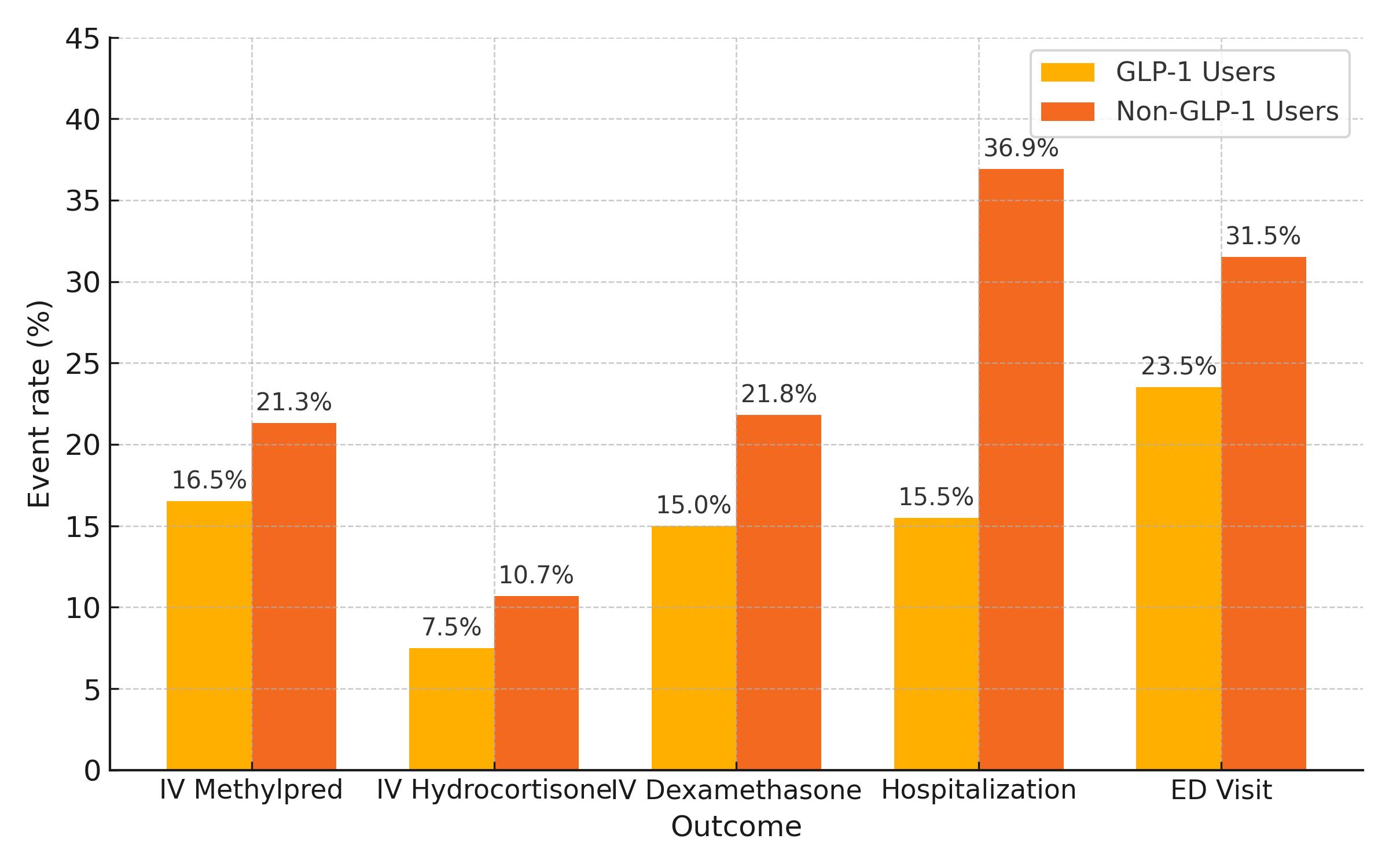
Figure: Comparison of event rates between GLP-1 users and non-users in patients with inflammatory bowel disease, including IV corticosteroid use, hospitalizations, and emergency department visits over 12-month follow-up. All outcomes were significantly lower among GLP-1 users (p < 0.0001 for all comparisons).
Disclosures:
Josue Davila indicated no relevant financial relationships.
Henry Herrera indicated no relevant financial relationships.
Sherif Saleh indicated no relevant financial relationships.
Nisheet Waghray indicated no relevant financial relationships.
Josue A. Davila, MD1, Henry Herrera, BS2, Sherif Saleh, MD1, Nisheet Waghray, MD1. P1193 - GLP-1 Receptor Agonists Are Associated With Reduced IBD Exacerbations, Hospitalizations, and ER Visits: A Multicenter Observational Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
