Sunday Poster Session
Category: IBD
P1185 - Exploring the Association Between IgA Vasculitis and Inflammatory Bowel Disease: A Systematic Review
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- HS
Haruki Sawada, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Haruki Sawada, MD1, Yoshito Nishimura, MD, PhD, MPH2, Ko Takamatsu, MD3, Edward Nguyen, MD3, Takahashi Takahashi, MD3, Kinanah Yaseen, MD1, Katherine Falloon, MD1, Florian Rieder, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2Mayo Clinic, Rochester, MN; 3University of Hawaii, John A. Burns School of Medicine, Honolulu, HI
Introduction: IgA vasculitis (IgAV) is a rare small-vessel vasculitis which was reported in adults with inflammatory bowel disease (IBD). Recent observations suggest IgAV may occur as an extraintestinal manifestation of IBD or as an adverse reaction to IBD therapies. We aimed to systematically review the literature to characterize the relationship between IBD and IgAV.
Methods: A comprehensive search of MEDLINE, EMBASE, and Web of Science was conducted to identify peer-reviewed reports of coexisting IBD and IgAV in adults. Two reviewers independently screened and selected studies. Data on clinical features, temporal sequence of IBD and IgAV, treatments, and outcomes were extracted. We also noted any associations with IBD medications.
Results: Seventeen relevant publications were identified, comprising three retrospective cohort studies and 14 single-patient case reports for a total of 66 patients with concomitant IBD and IgAV. In two observational cohorts, IBD preceded the onset of IgAV in 88% and 100% of patients, with median intervals of 9.2 and 17.3 years, respectively. All patients presented with skin involvement. IgAV developed during TNF-α inhibitor (TNFi) therapy in 74% and 67% of patients in the respective cohorts. Rechallenge with TNFi resulted in relapse in 67% of these cases. A Mendelian randomization study demonstrated a modest but significant genetic association between IBD and IgAV (OR 1.20; 95%CI: 1.07–1.36). Among the 14 individual case reports (mean age 44.6 years), all patients exhibited skin involvement, with renal (71%) and joint (64%) involvement also frequently reported. IgA deposition was confirmed in 9 of 12 biopsy-proven cases. Nine patients (64%) were receiving TNFi at the time of vasculitis onset; additional cases involved vedolizumab (n = 2) and ustekinumab (n = 1). Management frequently included discontinuation of the suspected biologic. Rechallenge with TNFi led to relapse in 4 of 5 cases (80%), whereas switching to a different class of biologic agents was generally well tolerated.
Discussion: IgAV, though uncommon, appears to be an under-recognized extraintestinal manifestation in patients with IBD. It may emerge independently as part of the extraintestinal spectrum of IBD or be triggered by IBD medications, in particular biologics like TNFi. Clinicians should remain vigilant for new-onset vasculitic symptoms in IBD patients. Further research is needed to clarify shared pathophysiological mechanisms and to guide clinical management.
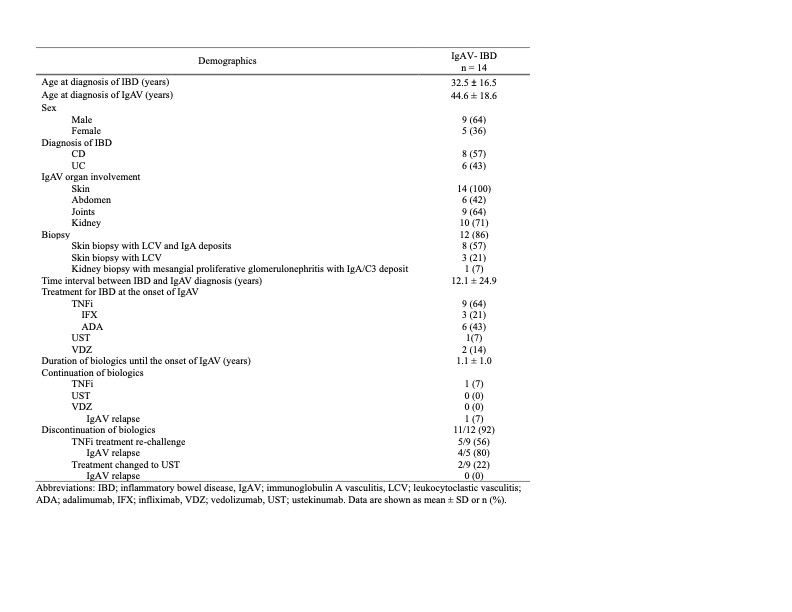
Figure: Table 1. Demographic Features of Patients with IBD and IgAV from Observational Studies
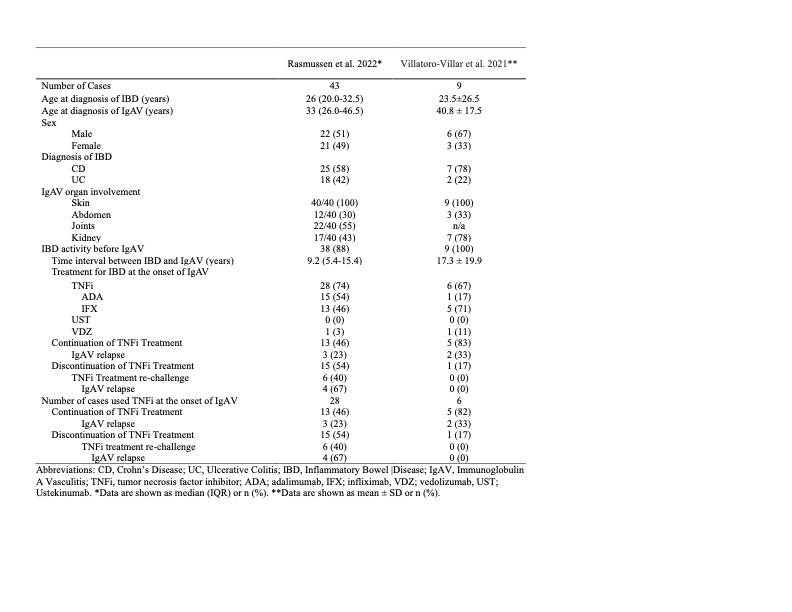
Figure: Table 2. Demographic Features of Patients with IBD and IgAV in Published Reports
Disclosures:
Haruki Sawada indicated no relevant financial relationships.
Yoshito Nishimura indicated no relevant financial relationships.
Ko Takamatsu indicated no relevant financial relationships.
Edward Nguyen indicated no relevant financial relationships.
Takahashi Takahashi indicated no relevant financial relationships.
Kinanah Yaseen indicated no relevant financial relationships.
Katherine Falloon: Cardinal Health, Inc. – Husband is employee. Janssen Pharmaceuticals, Inc. – Consultant. MD Education – Speaker. Pfizer – Grant/Research Support. Takeda Pharmaceuticals, Inc. – Speaker.
Florian Rieder: Adiso – Advisory Committee/Board Member, Consultant. Adnovate, Agomab, Allergan, AbbVie, Arena, Astra Zeneca, Bausch & Lomb, Boehringer-Ingelheim, Celgene/BMS, Celltrion, CDISC, Celsius, Cowen, 89Bio – Advisory Committee/Board Member, Consultant. Eugit, Ferring, Galapagos, Galmed, Genentech, Gilead, Gossamer, Granite, Guidepoint, Helmsley, Horizon Therapeutics, Image Analysis Limited – Advisory Committee/Board Member, Consultant. Landos, Jannsen, Koutif, Mestag, Metacrine, Mirum, Mobius, Mopac, Morphic, Myka Labs, Organovo, Origo, Palisade, Pfizer, Pliant, Prometheus Bioscience – Advisory Committee/Board Member, Consultant. Receptos, RedX, Roche, Samsung, Sanofi, Surmodics, Surrozen, Takeda, Techlab, Teva, Theravance, Thetis, Tr1x Bio, UCB, Ysios – Advisory Committee/Board Member, Consultant.
Haruki Sawada, MD1, Yoshito Nishimura, MD, PhD, MPH2, Ko Takamatsu, MD3, Edward Nguyen, MD3, Takahashi Takahashi, MD3, Kinanah Yaseen, MD1, Katherine Falloon, MD1, Florian Rieder, MD1. P1185 - Exploring the Association Between IgA Vasculitis and Inflammatory Bowel Disease: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Mayo Clinic, Rochester, MN; 3University of Hawaii, John A. Burns School of Medicine, Honolulu, HI
Introduction: IgA vasculitis (IgAV) is a rare small-vessel vasculitis which was reported in adults with inflammatory bowel disease (IBD). Recent observations suggest IgAV may occur as an extraintestinal manifestation of IBD or as an adverse reaction to IBD therapies. We aimed to systematically review the literature to characterize the relationship between IBD and IgAV.
Methods: A comprehensive search of MEDLINE, EMBASE, and Web of Science was conducted to identify peer-reviewed reports of coexisting IBD and IgAV in adults. Two reviewers independently screened and selected studies. Data on clinical features, temporal sequence of IBD and IgAV, treatments, and outcomes were extracted. We also noted any associations with IBD medications.
Results: Seventeen relevant publications were identified, comprising three retrospective cohort studies and 14 single-patient case reports for a total of 66 patients with concomitant IBD and IgAV. In two observational cohorts, IBD preceded the onset of IgAV in 88% and 100% of patients, with median intervals of 9.2 and 17.3 years, respectively. All patients presented with skin involvement. IgAV developed during TNF-α inhibitor (TNFi) therapy in 74% and 67% of patients in the respective cohorts. Rechallenge with TNFi resulted in relapse in 67% of these cases. A Mendelian randomization study demonstrated a modest but significant genetic association between IBD and IgAV (OR 1.20; 95%CI: 1.07–1.36). Among the 14 individual case reports (mean age 44.6 years), all patients exhibited skin involvement, with renal (71%) and joint (64%) involvement also frequently reported. IgA deposition was confirmed in 9 of 12 biopsy-proven cases. Nine patients (64%) were receiving TNFi at the time of vasculitis onset; additional cases involved vedolizumab (n = 2) and ustekinumab (n = 1). Management frequently included discontinuation of the suspected biologic. Rechallenge with TNFi led to relapse in 4 of 5 cases (80%), whereas switching to a different class of biologic agents was generally well tolerated.
Discussion: IgAV, though uncommon, appears to be an under-recognized extraintestinal manifestation in patients with IBD. It may emerge independently as part of the extraintestinal spectrum of IBD or be triggered by IBD medications, in particular biologics like TNFi. Clinicians should remain vigilant for new-onset vasculitic symptoms in IBD patients. Further research is needed to clarify shared pathophysiological mechanisms and to guide clinical management.
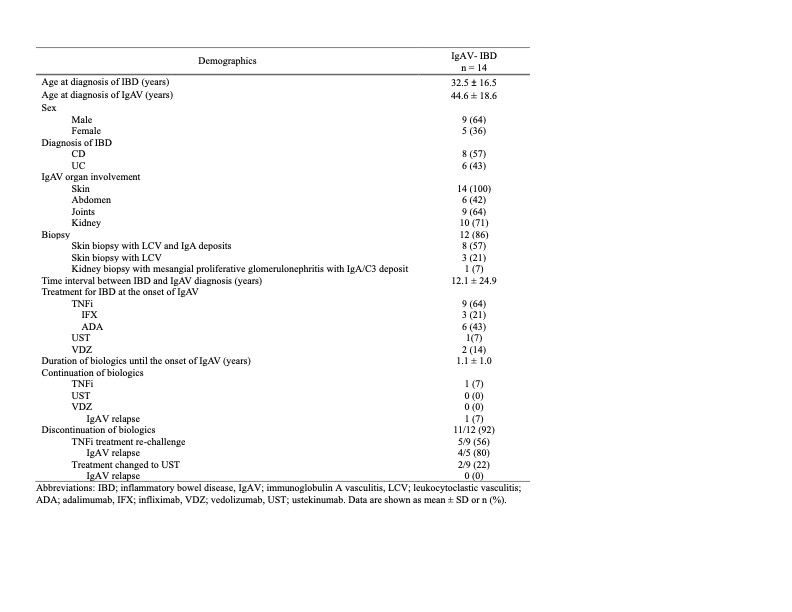
Figure: Table 1. Demographic Features of Patients with IBD and IgAV from Observational Studies
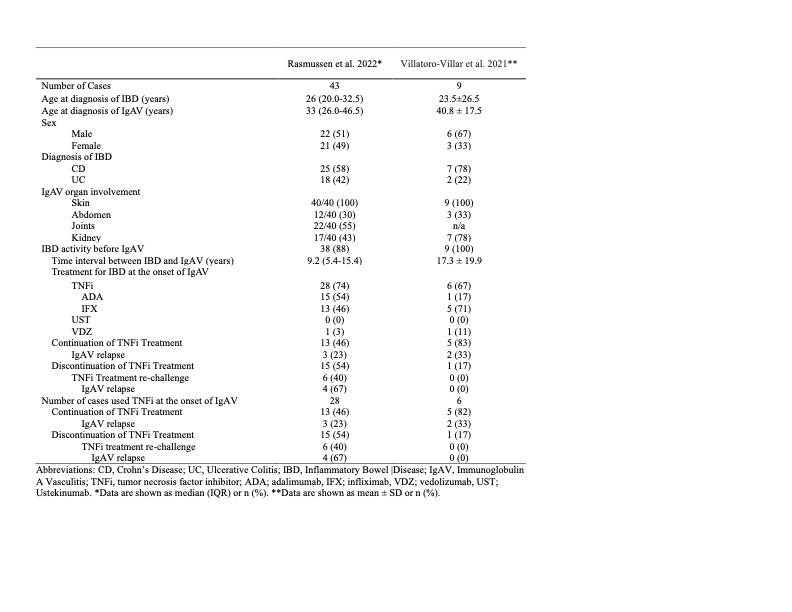
Figure: Table 2. Demographic Features of Patients with IBD and IgAV in Published Reports
Disclosures:
Haruki Sawada indicated no relevant financial relationships.
Yoshito Nishimura indicated no relevant financial relationships.
Ko Takamatsu indicated no relevant financial relationships.
Edward Nguyen indicated no relevant financial relationships.
Takahashi Takahashi indicated no relevant financial relationships.
Kinanah Yaseen indicated no relevant financial relationships.
Katherine Falloon: Cardinal Health, Inc. – Husband is employee. Janssen Pharmaceuticals, Inc. – Consultant. MD Education – Speaker. Pfizer – Grant/Research Support. Takeda Pharmaceuticals, Inc. – Speaker.
Florian Rieder: Adiso – Advisory Committee/Board Member, Consultant. Adnovate, Agomab, Allergan, AbbVie, Arena, Astra Zeneca, Bausch & Lomb, Boehringer-Ingelheim, Celgene/BMS, Celltrion, CDISC, Celsius, Cowen, 89Bio – Advisory Committee/Board Member, Consultant. Eugit, Ferring, Galapagos, Galmed, Genentech, Gilead, Gossamer, Granite, Guidepoint, Helmsley, Horizon Therapeutics, Image Analysis Limited – Advisory Committee/Board Member, Consultant. Landos, Jannsen, Koutif, Mestag, Metacrine, Mirum, Mobius, Mopac, Morphic, Myka Labs, Organovo, Origo, Palisade, Pfizer, Pliant, Prometheus Bioscience – Advisory Committee/Board Member, Consultant. Receptos, RedX, Roche, Samsung, Sanofi, Surmodics, Surrozen, Takeda, Techlab, Teva, Theravance, Thetis, Tr1x Bio, UCB, Ysios – Advisory Committee/Board Member, Consultant.
Haruki Sawada, MD1, Yoshito Nishimura, MD, PhD, MPH2, Ko Takamatsu, MD3, Edward Nguyen, MD3, Takahashi Takahashi, MD3, Kinanah Yaseen, MD1, Katherine Falloon, MD1, Florian Rieder, MD1. P1185 - Exploring the Association Between IgA Vasculitis and Inflammatory Bowel Disease: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
