Sunday Poster Session
Category: IBD
P1184 - Role of Fecal Myeloperoxidase (fMPO) in Patients With Ulcerative Colitis: A Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Megha R. Joshi, MBBS (she/her/hers)
Bellevue Hospital Center
Brooklyn, NY
Presenting Author(s)
Megha Joshi, MBBS1, Naga Vamsi Krishna Machineni, MD2, Pavana Appala, MBBS3, Sonali Dash, BS4, Tarika Walia, MBBS5, Siri Gottipati, 6, Tejeswara Rao Pydi, MBBS7, Rupak Desai, MBBS8
1Bellevue Hospital Center, New York, NY; 2Appalachian Regional Healthcare, Harlan, KY; 3Kasturba Medical College, Cumming, GA; 4Johns Hopkins University, Baltimore, MD; 5Raikhi Hospital Patiala, Patiala, Punjab, India; 6Glenelg High School, Glenelg, MD; 7Osmania medical college, Hyderabad, Telangana, India; 8Independent Outcomes Researcher, Atlanta, GA
Introduction: Ulcerative Colitis is a chronic inflammatory disease, mainly affecting the rectal mucosa of young adults (15-30 years) and geriatric population (50-70 years). Infiltrating neutrophils play a major role in mucosal inflammation, by releasing their products into the rectal lumen. Fecal myeloperoxidase (fMPO), fecal calprotectin (fcal), fecal lactoferrin (fLF), eosinophil-derived neurotoxin, and human neutrophil lipocalin (HNL) are some of the recognized neutrophil outputs that have served as valuable markers of inflammation. Noninvasive methods of disease diagnosis, staging, and treatment response monitoring often report increased patient adherence and decreased costs, demonstrating their significance in improved quality of care as compared to repeat invasive procedures.
We aim to establish the comparative diagnostic and prognosis efficacy of fecal myeloperoxidase in ulcerative colitis via this meta-analysis of published literature.
Methods: We utilized Google Scholar, and PubMed databases for studies published and conducted during 2015-2025. ‘Fecal myeloperoxidase’, ‘fecal biomarkers’, ‘ulcerative colitis’, ‘randomized control trials’, and ‘inflammatory bowel disease’ were our core search values. Studies were included if they showed comparative efficacies of different fecal biomarkers in the diagnosis, staging, and treatment response monitoring of patients with ulcerative colitis. We pooled data from the result tables of qualifying studies (mainly randomized controlled trials) to generate results.
Results: We pooled data from 10 qualifying studies, with a total of 491 UC patients included in the final analysis. Elevated fMPO (Mann Whitney U tests) are linked to relapse and severe disease activity in UC, correlating with advanced stages (3/4) as observed in endoscopic and histological assessments. fMPO (SN:77%, SP:77.2%) and fCal (SN: 75.2%, SP: 82.8%) outperformed HNL pAb/765 (SN: 62.3%, SP: 89.6%), HNL 763/764 (SN: 60.3%, SP: 88.1%), ECP(SN: 75.3%, SP: 73.1%), Tryptase, IL-1β, CRP(SN: 65.5%, SP: 67%), EPX, and EDN(SN: 64.9%, SP: 71.6%) in their associations with disease severity and consequent response to treatment. Three other studies also noted similar results over 12-24 months.
Discussion: fMPO is a highly specific non-invasive, promising tool capable of adding to the diagnostic and prognostic power of other fecal biomarkers for ulcerative colitis. Larger clinical trials with standardized protocols are needed to establish diagnostic threshold values for fMPO in ulcerative colitis.
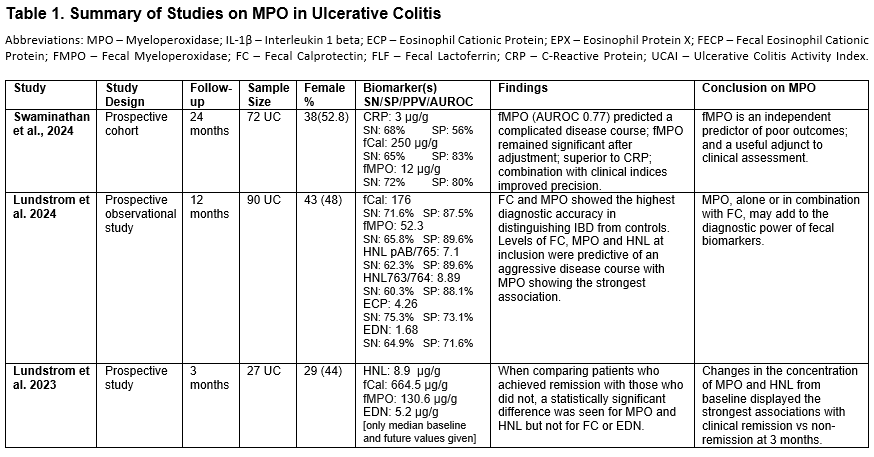
Figure: Table summary of studies on fMPO in Ulcerative Colitis- 1
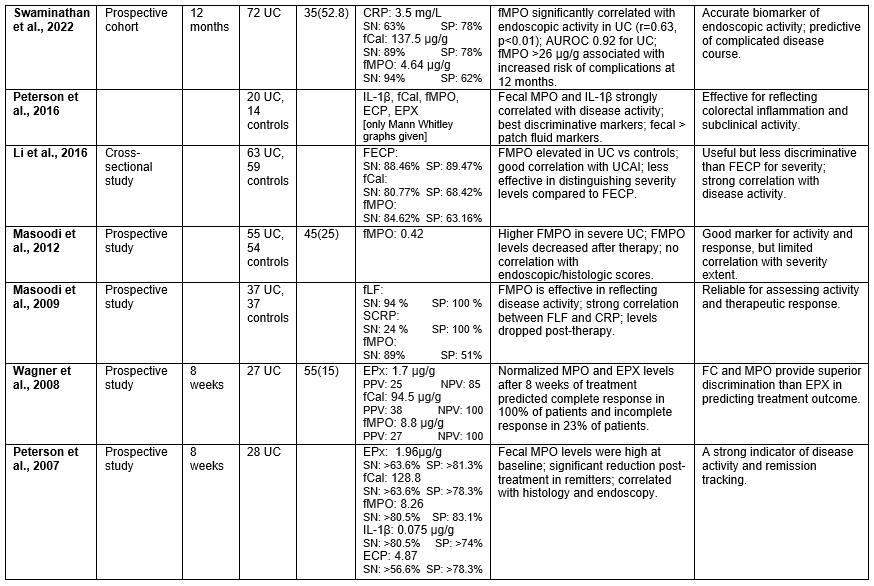
Figure: Table summary of studies on fMPO in Ulcerative Colitis- 2
Disclosures:
Megha Joshi indicated no relevant financial relationships.
Naga Vamsi Krishna Machineni indicated no relevant financial relationships.
Pavana Appala indicated no relevant financial relationships.
Sonali Dash indicated no relevant financial relationships.
Tarika Walia indicated no relevant financial relationships.
Siri Gottipati indicated no relevant financial relationships.
Tejeswara Rao Pydi indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Megha Joshi, MBBS1, Naga Vamsi Krishna Machineni, MD2, Pavana Appala, MBBS3, Sonali Dash, BS4, Tarika Walia, MBBS5, Siri Gottipati, 6, Tejeswara Rao Pydi, MBBS7, Rupak Desai, MBBS8. P1184 - Role of Fecal Myeloperoxidase (fMPO) in Patients With Ulcerative Colitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Bellevue Hospital Center, New York, NY; 2Appalachian Regional Healthcare, Harlan, KY; 3Kasturba Medical College, Cumming, GA; 4Johns Hopkins University, Baltimore, MD; 5Raikhi Hospital Patiala, Patiala, Punjab, India; 6Glenelg High School, Glenelg, MD; 7Osmania medical college, Hyderabad, Telangana, India; 8Independent Outcomes Researcher, Atlanta, GA
Introduction: Ulcerative Colitis is a chronic inflammatory disease, mainly affecting the rectal mucosa of young adults (15-30 years) and geriatric population (50-70 years). Infiltrating neutrophils play a major role in mucosal inflammation, by releasing their products into the rectal lumen. Fecal myeloperoxidase (fMPO), fecal calprotectin (fcal), fecal lactoferrin (fLF), eosinophil-derived neurotoxin, and human neutrophil lipocalin (HNL) are some of the recognized neutrophil outputs that have served as valuable markers of inflammation. Noninvasive methods of disease diagnosis, staging, and treatment response monitoring often report increased patient adherence and decreased costs, demonstrating their significance in improved quality of care as compared to repeat invasive procedures.
We aim to establish the comparative diagnostic and prognosis efficacy of fecal myeloperoxidase in ulcerative colitis via this meta-analysis of published literature.
Methods: We utilized Google Scholar, and PubMed databases for studies published and conducted during 2015-2025. ‘Fecal myeloperoxidase’, ‘fecal biomarkers’, ‘ulcerative colitis’, ‘randomized control trials’, and ‘inflammatory bowel disease’ were our core search values. Studies were included if they showed comparative efficacies of different fecal biomarkers in the diagnosis, staging, and treatment response monitoring of patients with ulcerative colitis. We pooled data from the result tables of qualifying studies (mainly randomized controlled trials) to generate results.
Results: We pooled data from 10 qualifying studies, with a total of 491 UC patients included in the final analysis. Elevated fMPO (Mann Whitney U tests) are linked to relapse and severe disease activity in UC, correlating with advanced stages (3/4) as observed in endoscopic and histological assessments. fMPO (SN:77%, SP:77.2%) and fCal (SN: 75.2%, SP: 82.8%) outperformed HNL pAb/765 (SN: 62.3%, SP: 89.6%), HNL 763/764 (SN: 60.3%, SP: 88.1%), ECP(SN: 75.3%, SP: 73.1%), Tryptase, IL-1β, CRP(SN: 65.5%, SP: 67%), EPX, and EDN(SN: 64.9%, SP: 71.6%) in their associations with disease severity and consequent response to treatment. Three other studies also noted similar results over 12-24 months.
Discussion: fMPO is a highly specific non-invasive, promising tool capable of adding to the diagnostic and prognostic power of other fecal biomarkers for ulcerative colitis. Larger clinical trials with standardized protocols are needed to establish diagnostic threshold values for fMPO in ulcerative colitis.
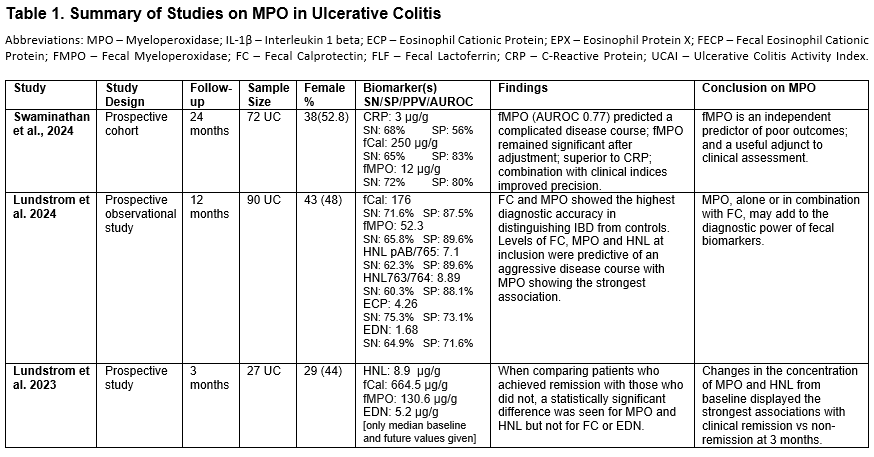
Figure: Table summary of studies on fMPO in Ulcerative Colitis- 1
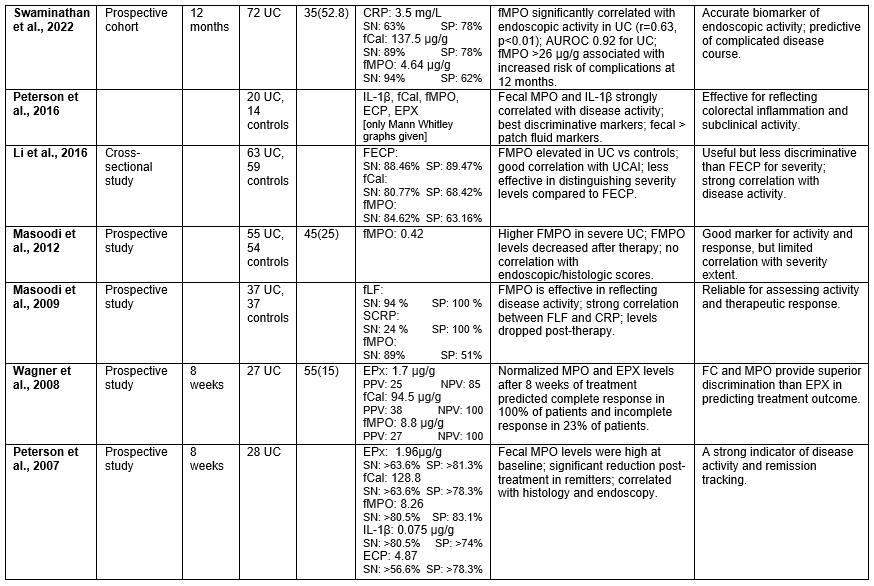
Figure: Table summary of studies on fMPO in Ulcerative Colitis- 2
Disclosures:
Megha Joshi indicated no relevant financial relationships.
Naga Vamsi Krishna Machineni indicated no relevant financial relationships.
Pavana Appala indicated no relevant financial relationships.
Sonali Dash indicated no relevant financial relationships.
Tarika Walia indicated no relevant financial relationships.
Siri Gottipati indicated no relevant financial relationships.
Tejeswara Rao Pydi indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Megha Joshi, MBBS1, Naga Vamsi Krishna Machineni, MD2, Pavana Appala, MBBS3, Sonali Dash, BS4, Tarika Walia, MBBS5, Siri Gottipati, 6, Tejeswara Rao Pydi, MBBS7, Rupak Desai, MBBS8. P1184 - Role of Fecal Myeloperoxidase (fMPO) in Patients With Ulcerative Colitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
