Sunday Poster Session
Category: IBD
P1136 - Comparative Risk of Infection-Related Hospitalization With Infliximab, Vedolizumab, and Ustekinumab in Elderly Inflammatory Bowel Disease: A Propensity-Score–Matched
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Abdallah Hussein, MD (he/him/his)
Virtua Our Lady of Lourdes Hospital
Camden, NJ
Presenting Author(s)
Abdallah Hussein, MD1, Islam Rajab, MD2, Toni Elias, DO3, Ahmed Salem, MD4, Mohammed Abu-Rumaileh, MD5, Ibrahim Shanti, MD6, Elaf Khatib, MS7, Yecheskel Schneider, MD, MS8
1Virtua Our Lady of Lourdes Hospital, Camden, NJ; 2St. Joseph's University Medical Center, Paterson, NJ; 3Rowan-Virtua School of Osteopathic Medicine, Camden, NJ; 4Maimonides Medical Center, Brooklyn, NY; 5The University of Toledo, Toledo, OH; 6Marshall University - - Huntington, WV, Huntington, WV; 7Thomas Jefferson University, Philadelphia, PA; 8Virtua Health System, Moorestown, NJ
Introduction: Managing inflammatory bowel disease (IBD) in older adults is challenging, as immunosenescence and comorbidities elevate the risk of serious infections. Although tumor necrosis factor-α antagonists (e.g., infliximab) remain a mainstay of therapy, newer gut-targeted agents such as vedolizumab and ustekinumab may offer improved safety in this vulnerable population. Yet, real-world, head-to-head data on infection-related hospitalization among elderly IBD patients are limited. This study therefore leveraged the global TriNetX Collaborative Network to compare six-month hospitalization risks across these three biologic classes in patients aged ≥ 60 years.
Methods: This retrospective cohort study utilized data from the global TriNetX Collaborative Network to identify patients aged ≥ 60 years with inflammatory bowel disease who newly initiated infliximab, vedolizumab, or ustekinumab between January 1, 2015, and December 31, 2024. The primary outcome was infection-related hospitalization within six months of treatment initiation. Three comparisons were performed: vedolizumab versus infliximab, ustekinumab versus infliximab, and vedolizumab versus ustekinumab. Propensity-score matching was used to balance baseline characteristics across treatment groups. We calculated univariable risk ratios with 95% confidence intervals to compare hospitalization risk in each matched cohort. Baseline characteristics are summarized in Table 1.
Results: In propensity‐score–matched cohorts, infection‐related hospitalization was significantly lower with both vedolizumab and ustekinumab compared with infliximab, but did not differ between vedolizumab and ustekinumab. Specifically, among 3,283 matched patients per arm, vedolizumab was associated with a 10.97 % hospitalization rate versus 15.90 % for infliximab (RR 0.69, 95 % CI 0.61–0.78; P < 0.0001). Similarly, in 2,918 patients per arm, ustekinumab yielded a 9.70 % rate versus 13.88 % with infliximab (RR 0.70, 95 % CI 0.61-0.78; P < 0.0001). In the head‐to‐head comparison of vedolizumab (n = 2,497) and ustekinumab (n = 2,497), hospitalization occurred in 10.77 % versus 9.49 %, respectively (RR 1.14, 95 % CI 0.96–1.34; P = 0.13).
Discussion: vedolizumab and ustekinumab were each associated with significantly lower hazards of key infection‐related hospitalizations—particularly lower respiratory and urinary tract infections, C. difficile enterocolitis, and all‐cause mortality—compared with infliximab in patients ≥ 60 years.
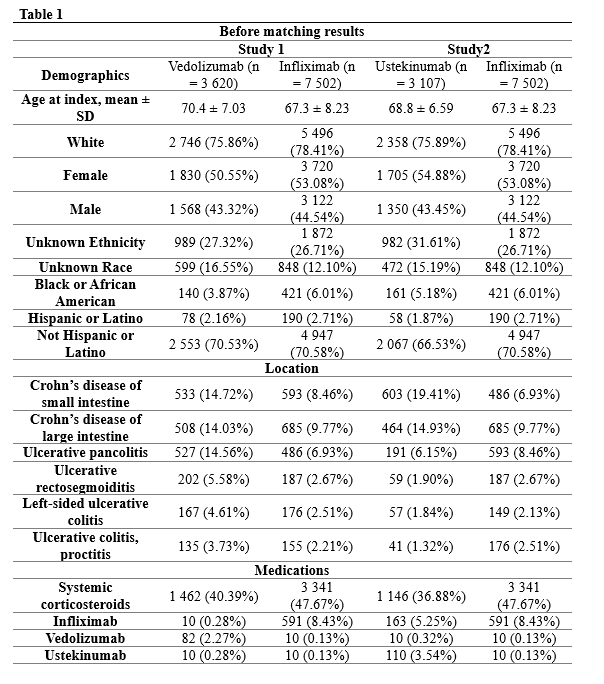
Figure: Table 1 Baseline Charectristics
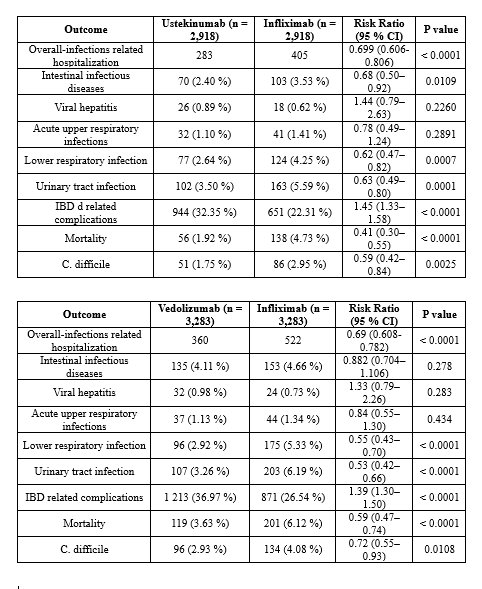
Figure: Outcomes
Disclosures:
Abdallah Hussein indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Toni Elias indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Mohammed Abu-Rumaileh indicated no relevant financial relationships.
Ibrahim Shanti indicated no relevant financial relationships.
Elaf Khatib indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Abdallah Hussein, MD1, Islam Rajab, MD2, Toni Elias, DO3, Ahmed Salem, MD4, Mohammed Abu-Rumaileh, MD5, Ibrahim Shanti, MD6, Elaf Khatib, MS7, Yecheskel Schneider, MD, MS8. P1136 - Comparative Risk of Infection-Related Hospitalization With Infliximab, Vedolizumab, and Ustekinumab in Elderly Inflammatory Bowel Disease: A Propensity-Score–Matched, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Virtua Our Lady of Lourdes Hospital, Camden, NJ; 2St. Joseph's University Medical Center, Paterson, NJ; 3Rowan-Virtua School of Osteopathic Medicine, Camden, NJ; 4Maimonides Medical Center, Brooklyn, NY; 5The University of Toledo, Toledo, OH; 6Marshall University - - Huntington, WV, Huntington, WV; 7Thomas Jefferson University, Philadelphia, PA; 8Virtua Health System, Moorestown, NJ
Introduction: Managing inflammatory bowel disease (IBD) in older adults is challenging, as immunosenescence and comorbidities elevate the risk of serious infections. Although tumor necrosis factor-α antagonists (e.g., infliximab) remain a mainstay of therapy, newer gut-targeted agents such as vedolizumab and ustekinumab may offer improved safety in this vulnerable population. Yet, real-world, head-to-head data on infection-related hospitalization among elderly IBD patients are limited. This study therefore leveraged the global TriNetX Collaborative Network to compare six-month hospitalization risks across these three biologic classes in patients aged ≥ 60 years.
Methods: This retrospective cohort study utilized data from the global TriNetX Collaborative Network to identify patients aged ≥ 60 years with inflammatory bowel disease who newly initiated infliximab, vedolizumab, or ustekinumab between January 1, 2015, and December 31, 2024. The primary outcome was infection-related hospitalization within six months of treatment initiation. Three comparisons were performed: vedolizumab versus infliximab, ustekinumab versus infliximab, and vedolizumab versus ustekinumab. Propensity-score matching was used to balance baseline characteristics across treatment groups. We calculated univariable risk ratios with 95% confidence intervals to compare hospitalization risk in each matched cohort. Baseline characteristics are summarized in Table 1.
Results: In propensity‐score–matched cohorts, infection‐related hospitalization was significantly lower with both vedolizumab and ustekinumab compared with infliximab, but did not differ between vedolizumab and ustekinumab. Specifically, among 3,283 matched patients per arm, vedolizumab was associated with a 10.97 % hospitalization rate versus 15.90 % for infliximab (RR 0.69, 95 % CI 0.61–0.78; P < 0.0001). Similarly, in 2,918 patients per arm, ustekinumab yielded a 9.70 % rate versus 13.88 % with infliximab (RR 0.70, 95 % CI 0.61-0.78; P < 0.0001). In the head‐to‐head comparison of vedolizumab (n = 2,497) and ustekinumab (n = 2,497), hospitalization occurred in 10.77 % versus 9.49 %, respectively (RR 1.14, 95 % CI 0.96–1.34; P = 0.13).
Discussion: vedolizumab and ustekinumab were each associated with significantly lower hazards of key infection‐related hospitalizations—particularly lower respiratory and urinary tract infections, C. difficile enterocolitis, and all‐cause mortality—compared with infliximab in patients ≥ 60 years.
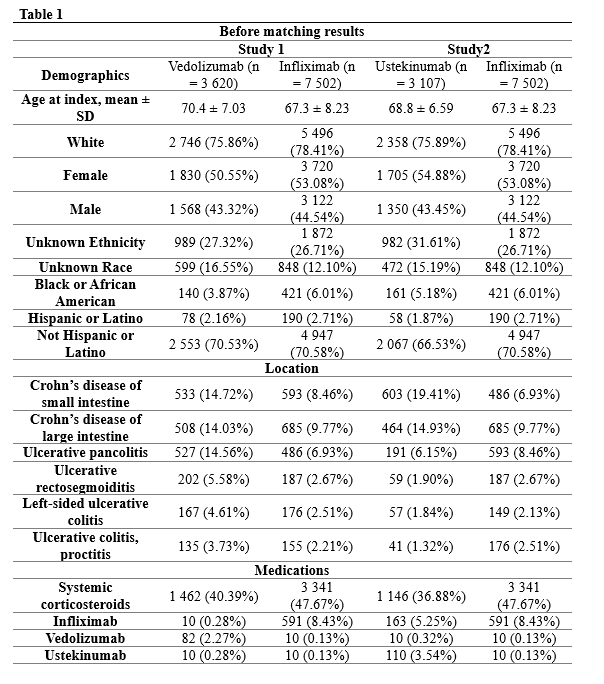
Figure: Table 1 Baseline Charectristics
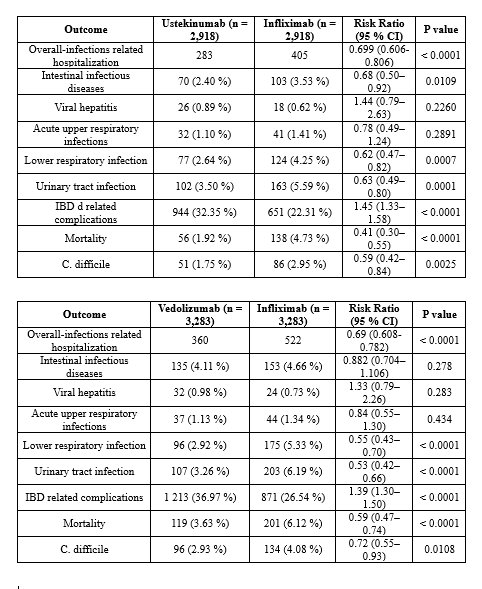
Figure: Outcomes
Disclosures:
Abdallah Hussein indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Toni Elias indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Mohammed Abu-Rumaileh indicated no relevant financial relationships.
Ibrahim Shanti indicated no relevant financial relationships.
Elaf Khatib indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Abdallah Hussein, MD1, Islam Rajab, MD2, Toni Elias, DO3, Ahmed Salem, MD4, Mohammed Abu-Rumaileh, MD5, Ibrahim Shanti, MD6, Elaf Khatib, MS7, Yecheskel Schneider, MD, MS8. P1136 - Comparative Risk of Infection-Related Hospitalization With Infliximab, Vedolizumab, and Ustekinumab in Elderly Inflammatory Bowel Disease: A Propensity-Score–Matched, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
